Monday Poster Session
Category: Biliary/Pancreas
P2277 - Primary Pancreatic Follicular Lymphoma: A Rare Incidental Finding During Evaluation for GI Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Lefika Bathobakae, MD, MPH
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Lefika Bathobakae, MD, MPH1, Dina Rohira, MD2, Tasnim Fatima, MD1, Rammy Bashir, MD, MSc3, Phenyo Phuu, MD4, Praneeth Bandaru, MD1, Yana Cavanagh, MD1
1St. Joseph's University Medical Center, Paterson, NJ; 2St. George's University School of Medicine, Paterson, NJ; 3Norwalk Hospital/Yale University, Norwalk, CT; 4St. Vincent’s Medical Center, Paterson, NJ
Introduction: Primary pancreatic follicular lymphoma (PPL) is an extremely rare form of extranodal non-Hodgkin lymphoma that originates in the pancreas.1,2 It accounts for less than 0.5% of pancreatic tumors and less than 1% of all extranodal lymphomas.1 Herein, we report a rare case of primary PPL discovered incidentally in a patient with symptomatic anemia.
Case Description/
Methods: A 65-year-old man with a history of type 2 diabetes presented to the ED with melena for one day. Triage labs: hemoglobin, 4.5 g/dL (reference range, 12.0-16.0), requiring 3 units of PRBCs. CT of the abdomen and pelvis revealed a thickened duodenum with air-fluid within it, suggestive of a duodenal ulcer. EGD showed a gastric nodule, food residue, and a large, ulcerated, non-bleeding mass near the papilla (Fig. 1). Colonoscopy was normal. Due to concern for ampullary mass, the patient underwent repeat EGD with endoscopic ultrasound (EUS) the next day. Endoscopic ultrasound (EUS) showed a mass in the uncinate process and fine-needle aspiration (FNA) was performed for histological analysis (Fig. 2). EUS also showed a prominent ampulla and mucosal resection was performed for tissue sampling. Histopathology showed duodenal mucosa with acute and chronic inflammation, ulceration, and focal reactive changes.
ERCP revealed an ulcerated and mass-like lesion in the major papilla and a filling defect on cholangiogram, consistent with a stone. A biliary sphincterotomy was performed, and a covered metal stent was placed into the common bile duct. FNA specimen showed CD10 positive B-cell lymphoma, which was consistent with follicular lymphoma. B-cell lymphocytes stained positive for CD20, PAX-5, CD10, BCL-6, BCL-2, and Ki67 was approximately 30%. The patient was transitioned to hospice care after six cycles of obinutuzumab monotherapy.
Discussion: Primary PPL is a rare but important diagnostic consideration in the evaluation of pancreatic masses. Cross-sectional imaging and tissue diagnosis with immunohistochemistry are key to differentiating lymphoma from more common pancreatic neoplasms. The primary treatment for PPL is systemic chemotherapy, often with regimens such as R-CHOP.3,4 CD20-targeting monoclonal antibodies can be considered in some cases. Surgery is generally reserved for diagnostic or palliative purposes rather than curative intent.1 Given the rarity of PPL, its management requires a high index of suspicion and a multidisciplinary approach to ensure timely and accurate diagnosis and appropriate treatment.
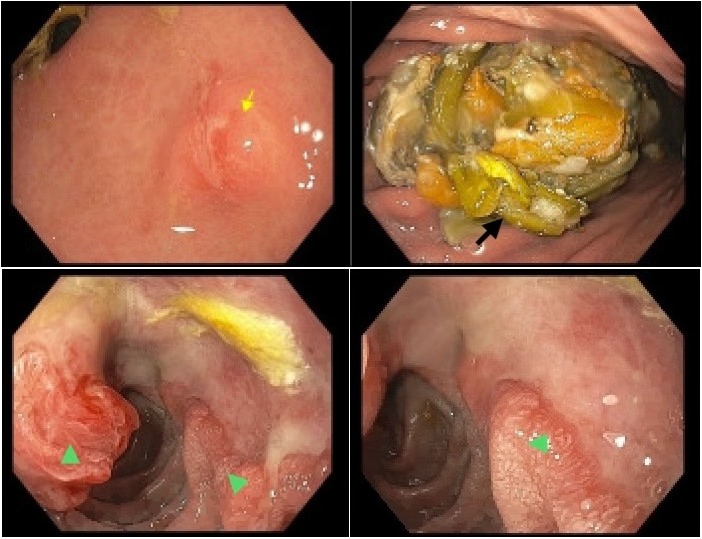
Figure: Figure 1. Endoscopic images showing a gastric nodule (yellow arrow), food residue, and a large, ulcerated, non-bleeding mass near the papilla (green arrows).
