Sunday Poster Session
Category: Stomach and Spleen
P2080 - Collagenous Gastritis as a Presentation of Iron Deficiency Anemia: A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Juan Jose Chaves, MD
Norwalk Hospital
Norwalk, CT
Presenting Author(s)
Juan Jose Chaves, MD, Triston Berger, MD, Jenny Joseph, MBBS, Reid Hopkins, MD
Norwalk Hospital, Norwalk, CT
Introduction: Collagenous gastritis (CG) is a type of collagenous gastroenteritis. It is a rare disease with an estimated incidence of 13 cases per 100,000 esophagogastroduodenoscopies (EGD). Due to its nonspecific symptoms, CG poses a diagnostic challenge for clinicians, and many cases are misdiagnosed. We present the case of a young man referred to gastroenterology (GI) for iron deficiency anemia (IDA) evaluation.
Case Description/
Methods: A 28-year-old man with a history of irritable bowel syndrome (IBS-C), anxiety, and depression presented with fatigue for the past 6 months associated with frequent bowel movements (Bristol-1 and 2), abdominal pain, and a feeling of incomplete evacuation. He had previously used linaclotide and sertraline. During the consultation, his vital signs were within normal limits, and a physical examination revealed pale sclera and a soft abdomen with mild tenderness in the left lower quadrant. Laboratory findings included hemoglobin 9.8 g/dL, hematocrit 34.5%, and MCV 66 fL. The iron panel showed a transferrin saturation of 6% and a ferritin level of 5 ng/mL. Vitamin B12 and folate levels were within normal limits. The EGD revealed diffuse nodular mucosa in the gastric corpus, with pathology consistent with CG and negative for H. pylori (Figure 1). Colonoscopy and computed tomography enterography were normal. Due to the absence of upper gastrointestinal symptoms, it was decided to initiate iron supplementation and conduct clinical observation. Recent laboratory tests showed resolution of IDA, and a repeat endoscopy is pending in a year.
Discussion: CG occurs predominantly in women with a bimodal age distribution (10-19 years and over 60). Its presentation is nonspecific, with abdominal pain, anemia, and diarrhea predominating. The most common, but not pathognomonic, endoscopic finding is gastric nodularity. Clinical differentials of nodular gastritis include H. pylori-associated gastritis, lymphoma, Crohn’s disease, and sarcoidosis. Its definitive diagnosis is made by histopathological analysis, with evidence of chronic inflammation in the subepithelial layer and collagen deposition in the lamina propria greater than 10 μm. The pathogenesis of the disease is unclear, making its management a clinical challenge. Sertraline has been associated with collagenous colitis; however, there are no reports of an association with CG. Further studies are needed to establish clear diagnostic criteria and identify effective treatment modalities for this less-recognized entity.
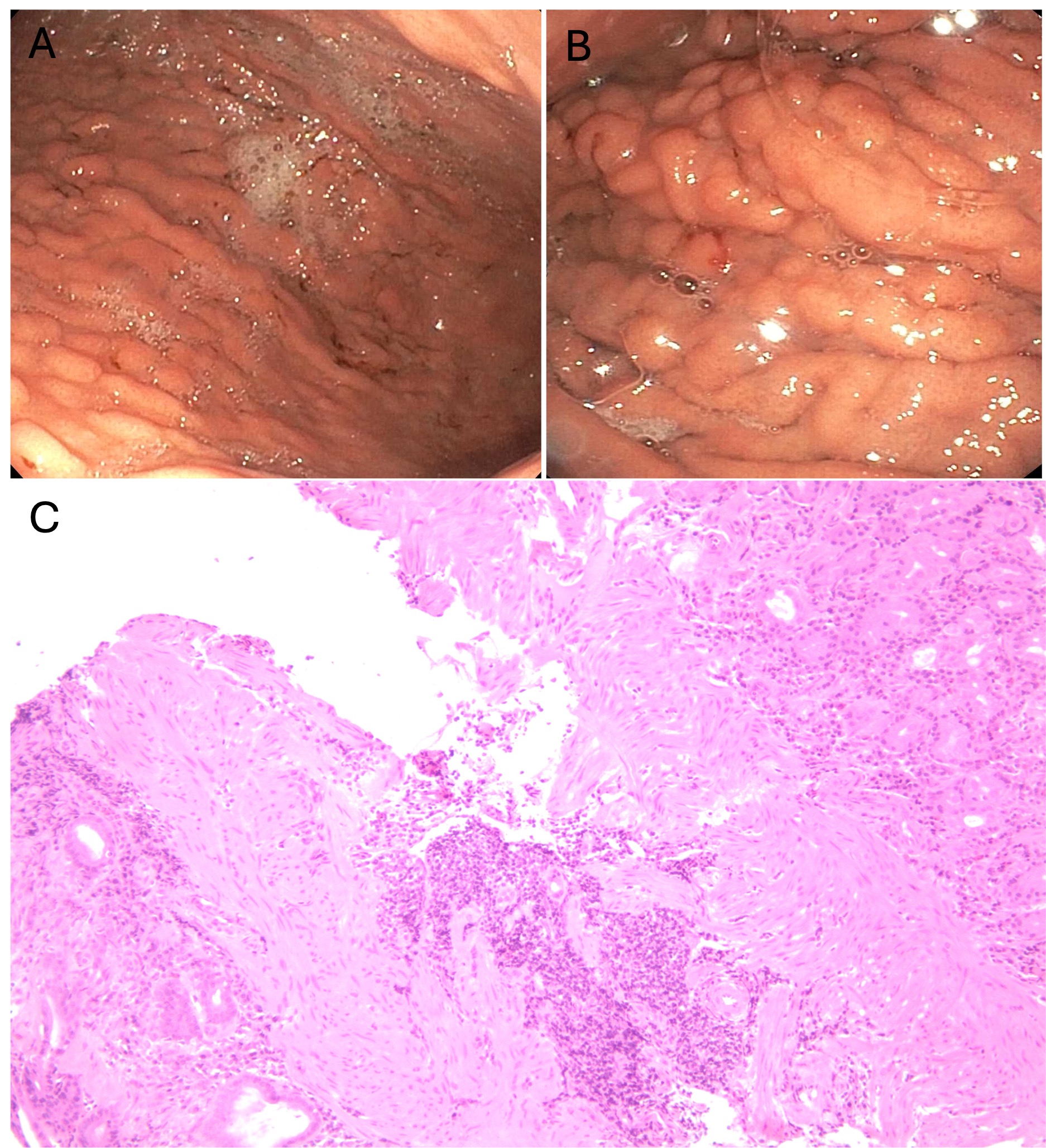
Figure: Figure 1. Endoscopic evidence of diffuse nodular mucosa in the gastric body (A and B). Gastric biopsy with increased chronic inflammatory infiltrate of the lamina propria associated with patchy increased subepithelial collagen with a thickness of up to 0.1 cm (C).
