Monday Poster Session
Category: Biliary/Pancreas
P2154 - Impact of Rurality and Age at Onset on Pancreatic Cancer Survival: A Population-Based Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ooreoluwa Fasola, MD
Texas Tech University Health Sciences Center - Permian Basin
Odessa, TX
Presenting Author(s)
Ooreoluwa Fasola, MD1, Eunice Aregbesola, MD2, Gloria Erazo, MD3, Anjul Verma, MD3, Guy Loic Nguefang Tchoukeu, MD3, Godfrey Tabowei, MD4, Eunice Omeludike, MD5
1Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX; 2University of Missouri , Columbia, Columbia, MO; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Texas Tech University Health Science center, Permian Basin, Odessa, TX; 5Piedmont Athens Regional Medical Centre, Athens, GA
Introduction: Pancreatic cancer is the third leading cause of cancer-related mortality, with increasing incidence and mortality among individuals younger than 50 years. However, the combined impact of rural residence and age at diagnosis on survival outcomes remains unclear. This study aimed to evaluate whether rurality influences survival in early-onset (< 50 years) and late-onset ( >50 years) pancreatic cancer using a population-based dataset.
Methods: We used the Surveillance, Epidemiology and End Results (SEER) database to identify patients aged 20–79 years diagnosed with pancreatic cancer between 2000 and 2020, categorizing them as early-onset (20–49 years) or late-onset (50–79 years). Rural versus urban residence was determined using SEER rural-urban continuum codes. Kaplan–Meier analysis was used to compare survival, and multivariable Cox proportional hazards models assessed the impact of rurality on survival, adjusting for potential confounders. An interaction term tested whether rurality and age at onset had a combined effect on survival.
Results: Of 34,996 patients, 3,000 had early-onset pancreatic cancer and 31,996 had late-onset disease. Among early-onset patients, 88.2% resided in urban areas, compared to 84.9% of those with late-onset disease. Five-year survival was lower in rural than urban residents for both early-onset (26% vs. 31.2%) and late-onset cases (9.8% vs. 12.1%) (Figure 1). In adjusted analyses, urban residents had a lower risk of death than rural residents (aHR 0.93; 95% CI 0.91–0.97; p < 0.001) (Figure 2). Late-onset patients had a significantly higher mortality risk than early-onset patients (aHR 10.66; 95% CI 5.00–24.84; p < 0.001). The interaction between rurality and age at onset was not statistically significant (aHR 1.02; 95% CI 0.89–1.16; p = 0.775), suggesting independent effects.
Discussion: Rural residence is associated with poorer 5-year survival in pancreatic cancer, independent of age at diagnosis. These findings underscore the urgent need for equitable healthcare access and targeted interventions in rural populations.
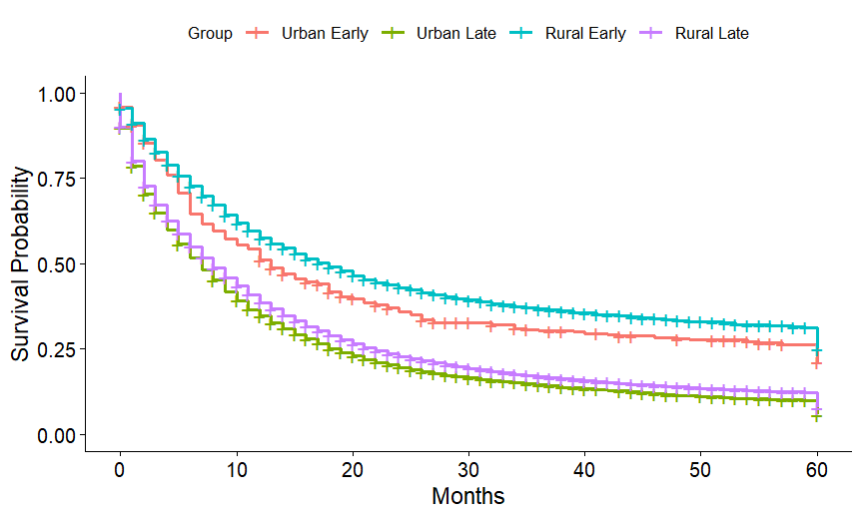
