Sunday Poster Session
Category: Stomach and Spleen
P2120 - A Rare Cause of Gastric Varices: Chronic Splenic Vein Thrombosis Leading to Sinistral Portal Hypertension
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MD
Michael Dybala, MD (he/him/his)
McGaw Medical Center of Northwestern University
Chicago, IL
Presenting Author(s)
Michael Dybala, MD
McGaw Medical Center of Northwestern University, Chicago, IL
Introduction: Sinistral portal hypertension is a rare cause of upper GI bleeding that occurs with occlusion of the splenic vein, mostly commonly due to pancreatic pathology. Rarely, sinistral portal hypertension can lead to collateral venous tracts, splenomegaly, and gastric varices, which can be life-threatening. Here, I describe a case of isolated gastric varices from sinistral portal hypertension arising from chronic splenic vein occlusion in a young patient with a history of Hodgkin lymphoma. This case highlights an unusual cause of varices and sinistral portal hypertension as well as novel therapies to treat variceal bleeding and prevent recurrence.
Case Description/
Methods: A 25-year-old female with a history of Hodgkin lymphoma in remission presented with dyspnea, melena, and abdominal pain. She was referred to the ED following after a hemoglobin of 6.2 g/dL was obtained on routine outpatient labs. Esophagogastroduodenoscopy revealed large, likely isolated gastric varices type 1 in the fundus and body of the stomach with possible stigmata of recent hemorrhage. Subsequent CT of the abdomen revealed midportion splenic vein occlusion with perisplenic and submucosal gastric varices as well as large collaterals extending from the splenic hilum to the SMV. Interventional radiology performed splenic venography and angioplasty with stent placement covering a 4 cm portion of narrowed splenic vein. Mechanical balloon thrombectomy and suction thrombectomy were performed after splenic vein stent placement. The patient was initiated on anticoagulation and discharged home. A triple phase CT of the liver one month after stent placement demonstrated a patent splenic vein stent and persistent abdominal venous collaterals and splenomegaly, and she has had no recurrent melena.
Discussion: Sinistral portal hypertension is most commonly associated with splenic vein occlusion due to pancreatic pathology. This patient’s chronic splenic vein occlusion was likely related to her history of Hodgkin lymphoma, which included retroperitoneal and mesenteric lymphadenopathy and notably encasement of the splenic artery and vein by a lymphomatous gastric mass. The lymphadenopathy and gastric mass improved with treatment, though sequelae remained, including splenic vein occlusion and venous collaterals. This case demonstrates both complications of splenic vein occlusion from intra-abdominal malignancy as well as a potential therapy via endovascular intervention, which is less invasive than splenic artery embolization or splenectomy.
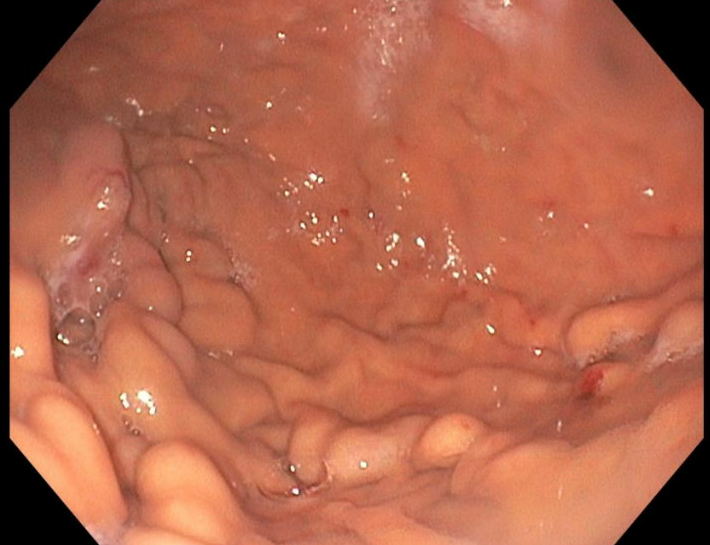
Figure: Image of the stomach from esophagogastroduodenoscopy revealing large varices in the stomach including fundus and body on the greater curvature with possible stigmata of recent hemorrhage, including scant amount of blood near varices
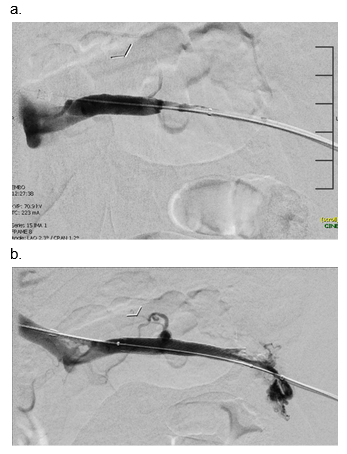
Figure: Fluoroscopic images of splenic vein venography a. Fluoroscopic image of contrast injection into the splenic vein demonstrating splenic vein occlusion b. Fluoroscopic image of contrast injection into the splenic vein after balloon angioplasty and uncovered stent placement demonstrating splenic vein patency
Disclosures:
Michael Dybala indicated no relevant financial relationships.