Disclosures:
Juan Jose Chaves indicated no relevant financial relationships.
Triston Berger indicated no relevant financial relationships.
Jenny Joseph indicated no relevant financial relationships.
Reid Hopkins indicated no relevant financial relationships.
Juan Jose Chaves, MD, Triston Berger, MD, Jenny Joseph, MBBS, Reid Hopkins, MD. P2080 - Collagenous Gastritis as a Presentation of Iron Deficiency Anemia: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Norwalk Hospital, Norwalk, CT
Introduction: Collagenous gastritis (CG) is a type of collagenous gastroenteritis. It is a rare disease with an estimated incidence of 13 cases per 100,000 esophagogastroduodenoscopies (EGD). Due to its nonspecific symptoms, CG poses a diagnostic challenge for clinicians, and many cases are misdiagnosed. We present the case of a young man referred to gastroenterology (GI) for iron deficiency anemia (IDA) evaluation.
Case Description/
Methods: A 28-year-old man with a history of irritable bowel syndrome (IBS-C), anxiety, and depression presented with fatigue for the past 6 months associated with frequent bowel movements (Bristol-1 and 2), abdominal pain, and a feeling of incomplete evacuation. He had previously used linaclotide and sertraline. During the consultation, his vital signs were within normal limits, and a physical examination revealed pale sclera and a soft abdomen with mild tenderness in the left lower quadrant. Laboratory findings included hemoglobin 9.8 g/dL, hematocrit 34.5%, and MCV 66 fL. The iron panel showed a transferrin saturation of 6% and a ferritin level of 5 ng/mL. Vitamin B12 and folate levels were within normal limits. The EGD revealed diffuse nodular mucosa in the gastric corpus, with pathology consistent with CG and negative for H. pylori (Figure 1). Colonoscopy and computed tomography enterography were normal. Due to the absence of upper gastrointestinal symptoms, it was decided to initiate iron supplementation and conduct clinical observation. Recent laboratory tests showed resolution of IDA, and a repeat endoscopy is pending in a year.
Discussion: CG occurs predominantly in women with a bimodal age distribution (10-19 years and over 60). Its presentation is nonspecific, with abdominal pain, anemia, and diarrhea predominating. The most common, but not pathognomonic, endoscopic finding is gastric nodularity. Clinical differentials of nodular gastritis include H. pylori-associated gastritis, lymphoma, Crohn’s disease, and sarcoidosis. Its definitive diagnosis is made by histopathological analysis, with evidence of chronic inflammation in the subepithelial layer and collagen deposition in the lamina propria greater than 10 μm. The pathogenesis of the disease is unclear, making its management a clinical challenge. Sertraline has been associated with collagenous colitis; however, there are no reports of an association with CG. Further studies are needed to establish clear diagnostic criteria and identify effective treatment modalities for this less-recognized entity.
