Monday Poster Session
Category: Biliary/Pancreas
P2141 - Academic Advantage? Evaluating Acute Cholangitis Outcomes by Hospital Teaching Status: A Nationwide Propensity Score Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Karan J. Yagnik, MD (he/him/his)
Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University
Long Branch, NJ
Presenting Author(s)
Karan J.. Yagnik, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Charmy Parikh, MD4, Pranav Patel, MD5, Yash Shah, MD6, Umar Hayat, MD7, Dushyant S. Dahiya, MD8, Dhruvil Radadiya, MD9, Hareesha Rishab Bharadwaj, 10, Doantrang Du, MD1, Ben Terrany, MD1, Dhramesh Kaswala, MD1, Bradley D. Confer, DO5, Harshit S. Khara, MD11
1Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 2St. Mary Medical Center, Langhorne, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Mercy Catholic Medical Center, Darby, PA; 5Geisinger Health System, Danville, PA; 6Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 7Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 8University of Kansas School of Medicine, Kansas City, KS; 9Cedars-Sinai Medical Center, Los Angeles, CA; 10The University of Manchester, Manchester, England, United Kingdom; 11Geisinger Health System, Danville, NJ
Introduction: Acute cholangitis (AC) is a serious condition caused by partial or complete obstruction of the common bile duct (CBD), leading to biliary tract infection. We aimed to evaluate whether teaching hospitals with trainees and nonteaching hospitals impact the outcome of acute cholangitis in the United States.
Methods: This study utilized the National Inpatient Sample database to analyze adult hospitalizations with a primary diagnosis of acute cholangitis in the U.S. from 2016–2020. A multivariate logistic regression along with chi-square and T-test were performed using SAS 9.4 software to analyze inpatient acute cholangitis-associated mortality, inflation-adjusted total hospital charge (THC), length of stay (LOS), incidence of septic shock, need for ICU, intubation, CVC placement as well as ERCP utilization in US teaching and non-teaching hospitals during the study period.
Results: This study included a total of 30,300 patients, out of them 23,535 (~78%) were managed in teaching hospitals and 6765 (~22%) were managed in non-teaching hospitals. Primary outcomes showed a significant increase in mortality for patients managed in teaching hospitals (2.77% vs 2.08%, p=0.01) in comparison to non-teaching hospitals, hospital LOS was slightly higher in teaching hospitals (5 days (IQR: 3-6) vs 4 days (IQR: 3-8)) and so did hospital cost ($15,259 vs $14,506) in comparison to non-teaching hospitals. Secondary outcomes showed patients in teaching hospitals had higher incidence of septic shock (16.06% vs 12.53%, p< 0.0001), ICU admissions (6.61% vs 5.07%, p=0.0002), intubation (5.30% vs 3.46%, p< 0.0001) in comparison to non-teaching hospitals. However, there was no significant difference found in between two groups for CVC placement and ERCP utilization.
Discussion: Our study found higher mortality rates for acute cholangitis patients in teaching hospitals compared to non-teaching hospitals. Teaching hospitals also had higher rates of septic shock, ICU admission, and intubation, with no difference in ERCP use. These differences could be due to several factors, such as greater resident and fellow autonomy in teaching hospitals and a potentially more proactive approach by physicians in non-teaching hospitals. Additionally, teaching hospitals often manage more complex, higher-acuity cases, which could contribute to worse outcomes.
