Monday Poster Session
Category: Biliary/Pancreas
P2163 - How Much Fluid Is Too Much Fluid? Fluid Resuscitation in Acute Pancreatitis in Patients With History of Congestive Heart Failure
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nisha R. Sanghani, DO
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Nisha R. Sanghani, DO1, Brett D. Cohen, DO2, Nishanth Eluri, MD2, Samuel Levine, MD1, Monica Dzwonkowski, DO1, Het Patel, DO3, Matthew J. Record, BA4, Kyle Tio, MD5, Rana Moawad, BSc6, Kimberly J. Chaput, DO7
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Hospital, Bethlehem, PA; 3St. Luke's Hospital, Bethlehem, PA; 4St. Luke’s University Hospital, Bethlehem, PA; 5St. Luke's University Health Network, Fountain Hill, PA; 6Lewis Katz School of Medicine at Temple University, Coplay, PA; 7St Luke's Gastroenterology, Center Valley, PA
Introduction: The mainstay of treatment for acute pancreatitis was classically aggressive fluid resuscitation. Recent studies have found that moderate fluid resuscitation is superior to that of aggressive, as patients are adequately treated without the adverse effects of fluid overload. However, these studies excluded patients with history of congestive heart failure (CHF). We studied patients who presented to St. Luke’s hospitals with acute pancreatitis and history of CHF to understand differences in fluid resuscitation and complications between those who developed acute decompensated heart failure (ADHF) and those who did not.
Methods: A retrospective chart review was performed on adult patients with a history of CHF who presented to St. Luke’s hospitals from 2019 to 2025 with acute pancreatitis. 279 encounters were reviewed. Patients with stage 4 chronic kidney disease, end stage renal disease on dialysis, decompensated cirrhosis, and ADHF on presentation were excluded. Of the remaining 189 patients, we compared fluid administration, outcomes, and complications between those who developed ADHF with that of those who did not. Statistical analyses were performed with STATA software.
Results: Of the 189 patients admitted with acute pancreatitis, 26.5% developed ADHF during their hospitalization. Those who developed ADHF received higher fluid boluses (mean 1.22L vs. 0.84L; p=0.010), had longer hospital stays (median 7 vs. 4 days; p< 0.001), and had a higher incidence of moderately severe or severe pancreatitis (54% vs. 19.4%; p< 0.001). Thirty-day readmission was more frequent in the ADHF group (38% vs. 24.5%), approaching but not reaching statistical significance (p = 0.098).
Discussion: This analysis highlights that larger fluid bolus administration may result in the development of ADHF, which is associated with worse outcomes and longer hospital lengths of stay. Previous literature, most prominently the WATERFALL trial, has shown the harms associated with aggressive early volume resuscitation in acute pancreatitis without including heart failure patients. This study points to the adverse role of fluid boluses specifically and suggests continuous fluids may be a better choice for fluid resuscitation in this population. Optimizing fluid resuscitation in patients with known CHF may reduce the risk of decompensation and associated complications, decreasing length of stay and improving both short- and long-term outcomes. Future prospective studies should be performed to help solidify this.
