Monday Poster Session
Category: Biliary/Pancreas
P2271 - G-Tube Migration Causing Acute Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- BW
Bryan Wey, MD
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Bryan Wey, MD, Ronak Modi, MD
St. Luke's University Health Network, Bethlehem, PA
Introduction: We present a case of an 80-year-old female with a medical history of multiple hemorrhagic strokes resulting in hemiparesis and dysphagia status post PEG tube placement for enteral feeding who presented from her facility for nausea, vomiting and abdominal pain. On presentation her vitals were unremarkable. Labs showed a mild leukocytosis of 11.82 k/µL and a lipase > 12000 u/L. CT scan of the abdomen showed peripancreatic edema without necrosis as well as interval migration of gastrostomy tube to the proximal small bowel.
Case Description/
Methods: The patient’s most recent hemorrhagic stroke occurred one year ago at an outside hospital. During that stay, interventional radiology had placed an 18 Fr Entuit® gastrostomy tube with a 10 cc balloon. She had several subsequent hospital visits for dislodged gastrostomy tubes requiring replacements. Three weeks before her most recent hospitalization, she was admitted for pneumonia. CT scan then showed the distal tip of the gastrostomy tube in the antrum of the stomach (Figure 1). During her presentation here, CT scan of the abdomen showed peripancreatic edema without necrosis as well as interval migration of gastrostomy tube to the proximal small bowel (Figure 2). On bedside exam, the patient had a 18 Fr Kangaroo™ gastrostomy tube with a 20cc balloon. There was minimal external tubing and the external bumper was at 14 cm at the skin level. The balloon was deflated and the tube was retracted. The balloon was then reinflated without resistance and the external bumper was tightened to 1.8 cm at the skin level. The patient was resumed on enteral feeds and otherwise had an uncomplicated stay for mild acute pancreatitis.
Discussion: Acute interstitial pancreatitis is typically caused by alcohol or gallstones. Other obstructive etiologies include a pancreatic head mass, ampullary polyp/tumor or papillary stenosis, which are very uncommon. There are rare case reports of a migrated gastrostomy tube balloon obstructing the ampulla leading to pancreatitis. Gastrostomy tubes migration is not uncommon. Patients who are at higher risk include those who are non-verbal or reside in a long-term care facility. Frequent tube care and securing the external tubing can minimize the risk of inward tube migration.
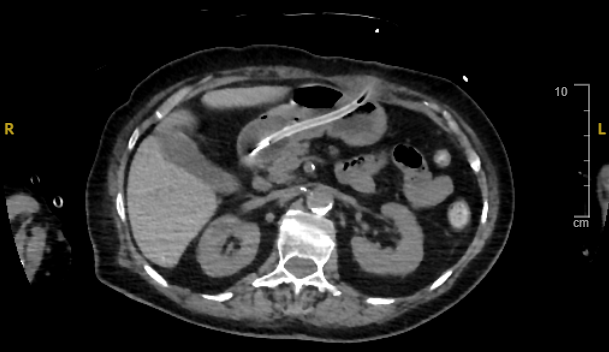
Figure: Figure 1. Distal tip of the gastrostomy tube with inflated balloon in the antrum of the stomach.

Figure: Figure 2. Distal tip of the gastrostomy tube in the second portion of the duodenum. (Yellow arrow: distal common bile duct. Red arrow: pancreatic duct. Blue arrow: inflated balloon distending the duodenal lumen at the level of the ampulla).
Disclosures:
Bryan Wey indicated no relevant financial relationships.
Ronak Modi indicated no relevant financial relationships.
Bryan Wey, MD, Ronak Modi, MD. P2271 - G-Tube Migration Causing Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
St. Luke's University Health Network, Bethlehem, PA
Introduction: We present a case of an 80-year-old female with a medical history of multiple hemorrhagic strokes resulting in hemiparesis and dysphagia status post PEG tube placement for enteral feeding who presented from her facility for nausea, vomiting and abdominal pain. On presentation her vitals were unremarkable. Labs showed a mild leukocytosis of 11.82 k/µL and a lipase > 12000 u/L. CT scan of the abdomen showed peripancreatic edema without necrosis as well as interval migration of gastrostomy tube to the proximal small bowel.
Case Description/
Methods: The patient’s most recent hemorrhagic stroke occurred one year ago at an outside hospital. During that stay, interventional radiology had placed an 18 Fr Entuit® gastrostomy tube with a 10 cc balloon. She had several subsequent hospital visits for dislodged gastrostomy tubes requiring replacements. Three weeks before her most recent hospitalization, she was admitted for pneumonia. CT scan then showed the distal tip of the gastrostomy tube in the antrum of the stomach (Figure 1). During her presentation here, CT scan of the abdomen showed peripancreatic edema without necrosis as well as interval migration of gastrostomy tube to the proximal small bowel (Figure 2). On bedside exam, the patient had a 18 Fr Kangaroo™ gastrostomy tube with a 20cc balloon. There was minimal external tubing and the external bumper was at 14 cm at the skin level. The balloon was deflated and the tube was retracted. The balloon was then reinflated without resistance and the external bumper was tightened to 1.8 cm at the skin level. The patient was resumed on enteral feeds and otherwise had an uncomplicated stay for mild acute pancreatitis.
Discussion: Acute interstitial pancreatitis is typically caused by alcohol or gallstones. Other obstructive etiologies include a pancreatic head mass, ampullary polyp/tumor or papillary stenosis, which are very uncommon. There are rare case reports of a migrated gastrostomy tube balloon obstructing the ampulla leading to pancreatitis. Gastrostomy tubes migration is not uncommon. Patients who are at higher risk include those who are non-verbal or reside in a long-term care facility. Frequent tube care and securing the external tubing can minimize the risk of inward tube migration.
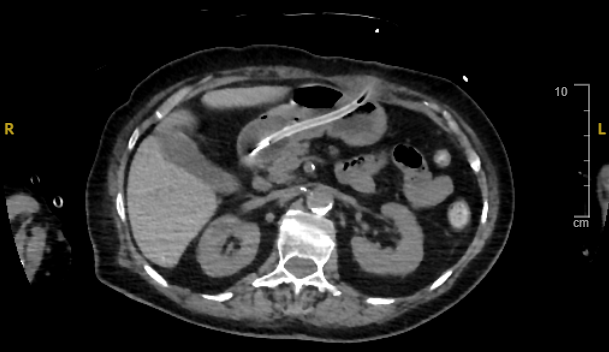
Figure: Figure 1. Distal tip of the gastrostomy tube with inflated balloon in the antrum of the stomach.

Figure: Figure 2. Distal tip of the gastrostomy tube in the second portion of the duodenum. (Yellow arrow: distal common bile duct. Red arrow: pancreatic duct. Blue arrow: inflated balloon distending the duodenal lumen at the level of the ampulla).
Disclosures:
Bryan Wey indicated no relevant financial relationships.
Ronak Modi indicated no relevant financial relationships.
Bryan Wey, MD, Ronak Modi, MD. P2271 - G-Tube Migration Causing Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
