Monday Poster Session
Category: Biliary/Pancreas
P2254 - Ketamine-Induced Biliary Injury: A Potential Precursor to Vanishing Bile Duct Syndrome
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Priya Kumari Maheshwari, MD (she/her/hers)
University of Central Florida, HCA Healthcare GME
Pensacola, FL
Presenting Author(s)
Priya Kumari Maheshwari, MD1, Inshaal Yasin, MD1, Ali Tariq, MD2, Michel Sabra, MD1, Maro Issac, PharmD3, Bola Habeb, MD4, William Goldsmith, MD5, Peter Fahim, MD6
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2HCA FLORIDA WEST HOSPITAL, Pensacola, FL; 3German University Egypt, Pensacola, FL; 4Florida State University/ Ascension Sacred Heart- Internal Medicine Department, Pensacola, FL; 5HCA Florida Healthcare, Pensacola, FL; 6Critical Care Medicine, University of Central Florida/HCA Florida West Hospital, Pensacola, FL
Introduction: Vanishing bile duct syndrome (VBDS), a rare cholestatic disorder characterized by irreversible loss of intrahepatic bile ducts. Commonly associated with autoimmune diseases, infections, and DILI, it remains a diagnostic challenge. Ketamine-induced cholangiopathy, though primarily described in chronic abuse or ICU sedation, has emerged as a potential contributor. However, its association with VBDS is not well established. We present a case of biopsy-confirmed VBDS with imaging resembling primary sclerosing cholangitis (PSC), in a patient with prior ketamine exposure, raising the possibility of a causal link.
Case Description/
Methods: A 56-year-old woman with no history of alcohol use presented with progressive jaundice and episodes of altered mental status. Her medical history included herpes simplex virus encephalitis, during which she required intubation and brief ketamine sedation. Months later, she developed acute cholestatic liver injury. Laboratory testing revealed hyperbilirubinemia, elevated alkaline phosphatase, and transaminases.
MRCP (Figure 1) revealed intrahepatic bile duct dilation with beading. Liver biopsy demonstrated ductopenia, consistent with VBDS and sclerosing cholangitis. ERCP showed multifocal ductal irregularities suggestive of a PSC-like pattern. However, autoimmune serologies were negative, and the patient had no history of inflammatory bowel disease.
She was treated with ursodeoxycholic acid, corticosteroids, and symptomatic measures, but continued to deteriorate. Her course was complicated by recurrent episodes of bacteremia, vertebral compression fractures, sacral wounds, and intrapulmonary shunting. Liver transplant evaluation was deferred due to poor functional status. She ultimately succumbed to complications of liver failure and sepsis.
Discussion: This case illustrates a potential continuum from ketamine-induced cholangiopathy to VBDS. Ketamine has been increasingly recognized as a cause of secondary sclerosing cholangitis, particularly in chronic abuse or ICU settings. Proposed mechanisms include direct cholangiocyte toxicity, increased bile viscosity, and biliary ischemia, leading to progressive ductal injury and loss. Although PSC was initially considered based on cholangiographic features, the absence of autoimmune markers or IBD, coupled with the temporal relationship to ketamine exposure, supports secondary cholangiopathy. The subsequent development of VBDS, suggests ketamine may trigger a progressive biliary injury culminating in irreversible ductopenia.