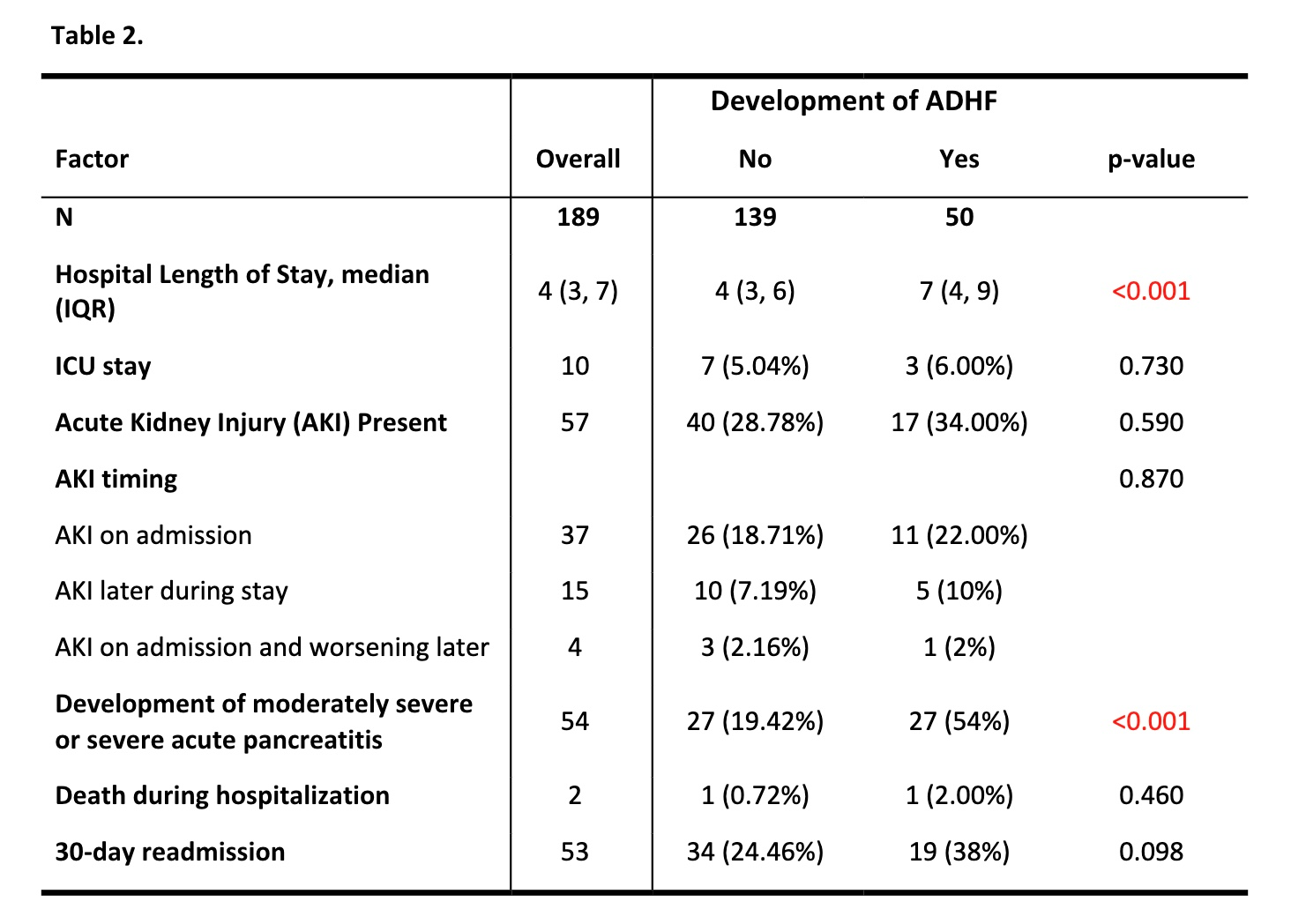
Figure: Comparison of the development of acute decompensated heart failure (ADHF) across demographic variables, admission characteristics, and amount of fluid administration in heart failure patients presenting with acute pancreatitis
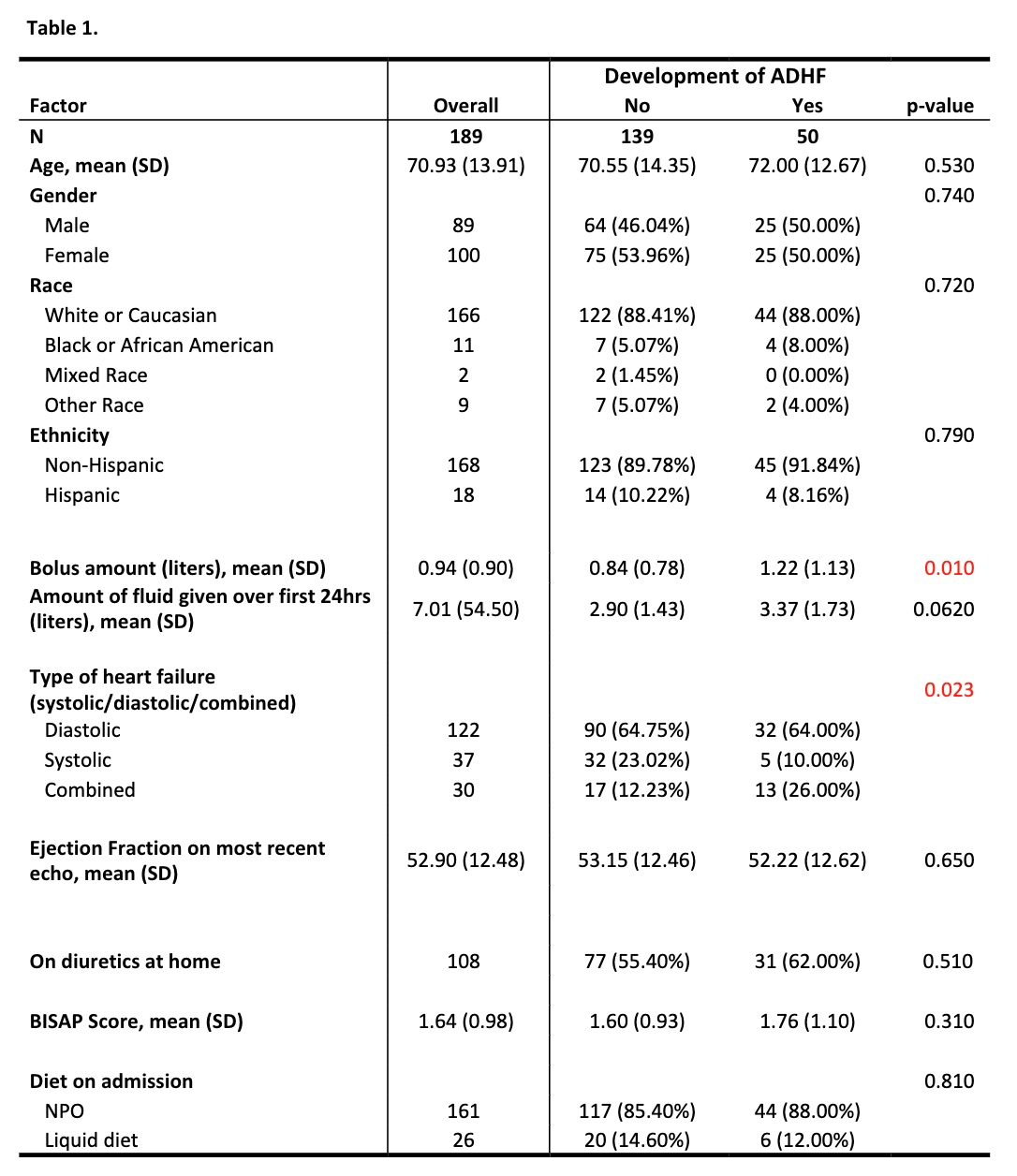
Figure: Comparison of the development of acute decompensated heart failure (ADHF) across outcome variables of interest in heart failure patients presenting with acute pancreatitis
Disclosures:
Nisha Sanghani indicated no relevant financial relationships.
Brett Cohen indicated no relevant financial relationships.
Nishanth Eluri indicated no relevant financial relationships.
Samuel Levine indicated no relevant financial relationships.
Monica Dzwonkowski indicated no relevant financial relationships.
Het Patel indicated no relevant financial relationships.
Matthew Record indicated no relevant financial relationships.
Kyle Tio indicated no relevant financial relationships.