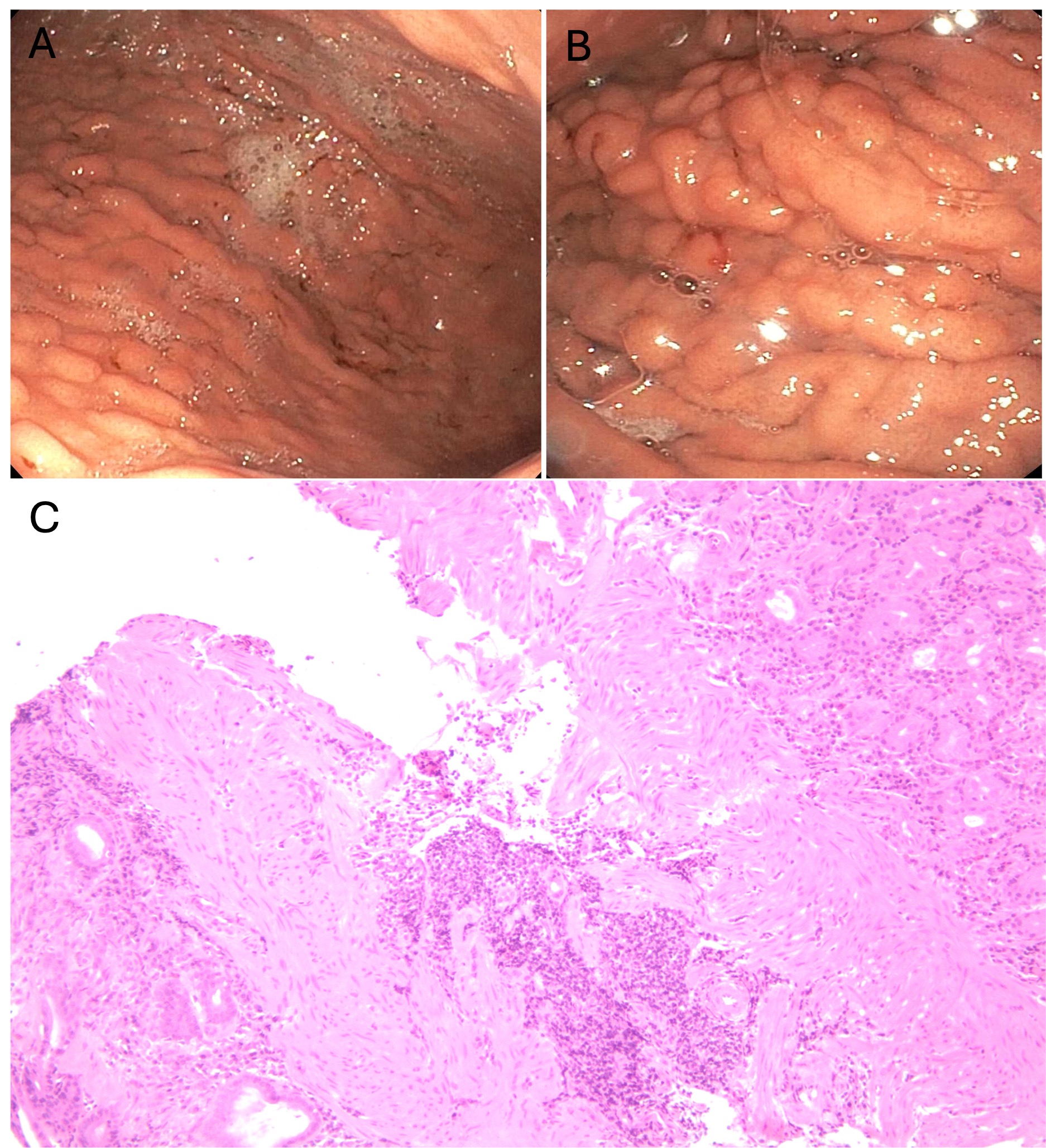
Figure: Figure 1. Endoscopic evidence of diffuse nodular mucosa in the gastric body (A and B). Gastric biopsy with increased chronic inflammatory infiltrate of the lamina propria associated with patchy increased subepithelial collagen with a thickness of up to 0.1 cm (C).
Disclosures:
Juan Jose Chaves indicated no relevant financial relationships.
Triston Berger indicated no relevant financial relationships.
Jenny Joseph indicated no relevant financial relationships.
Reid Hopkins indicated no relevant financial relationships.
Juan Jose Chaves, MD, Triston Berger, MD, Jenny Joseph, MBBS, Reid Hopkins, MD. P2080 - Collagenous Gastritis as a Presentation of Iron Deficiency Anemia: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