Figure: Figure 1 - 5-Year Kaplan-Meier Survival Curve by Rurality and Onset Type
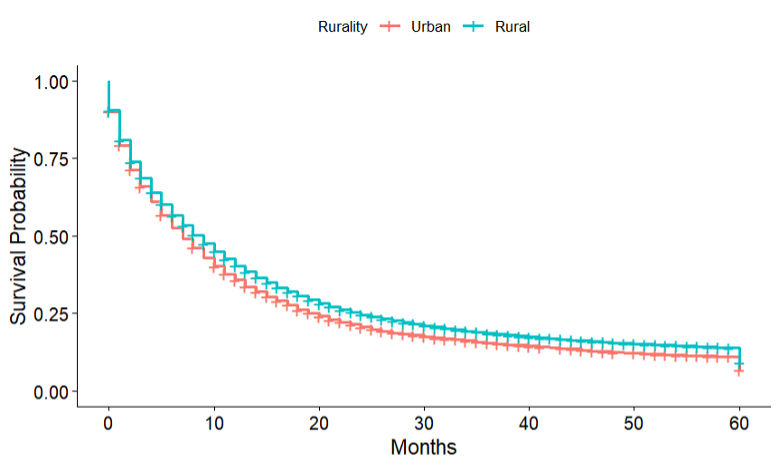
Figure: Figure 2 - 5-year Kaplan-Meier Survival Curve by Rurality
Disclosures:
Ooreoluwa Fasola indicated no relevant financial relationships.
Eunice Aregbesola indicated no relevant financial relationships.
Gloria Erazo indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Guy Loic Nguefang Tchoukeu indicated no relevant financial relationships.
Godfrey Tabowei indicated no relevant financial relationships.
Eunice Omeludike indicated no relevant financial relationships.
Ooreoluwa Fasola, MD1, Eunice Aregbesola, MD2, Gloria Erazo, MD3, Anjul Verma, MD3, Guy Loic Nguefang Tchoukeu, MD3, Godfrey Tabowei, MD4, Eunice Omeludike, MD5. P2154 - Impact of Rurality and Age at Onset on Pancreatic Cancer Survival: A Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX; 2University of Missouri , Columbia, Columbia, MO; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Texas Tech University Health Science center, Permian Basin, Odessa, TX; 5Piedmont Athens Regional Medical Centre, Athens, GA
Introduction: Pancreatic cancer is the third leading cause of cancer-related mortality, with increasing incidence and mortality among individuals younger than 50 years. However, the combined impact of rural residence and age at diagnosis on survival outcomes remains unclear. This study aimed to evaluate whether rurality influences survival in early-onset (< 50 years) and late-onset ( >50 years) pancreatic cancer using a population-based dataset.
Methods: We used the Surveillance, Epidemiology and End Results (SEER) database to identify patients aged 20–79 years diagnosed with pancreatic cancer between 2000 and 2020, categorizing them as early-onset (20–49 years) or late-onset (50–79 years). Rural versus urban residence was determined using SEER rural-urban continuum codes. Kaplan–Meier analysis was used to compare survival, and multivariable Cox proportional hazards models assessed the impact of rurality on survival, adjusting for potential confounders. An interaction term tested whether rurality and age at onset had a combined effect on survival.
Results: Of 34,996 patients, 3,000 had early-onset pancreatic cancer and 31,996 had late-onset disease. Among early-onset patients, 88.2% resided in urban areas, compared to 84.9% of those with late-onset disease. Five-year survival was lower in rural than urban residents for both early-onset (26% vs. 31.2%) and late-onset cases (9.8% vs. 12.1%) (Figure 1). In adjusted analyses, urban residents had a lower risk of death than rural residents (aHR 0.93; 95% CI 0.91–0.97; p < 0.001) (Figure 2). Late-onset patients had a significantly higher mortality risk than early-onset patients (aHR 10.66; 95% CI 5.00–24.84; p < 0.001). The interaction between rurality and age at onset was not statistically significant (aHR 1.02; 95% CI 0.89–1.16; p = 0.775), suggesting independent effects.