Rana Moawad indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Nisha R. Sanghani, DO1, Brett D. Cohen, DO2, Nishanth Eluri, MD2, Samuel Levine, MD1, Monica Dzwonkowski, DO1, Het Patel, DO3, Matthew J. Record, BA4, Kyle Tio, MD5, Rana Moawad, BSc6, Kimberly J. Chaput, DO7. P2163 - How Much Fluid Is Too Much Fluid? Fluid Resuscitation in Acute Pancreatitis in Patients With History of Congestive Heart Failure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Hospital, Bethlehem, PA; 3St. Luke's Hospital, Bethlehem, PA; 4St. Luke’s University Hospital, Bethlehem, PA; 5St. Luke's University Health Network, Fountain Hill, PA; 6Lewis Katz School of Medicine at Temple University, Coplay, PA; 7St Luke's Gastroenterology, Center Valley, PA
Introduction: The mainstay of treatment for acute pancreatitis was classically aggressive fluid resuscitation. Recent studies have found that moderate fluid resuscitation is superior to that of aggressive, as patients are adequately treated without the adverse effects of fluid overload. However, these studies excluded patients with history of congestive heart failure (CHF). We studied patients who presented to St. Luke’s hospitals with acute pancreatitis and history of CHF to understand differences in fluid resuscitation and complications between those who developed acute decompensated heart failure (ADHF) and those who did not.
Methods: A retrospective chart review was performed on adult patients with a history of CHF who presented to St. Luke’s hospitals from 2019 to 2025 with acute pancreatitis. 279 encounters were reviewed. Patients with stage 4 chronic kidney disease, end stage renal disease on dialysis, decompensated cirrhosis, and ADHF on presentation were excluded. Of the remaining 189 patients, we compared fluid administration, outcomes, and complications between those who developed ADHF with that of those who did not. Statistical analyses were performed with STATA software.
Results: Of the 189 patients admitted with acute pancreatitis, 26.5% developed ADHF during their hospitalization. Those who developed ADHF received higher fluid boluses (mean 1.22L vs. 0.84L; p=0.010), had longer hospital stays (median 7 vs. 4 days; p< 0.001), and had a higher incidence of moderately severe or severe pancreatitis (54% vs. 19.4%; p< 0.001). Thirty-day readmission was more frequent in the ADHF group (38% vs. 24.5%), approaching but not reaching statistical significance (p = 0.098).
Discussion: This analysis highlights that larger fluid bolus administration may result in the development of ADHF, which is associated with worse outcomes and longer hospital lengths of stay. Previous literature, most prominently the WATERFALL trial, has shown the harms associated with aggressive early volume resuscitation in acute pancreatitis without including heart failure patients. This study points to the adverse role of fluid boluses specifically and suggests continuous fluids may be a better choice for fluid resuscitation in this population. Optimizing fluid resuscitation in patients with known CHF may reduce the risk of decompensation and associated complications, decreasing length of stay and improving both short- and long-term outcomes. Future prospective studies should be performed to help solidify this.