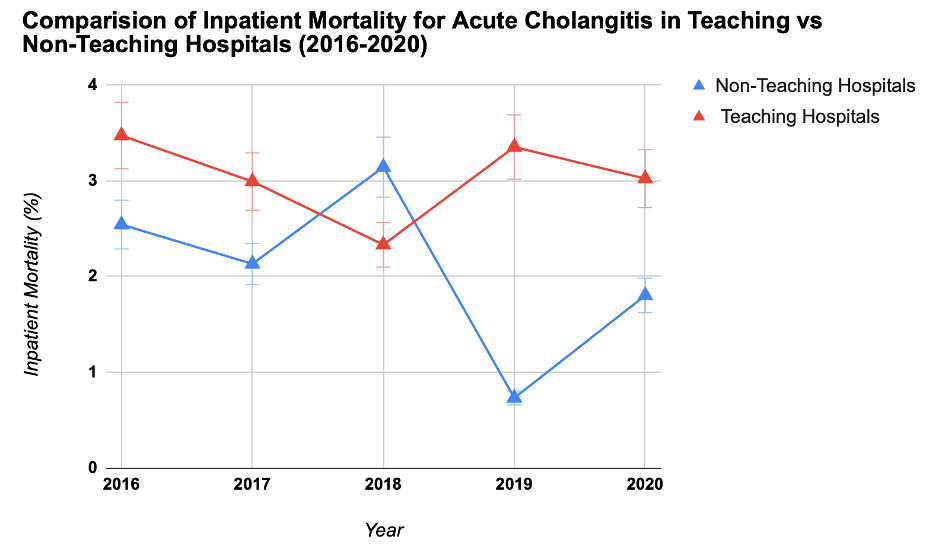
Figure: Comparison of in-patient mortality in acute cholangitis in teaching vs non-teaching hospitals. National inpatient sample database (2016-2020).
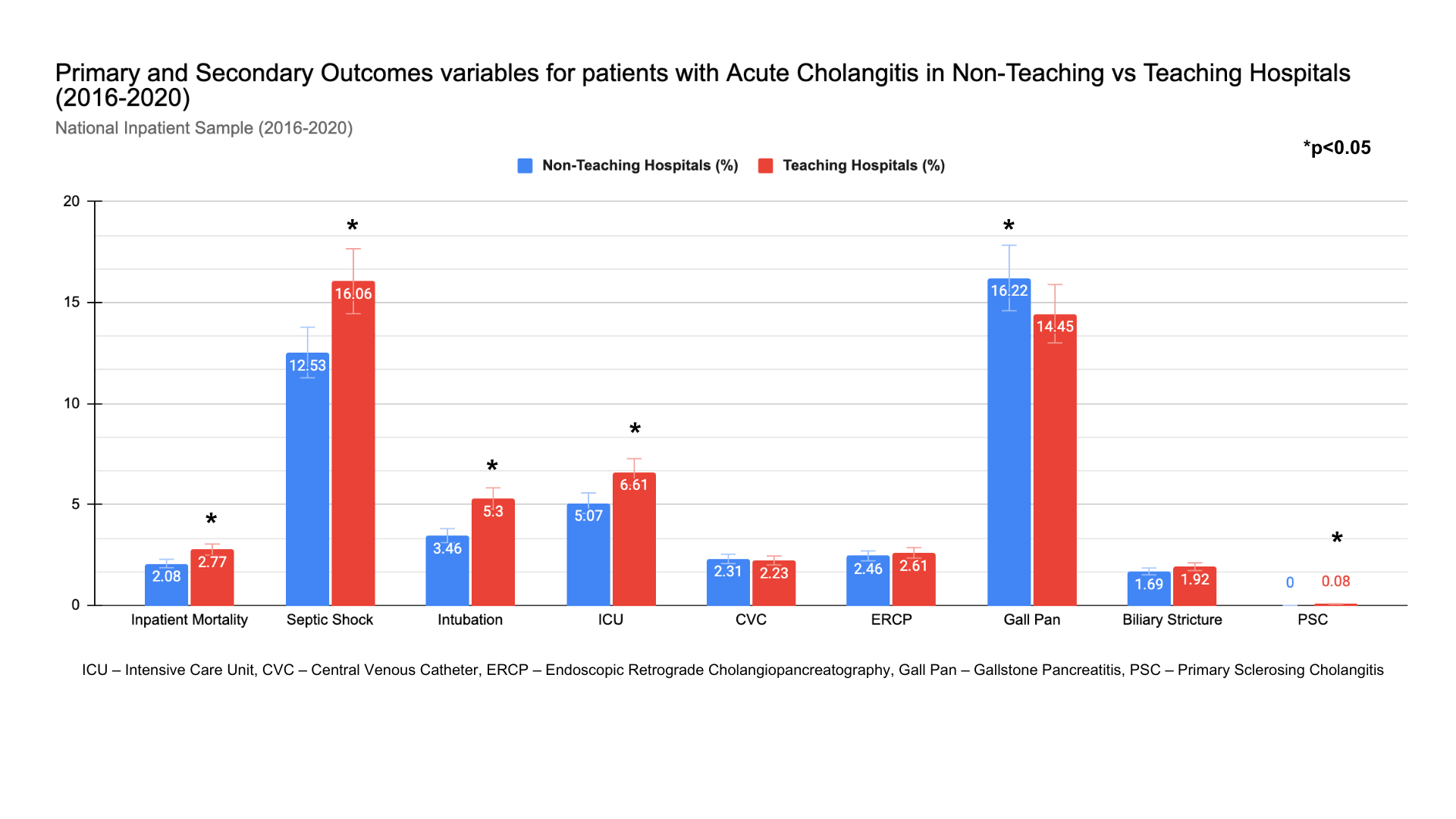
Figure: Primary and secondary outcomes of acute cholangitis: comparative analysis in between teaching and non-teaching hospitals. National inpatient sample database (2016-2020).
Disclosures:
Karan Yagnik indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Dhruvil Radadiya indicated no relevant financial relationships.
Hareesha Rishab Bharadwaj indicated no relevant financial relationships.
Doantrang Du indicated no relevant financial relationships.
Ben Terrany indicated no relevant financial relationships.
Dhramesh Kaswala indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Karan J.. Yagnik, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Charmy Parikh, MD4, Pranav Patel, MD5, Yash Shah, MD6, Umar Hayat, MD7, Dushyant S. Dahiya, MD8, Dhruvil Radadiya, MD9, Hareesha Rishab Bharadwaj, 10, Doantrang Du, MD1, Ben Terrany, MD1, Dhramesh Kaswala, MD1, Bradley D. Confer, DO5, Harshit S. Khara, MD11. P2141 - Academic Advantage? Evaluating Acute Cholangitis Outcomes by Hospital Teaching Status: A Nationwide Propensity Score Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 2St. Mary Medical Center, Langhorne, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Mercy Catholic Medical Center, Darby, PA; 5Geisinger Health System, Danville, PA; 6Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 7Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 8University of Kansas School of Medicine, Kansas City, KS; 9Cedars-Sinai Medical Center, Los Angeles, CA; 10The University of Manchester, Manchester, England, United Kingdom; 11Geisinger Health System, Danville, NJ
Introduction: Acute cholangitis (AC) is a serious condition caused by partial or complete obstruction of the common bile duct (CBD), leading to biliary tract infection. We aimed to evaluate whether teaching hospitals with trainees and nonteaching hospitals impact the outcome of acute cholangitis in the United States.
Methods: This study utilized the National Inpatient Sample database to analyze adult hospitalizations with a primary diagnosis of acute cholangitis in the U.S. from 2016–2020. A multivariate logistic regression along with chi-square and T-test were performed using SAS 9.4 software to analyze inpatient acute cholangitis-associated mortality, inflation-adjusted total hospital charge (THC), length of stay (LOS), incidence of septic shock, need for ICU, intubation, CVC placement as well as ERCP utilization in US teaching and non-teaching hospitals during the study period.