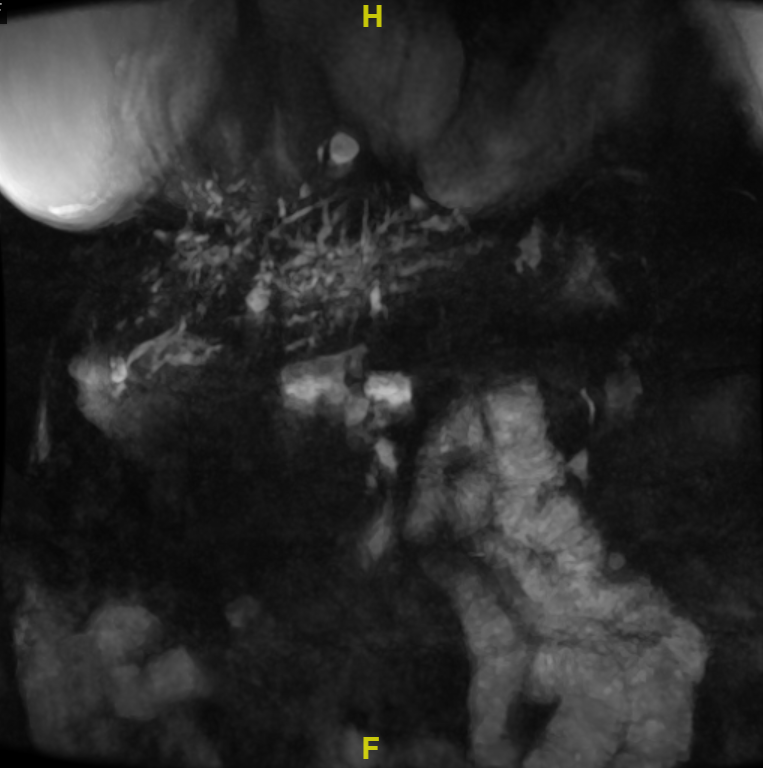
Figure: Figure 1: MRCP image demonstrating intrahepatic bile duct dilation with multifocal strictures and beading.
Disclosures:
Priya Kumari Maheshwari indicated no relevant financial relationships.
Inshaal Yasin indicated no relevant financial relationships.
Ali Tariq indicated no relevant financial relationships.
Michel Sabra indicated no relevant financial relationships.
Maro Issac indicated no relevant financial relationships.
Bola Habeb indicated no relevant financial relationships.
William Goldsmith indicated no relevant financial relationships.
Peter Fahim indicated no relevant financial relationships.
Priya Kumari Maheshwari, MD1, Inshaal Yasin, MD1, Ali Tariq, MD2, Michel Sabra, MD1, Maro Issac, PharmD3, Bola Habeb, MD4, William Goldsmith, MD5, Peter Fahim, MD6. P2254 - Ketamine-Induced Biliary Injury: A Potential Precursor to Vanishing Bile Duct Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2HCA FLORIDA WEST HOSPITAL, Pensacola, FL; 3German University Egypt, Pensacola, FL; 4Florida State University/ Ascension Sacred Heart- Internal Medicine Department, Pensacola, FL; 5HCA Florida Healthcare, Pensacola, FL; 6Critical Care Medicine, University of Central Florida/HCA Florida West Hospital, Pensacola, FL
Introduction: Vanishing bile duct syndrome (VBDS), a rare cholestatic disorder characterized by irreversible loss of intrahepatic bile ducts. Commonly associated with autoimmune diseases, infections, and DILI, it remains a diagnostic challenge. Ketamine-induced cholangiopathy, though primarily described in chronic abuse or ICU sedation, has emerged as a potential contributor. However, its association with VBDS is not well established. We present a case of biopsy-confirmed VBDS with imaging resembling primary sclerosing cholangitis (PSC), in a patient with prior ketamine exposure, raising the possibility of a causal link.
Case Description/
Methods: A 56-year-old woman with no history of alcohol use presented with progressive jaundice and episodes of altered mental status. Her medical history included herpes simplex virus encephalitis, during which she required intubation and brief ketamine sedation. Months later, she developed acute cholestatic liver injury. Laboratory testing revealed hyperbilirubinemia, elevated alkaline phosphatase, and transaminases.
MRCP (Figure 1) revealed intrahepatic bile duct dilation with beading. Liver biopsy demonstrated ductopenia, consistent with VBDS and sclerosing cholangitis. ERCP showed multifocal ductal irregularities suggestive of a PSC-like pattern. However, autoimmune serologies were negative, and the patient had no history of inflammatory bowel disease.