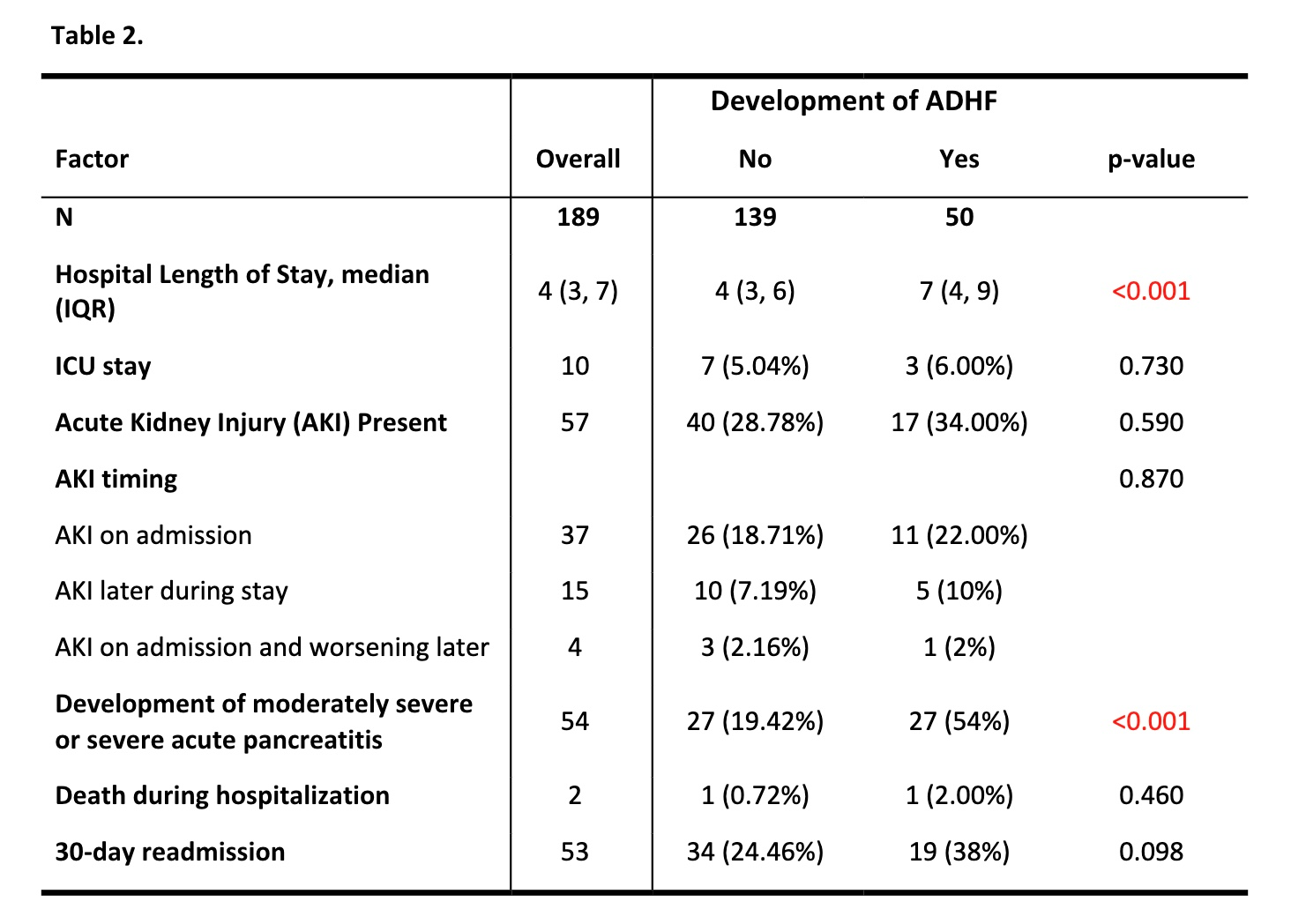
Figure: Comparison of the development of acute decompensated heart failure (ADHF) across demographic variables, admission characteristics, and amount of fluid administration in heart failure patients presenting with acute pancreatitis
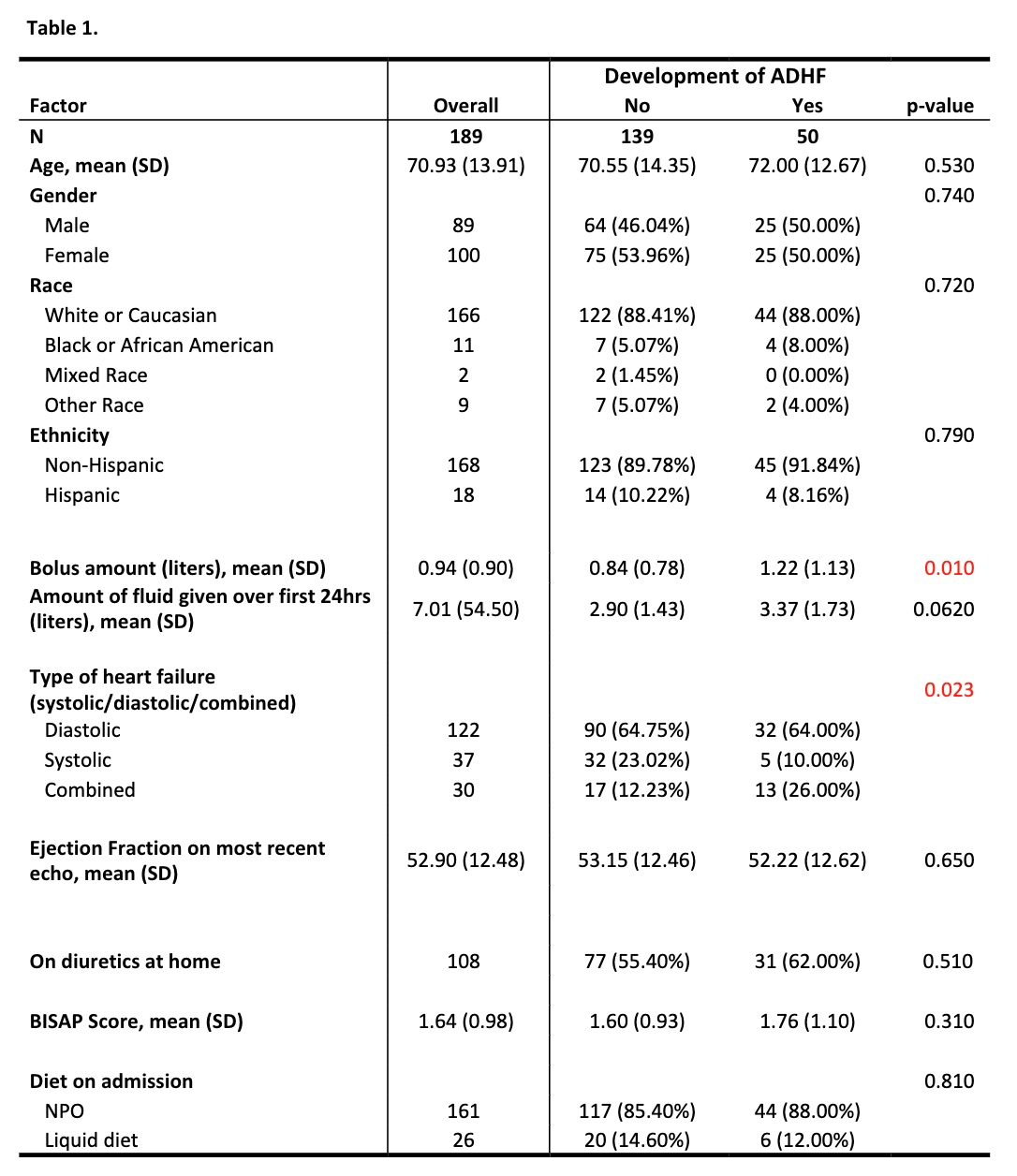
Figure: Comparison of the development of acute decompensated heart failure (ADHF) across outcome variables of interest in heart failure patients presenting with acute pancreatitis
Disclosures:
Nisha Sanghani indicated no relevant financial relationships.
Brett Cohen indicated no relevant financial relationships.
Nishanth Eluri indicated no relevant financial relationships.
Samuel Levine indicated no relevant financial relationships.
Monica Dzwonkowski indicated no relevant financial relationships.
Het Patel indicated no relevant financial relationships.
Matthew Record indicated no relevant financial relationships.
Kyle Tio indicated no relevant financial relationships.
Rana Moawad indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Nisha R. Sanghani, DO1, Brett D. Cohen, DO2, Nishanth Eluri, MD2, Samuel Levine, MD1, Monica Dzwonkowski, DO1, Het Patel, DO3, Matthew J. Record, BA4, Kyle Tio, MD5, Rana Moawad, BSc6, Kimberly J. Chaput, DO7. P2163 - How Much Fluid Is Too Much Fluid? Fluid Resuscitation in Acute Pancreatitis in Patients With History of Congestive Heart Failure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