Results: This study included a total of 30,300 patients, out of them 23,535 (~78%) were managed in teaching hospitals and 6765 (~22%) were managed in non-teaching hospitals. Primary outcomes showed a significant increase in mortality for patients managed in teaching hospitals (2.77% vs 2.08%, p=0.01) in comparison to non-teaching hospitals, hospital LOS was slightly higher in teaching hospitals (5 days (IQR: 3-6) vs 4 days (IQR: 3-8)) and so did hospital cost ($15,259 vs $14,506) in comparison to non-teaching hospitals. Secondary outcomes showed patients in teaching hospitals had higher incidence of septic shock (16.06% vs 12.53%, p< 0.0001), ICU admissions (6.61% vs 5.07%, p=0.0002), intubation (5.30% vs 3.46%, p< 0.0001) in comparison to non-teaching hospitals. However, there was no significant difference found in between two groups for CVC placement and ERCP utilization.
Discussion: Our study found higher mortality rates for acute cholangitis patients in teaching hospitals compared to non-teaching hospitals. Teaching hospitals also had higher rates of septic shock, ICU admission, and intubation, with no difference in ERCP use. These differences could be due to several factors, such as greater resident and fellow autonomy in teaching hospitals and a potentially more proactive approach by physicians in non-teaching hospitals. Additionally, teaching hospitals often manage more complex, higher-acuity cases, which could contribute to worse outcomes.
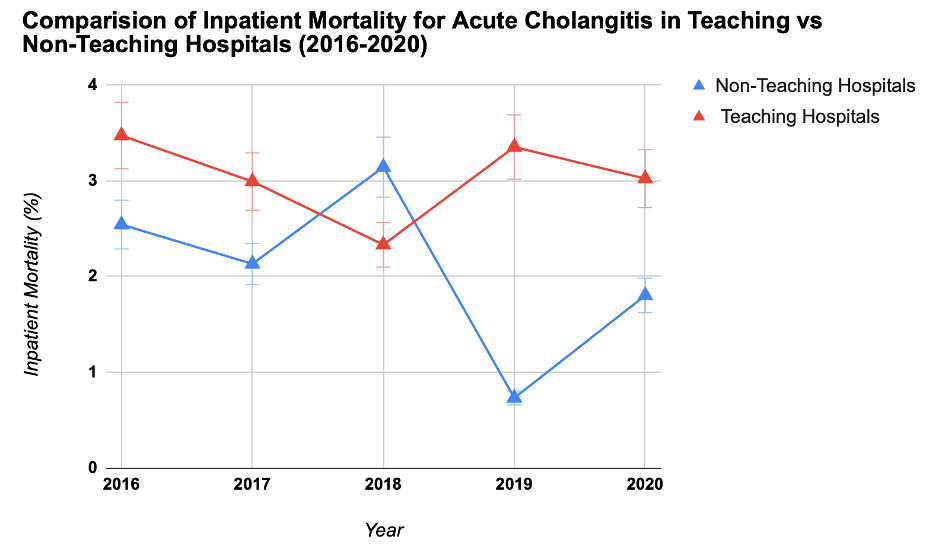
Figure: Comparison of in-patient mortality in acute cholangitis in teaching vs non-teaching hospitals. National inpatient sample database (2016-2020).