Michael Dybala, MD. P2120 - A Rare Cause of Gastric Varices: Chronic Splenic Vein Thrombosis Leading to Sinistral Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
McGaw Medical Center of Northwestern University, Chicago, IL
Introduction: Sinistral portal hypertension is a rare cause of upper GI bleeding that occurs with occlusion of the splenic vein, mostly commonly due to pancreatic pathology. Rarely, sinistral portal hypertension can lead to collateral venous tracts, splenomegaly, and gastric varices, which can be life-threatening. Here, I describe a case of isolated gastric varices from sinistral portal hypertension arising from chronic splenic vein occlusion in a young patient with a history of Hodgkin lymphoma. This case highlights an unusual cause of varices and sinistral portal hypertension as well as novel therapies to treat variceal bleeding and prevent recurrence.
Case Description/
Methods: A 25-year-old female with a history of Hodgkin lymphoma in remission presented with dyspnea, melena, and abdominal pain. She was referred to the ED following after a hemoglobin of 6.2 g/dL was obtained on routine outpatient labs. Esophagogastroduodenoscopy revealed large, likely isolated gastric varices type 1 in the fundus and body of the stomach with possible stigmata of recent hemorrhage. Subsequent CT of the abdomen revealed midportion splenic vein occlusion with perisplenic and submucosal gastric varices as well as large collaterals extending from the splenic hilum to the SMV. Interventional radiology performed splenic venography and angioplasty with stent placement covering a 4 cm portion of narrowed splenic vein. Mechanical balloon thrombectomy and suction thrombectomy were performed after splenic vein stent placement. The patient was initiated on anticoagulation and discharged home. A triple phase CT of the liver one month after stent placement demonstrated a patent splenic vein stent and persistent abdominal venous collaterals and splenomegaly, and she has had no recurrent melena.
Discussion: Sinistral portal hypertension is most commonly associated with splenic vein occlusion due to pancreatic pathology. This patient’s chronic splenic vein occlusion was likely related to her history of Hodgkin lymphoma, which included retroperitoneal and mesenteric lymphadenopathy and notably encasement of the splenic artery and vein by a lymphomatous gastric mass. The lymphadenopathy and gastric mass improved with treatment, though sequelae remained, including splenic vein occlusion and venous collaterals. This case demonstrates both complications of splenic vein occlusion from intra-abdominal malignancy as well as a potential therapy via endovascular intervention, which is less invasive than splenic artery embolization or splenectomy.
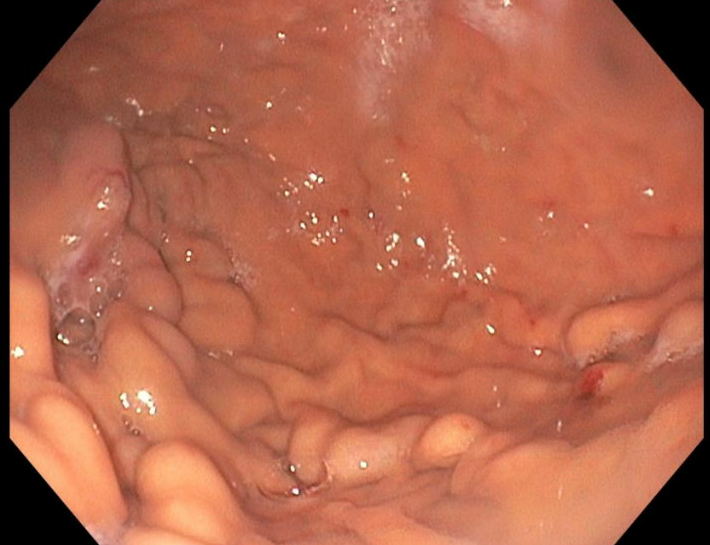
Figure: Image of the stomach from esophagogastroduodenoscopy revealing large varices in the stomach including fundus and body on the greater curvature with possible stigmata of recent hemorrhage, including scant amount of blood near varices
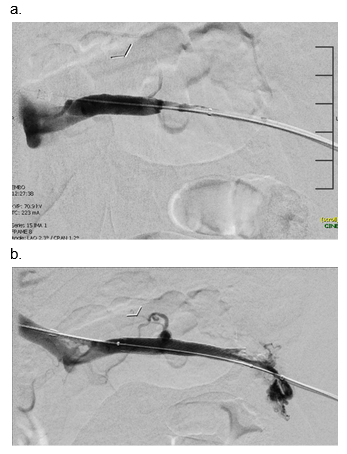
Figure: Fluoroscopic images of splenic vein venography a. Fluoroscopic image of contrast injection into the splenic vein demonstrating splenic vein occlusion b. Fluoroscopic image of contrast injection into the splenic vein after balloon angioplasty and uncovered stent placement demonstrating splenic vein patency
Disclosures:
Michael Dybala indicated no relevant financial relationships.
Michael Dybala, MD. P2120 - A Rare Cause of Gastric Varices: Chronic Splenic Vein Thrombosis Leading to Sinistral Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