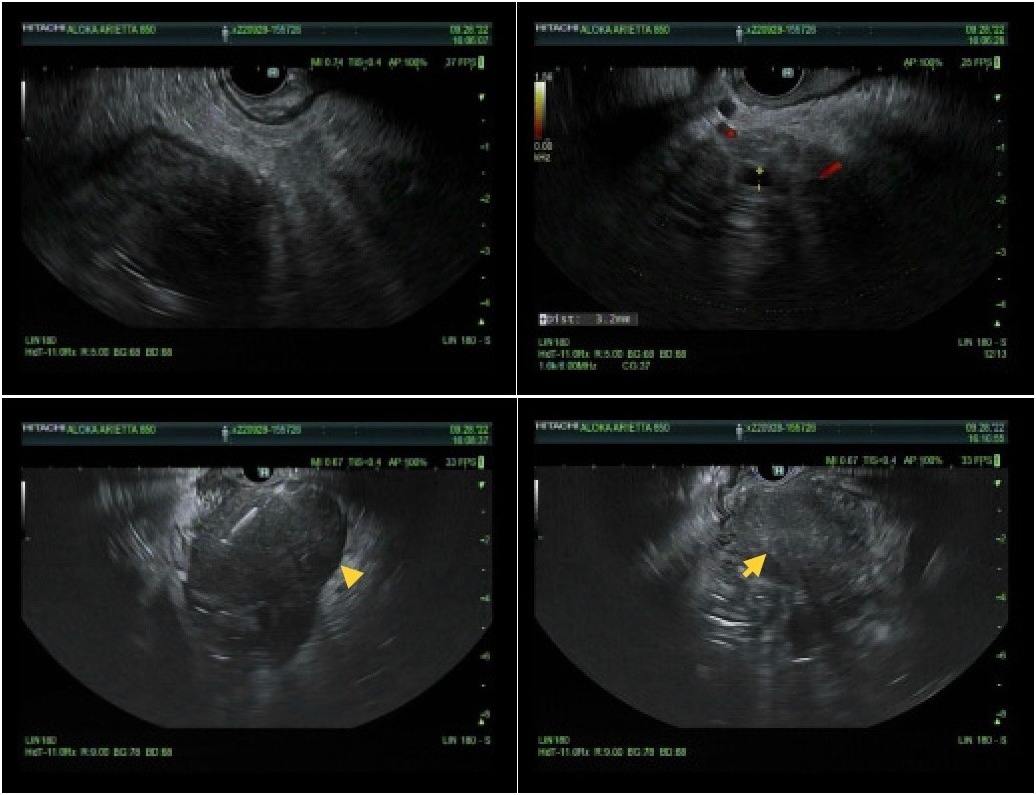
Figure: Figure 2. Endoscopic ultrasound showing an irregular, hypoechoic mass in the periampullary region of the pancreas measuring 56 mm by 58 mm in maximal cross-sectional diameter (yellow arrows).
Disclosures:
Lefika Bathobakae indicated no relevant financial relationships.
Dina Rohira indicated no relevant financial relationships.
Tasnim Fatima indicated no relevant financial relationships.
Rammy Bashir indicated no relevant financial relationships.
