Sunday Poster Session
Category: Stomach and Spleen
P2125 - Early Gastric Cancer in a Post-Liver Transplant Patient: The Role of Advanced Endoscopic Techniques
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Joselyn De Jesus-Gonzalez, MD (she/her/hers)
Ponce Health Sciences University
Ponce, PR
Presenting Author(s)
Joselyn De Jesus-Gonzalez, MD1, Barbara Rosado-Carrion, MD2
1Ponce Health Sciences University, Ponce, Puerto Rico; 2Ponce Health Sciences University, School of Medicine, Ponce, Puerto Rico
Introduction: Early gastric cancer in immunosuppressed patients may present with subtle mucosal changes that are easily missed on routine endoscopy. Liver transplant recipients on chronic immunosuppression have been associated with an elevated risk of de novo malignancies, including gastrointestinal cancers. Although rare, this complication contributes to late morbidity and mortality in this population and remains underreported. We report a case of early gastric cancer in a liver transplant recipient, diagnosed and managed with advanced endoscopic techniques.
Case Description/
Methods: A 79-year-old male with a pertinent history of liver transplantation in 2014 and chronic kidney disease, maintained on chronic tacrolimus and mycophenolate therapy, presented with several months of unintentional weight loss and new-onset vomiting. Initial esophagogastroduodenoscopy (EGD) revealed decreased rugal folds and pale mucosa in the gastric fundus and antrum. Histopathology demonstrated atrophic gastritis with intestinal metaplasia, along with foci of low-grade and high-grade dysplasia in the antrum. A repeated EGD utilizing magnifying endoscopy and narrow-band imaging (NBI) identified a mildly granular, friable area at the incisura angularis. Targeted biopsies confirmed adenocarcinoma arising in a background of atrophic gastritis. Helicobacter pylori testing was negative. The patient underwent endoscopic submucosal dissection (ESD), with final pathology revealing moderately differentiated gastric adenocarcinoma with negative margins and no lymphovascular invasion. Follow-up PET imaging and EGD at six months showed no evidence of recurrence.
Discussion: Gastric cancer remains an uncommon but serious post-transplant complication, particularly in patients on long-term immunosuppressive therapy. Tacrolimus-induced immunosuppression has been implicated in increasing oncogenic potential. In this case, chronic immunosuppression and atrophic gastritis likely acted independently and synergistically to promote gastric adenocarcinoma development. Advanced imaging with NBI enabled the early identification of an inconspicuous lesion on standard endoscopy. ESD offered a curative, minimally invasive treatment option, especially suitable for elderly, immunocompromised individuals with multiple comorbidities. This case emphasizes the value of advanced endoscopic imaging for early gastric cancer detection and supports the implementation of tailored cancer surveillance strategies in solid organ transplant recipients.
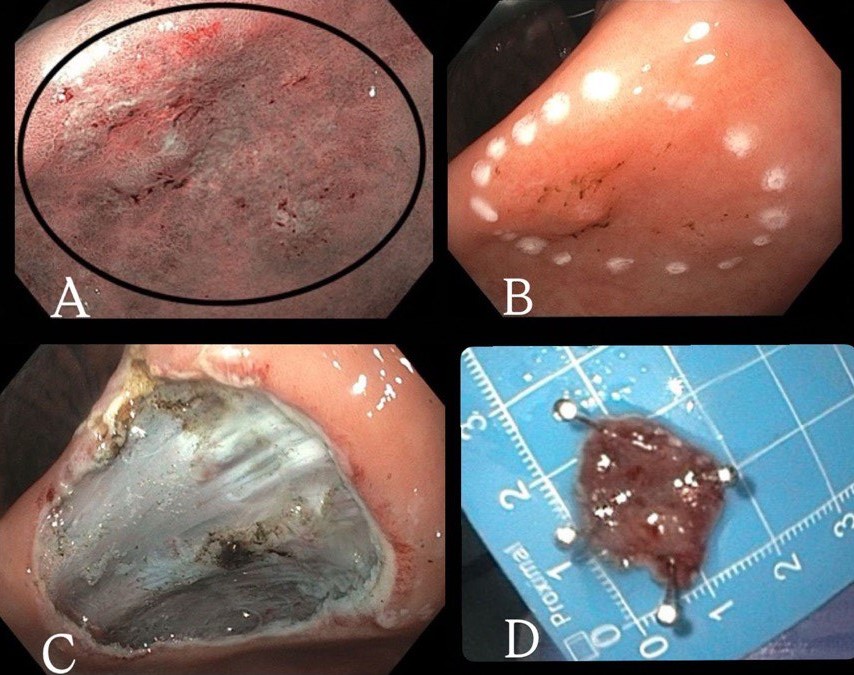
Figure: Figure 1: Endoscopic findings and treatment steps. (A) Magnifying endoscopy with narrow-band imaging findings at incisura angularis; (B) The lesion is circumferentially marked with cautery in preparation for endoscopic submucosal dissection; (C) En bloc resection is achieved using an endoscopic knife to dissect the mucosa along the previously marked margins; (D) A 2 cm segment of gastric mucosa is successfully removed.
Disclosures:
Joselyn De Jesus-Gonzalez indicated no relevant financial relationships.
Barbara Rosado-Carrion indicated no relevant financial relationships.
