Monday Poster Session
Category: Biliary/Pancreas
P2275 - Incidental IPMN in McCune-Albright Syndrome: A Case for Expanding Genetic Risk Stratification for Pancreatic Neoplasia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Lefika Bathobakae, MD, MPH
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Lefika Bathobakae, MD, MPH1, Reshma John, MD, MPH1, Aqsa Sorathia, MD1, Rammy Bashir, MD, MSc2, Praneeth Bandaru, MD1, Yana Cavanagh, MD1
1St. Joseph's University Medical Center, Paterson, NJ; 2Norwalk Hospital/Yale University, Norwalk, CT
Introduction: McCune-Albright Syndrome (MAS) is a rare mosaic genetic disorder caused by postzygotic activating mutations in the GNAS gene.1 It is classically characterized by fibrous dysplasia, café-au-lait macules, and endocrinopathies.2 Pancreatic intraductal papillary mucinous neoplasms (IPMNs) are cystic pancreatic tumors,3 with main duct IPMNs having a high risk of malignant transformation.4 Herein, we present a rare case of MAS with incidental detection of IPMN, raising important questions about cancer risk and surveillance in this population.
Case Description/
Methods: A 51-year-old woman with a history of McCune-Albright syndrome (MAS) and IBS-C presented to our clinic for abnormal imaging. The patient had an MRI of the abdomen with contrast for evaluation of a benign neoplasm of the right adrenal gland. MRI revealed an incidental cystic tubular structure anterior to the common bile duct, measuring approximately 4.5 cm x 1 cm, with small outpouchings adjacent to it (Figure 1). Labs: alkaline phosphatase, 338 IntlUnit/L (normal range; 44-121). EGD revealed multiple gastric polyps which were resected and pathology was benign. EUS revealed dilated pancreatic duct in the pancreatic head with a sudden transition to normal size at the level of the genu, suggestive of main duct IPMN. The pancreatic duct measured up to 7-8 mm in diameter.
During ERCP, the major papilla appeared patulous with mucin, giving a fish-mouth appearance (Figure 2). There was marked dilatation of the ventral pancreatic duct in the head of the pancreas to about 10-11 mm from the level of the ampulla with sudden transition to normal size duct at the genu, consistent with IPMN. FNA specimen was negative for malignant cells and mostly mucinous material and scattered inflammatory cells. The patient was counseled on the risk of pancreatobiliary malignancy and referred to the surgical service for evaluation.
Discussion: IPMNs are mucin-producing neoplasms of the pancreas that carry malignant potential. Activating GNAS mutations are frequently identified in IPMN and play a key role in tumorigenesis. MAS, caused by somatic GNAS mutations, shares this molecular alteration, yet its association with pancreatic neoplasia remains poorly defined. The incidental finding of IPMN in a patient with MAS raises the possibility that this mosaic disorder may confer an increased risk for pancreatic cystic neoplasms. Given the shared genetic pathway, it is plausible that patients with MAS represent an underrecognized high-risk group for pancreatic cancer.
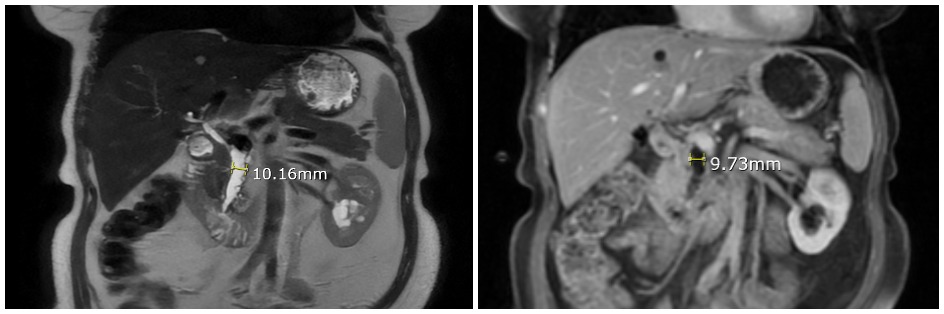
Figure: Figure 1. Magnetic resonance imaging of the abdomen (T2 sequence view) showing dilated main pancreatic duct in the head of the pancreas. No distal stones/strictures/obstructions noted. There was a sudden transition to normal caliber pancreatic duct at the level of the genu (not shown on this image). The rest of the pancreas, including the duct and parenchyma, was normal. These image findings likely represent the main duct IPMN.

Figure: Figure 2. Endoscopic retrograde cholangiopancreatography images showing the typical fish mouth appearance of the pancreatic duct opening with mucin extruding, consistent with the main duct IPMN. The middle and right panels are Spyglass/pancreatioscopy images showing a dilated pancreatic duct with mucin debris and dilated side branches. No intraductal lesions noted.
Disclosures:
Lefika Bathobakae indicated no relevant financial relationships.
Reshma John indicated no relevant financial relationships.
Aqsa Sorathia indicated no relevant financial relationships.