Phenyo Phuu indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Lefika Bathobakae, MD, MPH1, Dina Rohira, MD2, Tasnim Fatima, MD1, Rammy Bashir, MD, MSc3, Phenyo Phuu, MD4, Praneeth Bandaru, MD1, Yana Cavanagh, MD1. P2277 - Primary Pancreatic Follicular Lymphoma: A Rare Incidental Finding During Evaluation for GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2St. George's University School of Medicine, Paterson, NJ; 3Norwalk Hospital/Yale University, Norwalk, CT; 4St. Vincent’s Medical Center, Paterson, NJ
Introduction: Primary pancreatic follicular lymphoma (PPL) is an extremely rare form of extranodal non-Hodgkin lymphoma that originates in the pancreas.1,2 It accounts for less than 0.5% of pancreatic tumors and less than 1% of all extranodal lymphomas.1 Herein, we report a rare case of primary PPL discovered incidentally in a patient with symptomatic anemia.
Case Description/
Methods: A 65-year-old man with a history of type 2 diabetes presented to the ED with melena for one day. Triage labs: hemoglobin, 4.5 g/dL (reference range, 12.0-16.0), requiring 3 units of PRBCs. CT of the abdomen and pelvis revealed a thickened duodenum with air-fluid within it, suggestive of a duodenal ulcer. EGD showed a gastric nodule, food residue, and a large, ulcerated, non-bleeding mass near the papilla (Fig. 1). Colonoscopy was normal. Due to concern for ampullary mass, the patient underwent repeat EGD with endoscopic ultrasound (EUS) the next day. Endoscopic ultrasound (EUS) showed a mass in the uncinate process and fine-needle aspiration (FNA) was performed for histological analysis (Fig. 2). EUS also showed a prominent ampulla and mucosal resection was performed for tissue sampling. Histopathology showed duodenal mucosa with acute and chronic inflammation, ulceration, and focal reactive changes.
ERCP revealed an ulcerated and mass-like lesion in the major papilla and a filling defect on cholangiogram, consistent with a stone. A biliary sphincterotomy was performed, and a covered metal stent was placed into the common bile duct. FNA specimen showed CD10 positive B-cell lymphoma, which was consistent with follicular lymphoma. B-cell lymphocytes stained positive for CD20, PAX-5, CD10, BCL-6, BCL-2, and Ki67 was approximately 30%. The patient was transitioned to hospice care after six cycles of obinutuzumab monotherapy.
Discussion: Primary PPL is a rare but important diagnostic consideration in the evaluation of pancreatic masses. Cross-sectional imaging and tissue diagnosis with immunohistochemistry are key to differentiating lymphoma from more common pancreatic neoplasms. The primary treatment for PPL is systemic chemotherapy, often with regimens such as R-CHOP.3,4 CD20-targeting monoclonal antibodies can be considered in some cases. Surgery is generally reserved for diagnostic or palliative purposes rather than curative intent.1 Given the rarity of PPL, its management requires a high index of suspicion and a multidisciplinary approach to ensure timely and accurate diagnosis and appropriate treatment.
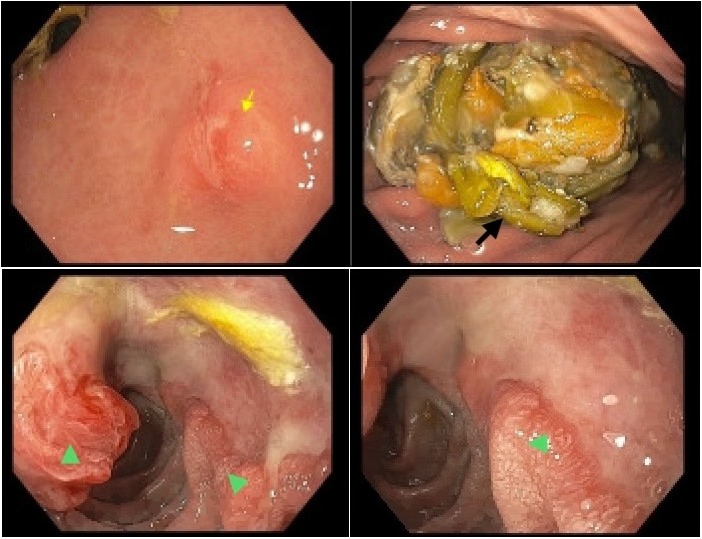
Figure: Figure 1. Endoscopic images showing a gastric nodule (yellow arrow), food residue, and a large, ulcerated, non-bleeding mass near the papilla (green arrows).