Discussion: Rural residence is associated with poorer 5-year survival in pancreatic cancer, independent of age at diagnosis. These findings underscore the urgent need for equitable healthcare access and targeted interventions in rural populations.
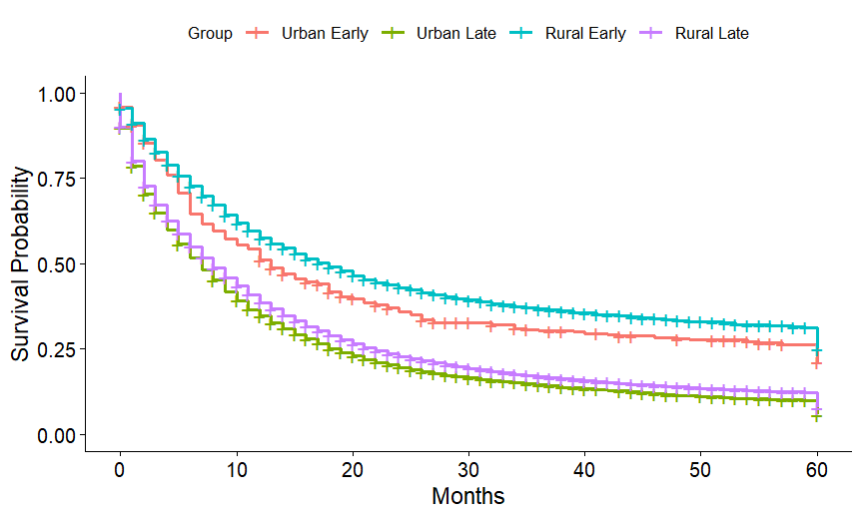
Figure: Figure 1 - 5-Year Kaplan-Meier Survival Curve by Rurality and Onset Type
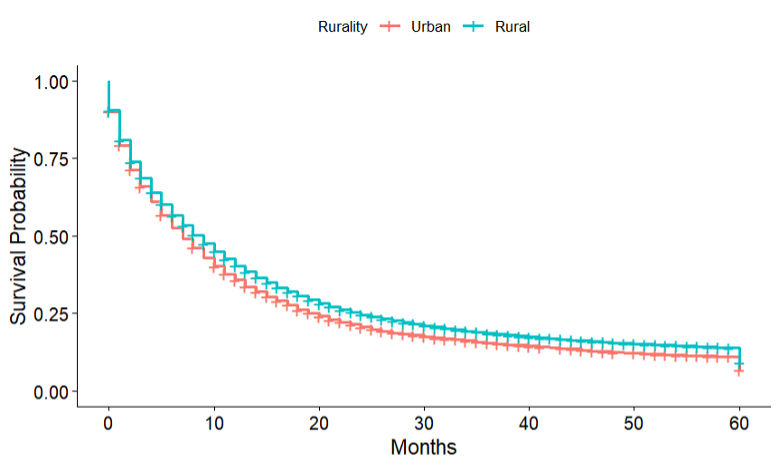
Figure: Figure 2 - 5-year Kaplan-Meier Survival Curve by Rurality
Disclosures:
Ooreoluwa Fasola indicated no relevant financial relationships.
Eunice Aregbesola indicated no relevant financial relationships.
Gloria Erazo indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Guy Loic Nguefang Tchoukeu indicated no relevant financial relationships.
Godfrey Tabowei indicated no relevant financial relationships.
Eunice Omeludike indicated no relevant financial relationships.
Ooreoluwa Fasola, MD1, Eunice Aregbesola, MD2, Gloria Erazo, MD3, Anjul Verma, MD3, Guy Loic Nguefang Tchoukeu, MD3, Godfrey Tabowei, MD4, Eunice Omeludike, MD5. P2154 - Impact of Rurality and Age at Onset on Pancreatic Cancer Survival: A Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