Rammy Bashir indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Lefika Bathobakae, MD, MPH1, Reshma John, MD, MPH1, Aqsa Sorathia, MD1, Rammy Bashir, MD, MSc2, Praneeth Bandaru, MD1, Yana Cavanagh, MD1. P2275 - Incidental IPMN in McCune-Albright Syndrome: A Case for Expanding Genetic Risk Stratification for Pancreatic Neoplasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2Norwalk Hospital/Yale University, Norwalk, CT
Introduction: McCune-Albright Syndrome (MAS) is a rare mosaic genetic disorder caused by postzygotic activating mutations in the GNAS gene.1 It is classically characterized by fibrous dysplasia, café-au-lait macules, and endocrinopathies.2 Pancreatic intraductal papillary mucinous neoplasms (IPMNs) are cystic pancreatic tumors,3 with main duct IPMNs having a high risk of malignant transformation.4 Herein, we present a rare case of MAS with incidental detection of IPMN, raising important questions about cancer risk and surveillance in this population.
Case Description/
Methods: A 51-year-old woman with a history of McCune-Albright syndrome (MAS) and IBS-C presented to our clinic for abnormal imaging. The patient had an MRI of the abdomen with contrast for evaluation of a benign neoplasm of the right adrenal gland. MRI revealed an incidental cystic tubular structure anterior to the common bile duct, measuring approximately 4.5 cm x 1 cm, with small outpouchings adjacent to it (Figure 1). Labs: alkaline phosphatase, 338 IntlUnit/L (normal range; 44-121). EGD revealed multiple gastric polyps which were resected and pathology was benign. EUS revealed dilated pancreatic duct in the pancreatic head with a sudden transition to normal size at the level of the genu, suggestive of main duct IPMN. The pancreatic duct measured up to 7-8 mm in diameter.
During ERCP, the major papilla appeared patulous with mucin, giving a fish-mouth appearance (Figure 2). There was marked dilatation of the ventral pancreatic duct in the head of the pancreas to about 10-11 mm from the level of the ampulla with sudden transition to normal size duct at the genu, consistent with IPMN. FNA specimen was negative for malignant cells and mostly mucinous material and scattered inflammatory cells. The patient was counseled on the risk of pancreatobiliary malignancy and referred to the surgical service for evaluation.
Discussion: IPMNs are mucin-producing neoplasms of the pancreas that carry malignant potential. Activating GNAS mutations are frequently identified in IPMN and play a key role in tumorigenesis. MAS, caused by somatic GNAS mutations, shares this molecular alteration, yet its association with pancreatic neoplasia remains poorly defined. The incidental finding of IPMN in a patient with MAS raises the possibility that this mosaic disorder may confer an increased risk for pancreatic cystic neoplasms. Given the shared genetic pathway, it is plausible that patients with MAS represent an underrecognized high-risk group for pancreatic cancer.
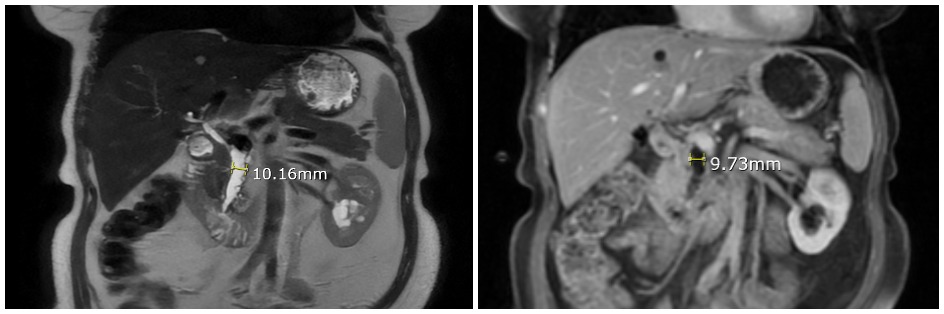
Figure: Figure 1. Magnetic resonance imaging of the abdomen (T2 sequence view) showing dilated main pancreatic duct in the head of the pancreas. No distal stones/strictures/obstructions noted. There was a sudden transition to normal caliber pancreatic duct at the level of the genu (not shown on this image). The rest of the pancreas, including the duct and parenchyma, was normal. These image findings likely represent the main duct IPMN.

Figure: Figure 2. Endoscopic retrograde cholangiopancreatography images showing the typical fish mouth appearance of the pancreatic duct opening with mucin extruding, consistent with the main duct IPMN. The middle and right panels are Spyglass/pancreatioscopy images showing a dilated pancreatic duct with mucin debris and dilated side branches. No intraductal lesions noted.
Disclosures:
Lefika Bathobakae indicated no relevant financial relationships.
Reshma John indicated no relevant financial relationships.
Aqsa Sorathia indicated no relevant financial relationships.
Rammy Bashir indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Lefika Bathobakae, MD, MPH1, Reshma John, MD, MPH1, Aqsa Sorathia, MD1, Rammy Bashir, MD, MSc2, Praneeth Bandaru, MD1, Yana Cavanagh, MD1. P2275 - Incidental IPMN in McCune-Albright Syndrome: A Case for Expanding Genetic Risk Stratification for Pancreatic Neoplasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