Joselyn De Jesus-Gonzalez, MD1, Barbara Rosado-Carrion, MD2. P2125 - Early Gastric Cancer in a Post-Liver Transplant Patient: The Role of Advanced Endoscopic Techniques, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ponce Health Sciences University, Ponce, Puerto Rico; 2Ponce Health Sciences University, School of Medicine, Ponce, Puerto Rico
Introduction: Early gastric cancer in immunosuppressed patients may present with subtle mucosal changes that are easily missed on routine endoscopy. Liver transplant recipients on chronic immunosuppression have been associated with an elevated risk of de novo malignancies, including gastrointestinal cancers. Although rare, this complication contributes to late morbidity and mortality in this population and remains underreported. We report a case of early gastric cancer in a liver transplant recipient, diagnosed and managed with advanced endoscopic techniques.
Case Description/
Methods: A 79-year-old male with a pertinent history of liver transplantation in 2014 and chronic kidney disease, maintained on chronic tacrolimus and mycophenolate therapy, presented with several months of unintentional weight loss and new-onset vomiting. Initial esophagogastroduodenoscopy (EGD) revealed decreased rugal folds and pale mucosa in the gastric fundus and antrum. Histopathology demonstrated atrophic gastritis with intestinal metaplasia, along with foci of low-grade and high-grade dysplasia in the antrum. A repeated EGD utilizing magnifying endoscopy and narrow-band imaging (NBI) identified a mildly granular, friable area at the incisura angularis. Targeted biopsies confirmed adenocarcinoma arising in a background of atrophic gastritis. Helicobacter pylori testing was negative. The patient underwent endoscopic submucosal dissection (ESD), with final pathology revealing moderately differentiated gastric adenocarcinoma with negative margins and no lymphovascular invasion. Follow-up PET imaging and EGD at six months showed no evidence of recurrence.
Discussion: Gastric cancer remains an uncommon but serious post-transplant complication, particularly in patients on long-term immunosuppressive therapy. Tacrolimus-induced immunosuppression has been implicated in increasing oncogenic potential. In this case, chronic immunosuppression and atrophic gastritis likely acted independently and synergistically to promote gastric adenocarcinoma development. Advanced imaging with NBI enabled the early identification of an inconspicuous lesion on standard endoscopy. ESD offered a curative, minimally invasive treatment option, especially suitable for elderly, immunocompromised individuals with multiple comorbidities. This case emphasizes the value of advanced endoscopic imaging for early gastric cancer detection and supports the implementation of tailored cancer surveillance strategies in solid organ transplant recipients.
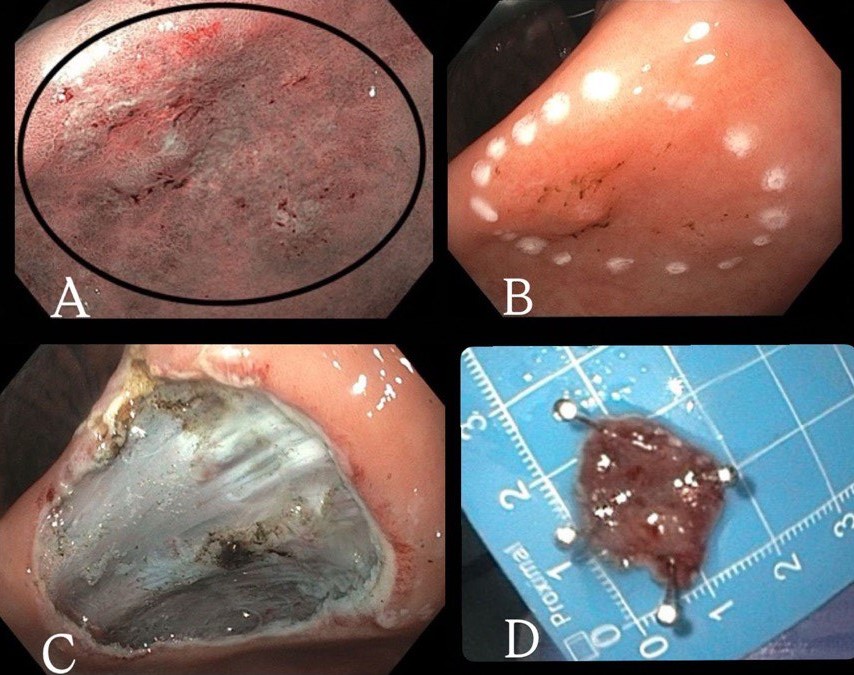
Figure: Figure 1: Endoscopic findings and treatment steps. (A) Magnifying endoscopy with narrow-band imaging findings at incisura angularis; (B) The lesion is circumferentially marked with cautery in preparation for endoscopic submucosal dissection; (C) En bloc resection is achieved using an endoscopic knife to dissect the mucosa along the previously marked margins; (D) A 2 cm segment of gastric mucosa is successfully removed.
Disclosures:
Joselyn De Jesus-Gonzalez indicated no relevant financial relationships.
Barbara Rosado-Carrion indicated no relevant financial relationships.
Joselyn De Jesus-Gonzalez, MD1, Barbara Rosado-Carrion, MD2. P2125 - Early Gastric Cancer in a Post-Liver Transplant Patient: The Role of Advanced Endoscopic Techniques, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