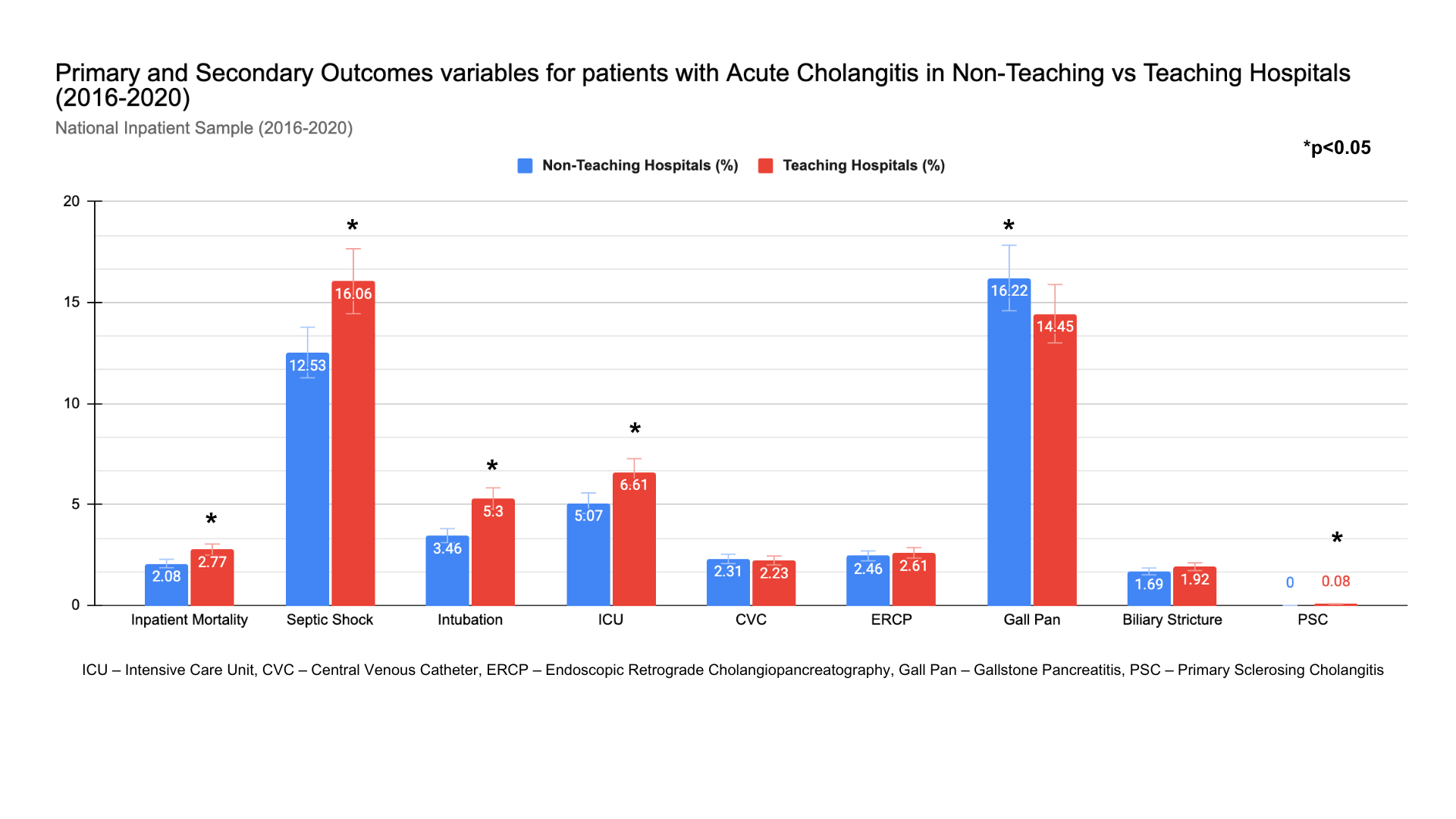
Figure: Primary and secondary outcomes of acute cholangitis: comparative analysis in between teaching and non-teaching hospitals. National inpatient sample database (2016-2020).
Disclosures:
Karan Yagnik indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Dhruvil Radadiya indicated no relevant financial relationships.
Hareesha Rishab Bharadwaj indicated no relevant financial relationships.
Doantrang Du indicated no relevant financial relationships.
Ben Terrany indicated no relevant financial relationships.
Dhramesh Kaswala indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Karan J.. Yagnik, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Charmy Parikh, MD4, Pranav Patel, MD5, Yash Shah, MD6, Umar Hayat, MD7, Dushyant S. Dahiya, MD8, Dhruvil Radadiya, MD9, Hareesha Rishab Bharadwaj, 10, Doantrang Du, MD1, Ben Terrany, MD1, Dhramesh Kaswala, MD1, Bradley D. Confer, DO5, Harshit S. Khara, MD11. P2141 - Academic Advantage? Evaluating Acute Cholangitis Outcomes by Hospital Teaching Status: A Nationwide Propensity Score Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