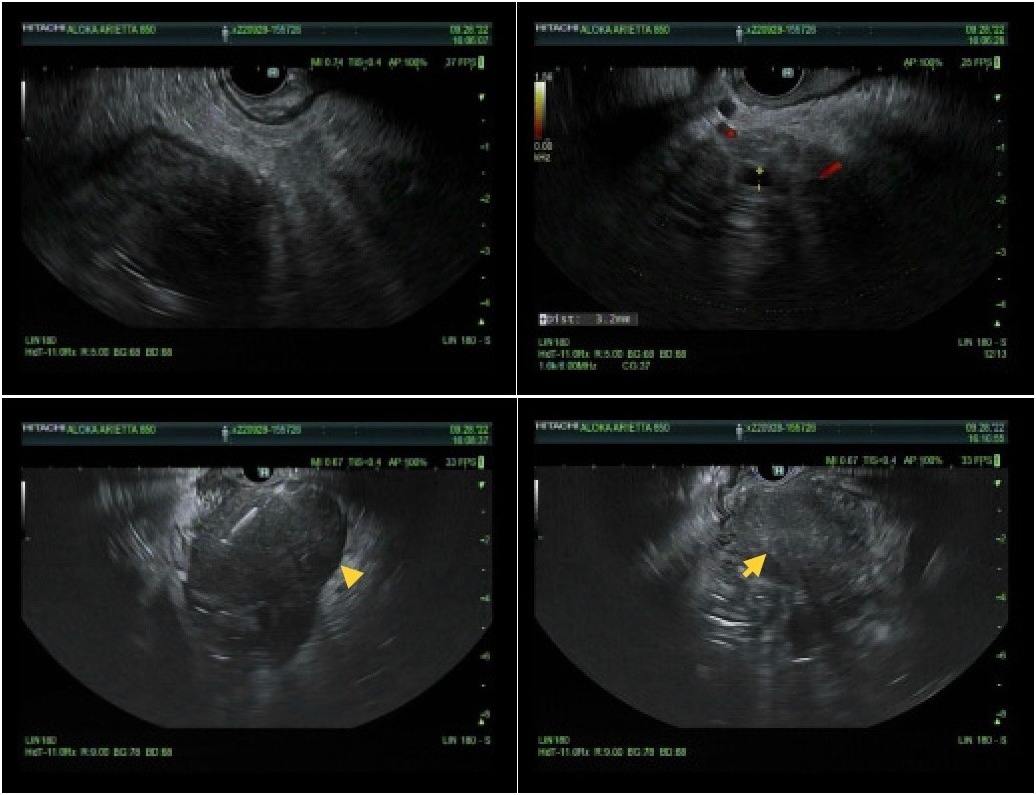
Figure: Figure 2. Endoscopic ultrasound showing an irregular, hypoechoic mass in the periampullary region of the pancreas measuring 56 mm by 58 mm in maximal cross-sectional diameter (yellow arrows).
Disclosures:
Lefika Bathobakae indicated no relevant financial relationships.
Dina Rohira indicated no relevant financial relationships.
Tasnim Fatima indicated no relevant financial relationships.
Rammy Bashir indicated no relevant financial relationships.
Phenyo Phuu indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Lefika Bathobakae, MD, MPH1, Dina Rohira, MD2, Tasnim Fatima, MD1, Rammy Bashir, MD, MSc3, Phenyo Phuu, MD4, Praneeth Bandaru, MD1, Yana Cavanagh, MD1. P2277 - Primary Pancreatic Follicular Lymphoma: A Rare Incidental Finding During Evaluation for GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