She was treated with ursodeoxycholic acid, corticosteroids, and symptomatic measures, but continued to deteriorate. Her course was complicated by recurrent episodes of bacteremia, vertebral compression fractures, sacral wounds, and intrapulmonary shunting. Liver transplant evaluation was deferred due to poor functional status. She ultimately succumbed to complications of liver failure and sepsis.
Discussion: This case illustrates a potential continuum from ketamine-induced cholangiopathy to VBDS. Ketamine has been increasingly recognized as a cause of secondary sclerosing cholangitis, particularly in chronic abuse or ICU settings. Proposed mechanisms include direct cholangiocyte toxicity, increased bile viscosity, and biliary ischemia, leading to progressive ductal injury and loss. Although PSC was initially considered based on cholangiographic features, the absence of autoimmune markers or IBD, coupled with the temporal relationship to ketamine exposure, supports secondary cholangiopathy. The subsequent development of VBDS, suggests ketamine may trigger a progressive biliary injury culminating in irreversible ductopenia.
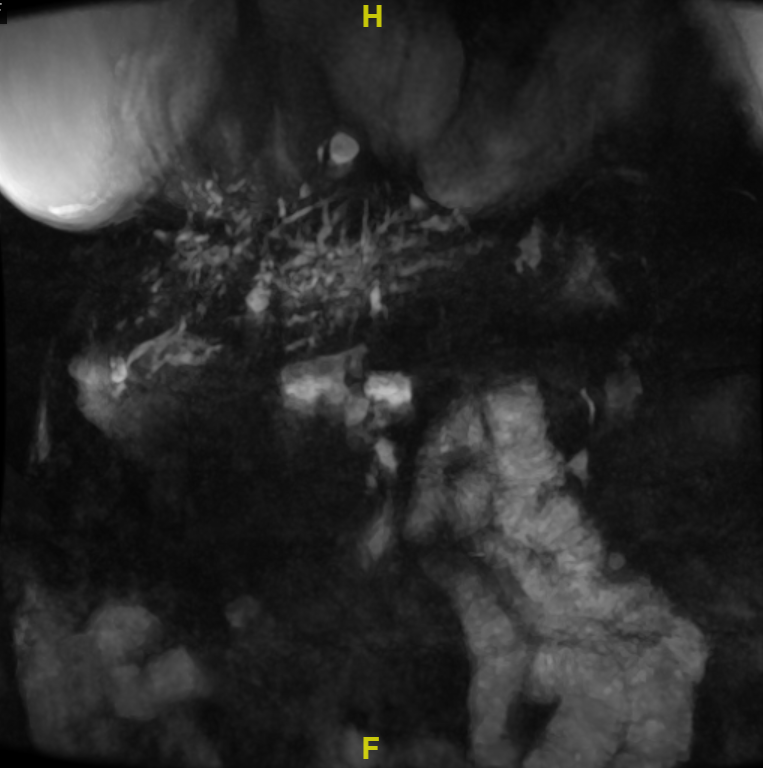
Figure: Figure 1: MRCP image demonstrating intrahepatic bile duct dilation with multifocal strictures and beading.
Disclosures:
Priya Kumari Maheshwari indicated no relevant financial relationships.
Inshaal Yasin indicated no relevant financial relationships.
Ali Tariq indicated no relevant financial relationships.
Michel Sabra indicated no relevant financial relationships.
Maro Issac indicated no relevant financial relationships.
Bola Habeb indicated no relevant financial relationships.
William Goldsmith indicated no relevant financial relationships.
Peter Fahim indicated no relevant financial relationships.
Priya Kumari Maheshwari, MD1, Inshaal Yasin, MD1, Ali Tariq, MD2, Michel Sabra, MD1, Maro Issac, PharmD3, Bola Habeb, MD4, William Goldsmith, MD5, Peter Fahim, MD6. P2254 - Ketamine-Induced Biliary Injury: A Potential Precursor to Vanishing Bile Duct Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

