Sunday Poster Session
Category: Stomach and Spleen
P2055 - Gastroparesis Impacts on Congestive Heart Failure Clinical Outcomes: Retroactive Analysis Based on the NIS Database (2020-2021)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ahmad Alnasarat, MD
SIH Memorial Hospital of Carbondale
Carbondale, IL
Presenting Author(s)
Ahmad Alnasarat, MD1, Montaser Elkholy, MD2, Mohammad Kloub, MD3, Ahmed Abdelrahman, MD4
1SIH Memorial Hospital of Carbondale, Carbondale, IL; 2DMC Sinai-Grace Hospital, Detroit, MI; 3New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 4Mount Sinai Heart Institute, Miami, FL
Introduction: Delays in gastric emptying without mechanical obstruction are the hallmark of gastroparesis, a chronic motility disorder that is more common in women and those with diabetes or other comorbidities. Both congestive heart failure (CHF) and gastroparesis are common conditions with risk factors that overlap. However, little is known about how gastroparesis affects outcomes related to CHF. In order to assess this association, we performed this retrospective study using the Nationwide Inpatient Sample (NIS).
Methods: We looked through the NIS database from 2020 to 2021 for adult patients who had gastroparesis as a secondary diagnosis and congestive heart failure (CHF) as their primary diagnosis. The Data included mortality, cardiogenic shock, length of stay (LOS), acute heart failure (AHF), acute kidney injury (AKI), hemodialysis, respiratory failure (ARF), acute cerebrovascular accident (CVA), and length of stay (LOS). After controlling for comorbidities (diabetes, chronic kidney disease, dyslipidemia, obesity, CAD, stroke, COPD, smoking, and hypertension), age, sex, and race, logistic multivariable regression models were employed.
Results: Gastroparesis was present in 20,443 (0.97%) of the 2,097,879 CHF hospitalizations. Most of these patients are older than 65. Gastroparesis was associated with lower mortality (OR 0.60, 95% CI 0.56–0.65, P < 0.0001), AKI (OR 0.80, 95% CI 0.77–0.83, P < 0.0001), AHF (OR 0.57, 95% CI 0.55–0.58, P < 0.0001), ARF (OR 0.66, 95% CI 0.63–0.69, P < 0.0001), CVA (OR 0.56, 95% CI 0.47–0.67, P < 0.0001), and cardiogenic shock (OR 0.40, 95% CI 0.35–0.45, P < 0.0001). On the other hand, gastroparesis raised the odds of LOS (OR 1.19, 95% CI 1.05–1.35, P < 0.0001) and hemodialysis (OR 1.31, 95% CI 1.25–1.36, P < 0.0001). According to demographic analysis, the prevalence was higher in older age groups (70.68% aged 65 years or older vs. 36.65% overall, P < 0.0001), males (52.57% vs. 35.55%, P < 0.0001), and Whites (67.63% vs. 54.35%, P < 0.0001). Obesity (OR 1.54) and chronic kidney disease (CKD) were significant predictors of LOS.
Discussion: Gastroparesis in hospitalized adults with CHF was linked to increased odds of hemodialysis and extended hospitalization, but decreased odds of in-hospital mortality and a number of acute complications in this sizable cohort. Further prospective research is needed to elucidate the clinical significance of these associations.
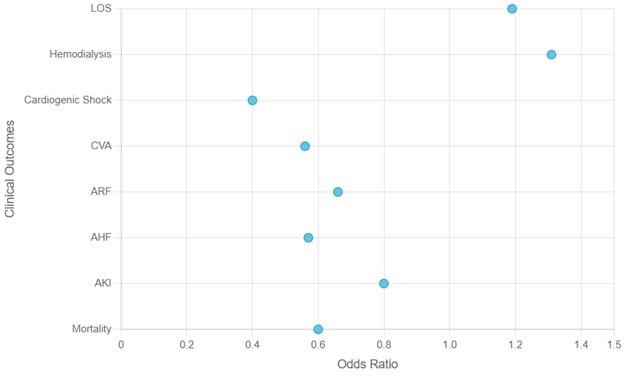
Figure: Figure1. Odds ratio of clinical outcomes

Figure: Table 1.
Disclosures:
Ahmad Alnasarat indicated no relevant financial relationships.
Montaser Elkholy indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Ahmed Abdelrahman indicated no relevant financial relationships.
Ahmad Alnasarat, MD1, Montaser Elkholy, MD2, Mohammad Kloub, MD3, Ahmed Abdelrahman, MD4. P2055 - Gastroparesis Impacts on Congestive Heart Failure Clinical Outcomes: Retroactive Analysis Based on the NIS Database (2020-2021), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SIH Memorial Hospital of Carbondale, Carbondale, IL; 2DMC Sinai-Grace Hospital, Detroit, MI; 3New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 4Mount Sinai Heart Institute, Miami, FL
Introduction: Delays in gastric emptying without mechanical obstruction are the hallmark of gastroparesis, a chronic motility disorder that is more common in women and those with diabetes or other comorbidities. Both congestive heart failure (CHF) and gastroparesis are common conditions with risk factors that overlap. However, little is known about how gastroparesis affects outcomes related to CHF. In order to assess this association, we performed this retrospective study using the Nationwide Inpatient Sample (NIS).
Methods: We looked through the NIS database from 2020 to 2021 for adult patients who had gastroparesis as a secondary diagnosis and congestive heart failure (CHF) as their primary diagnosis. The Data included mortality, cardiogenic shock, length of stay (LOS), acute heart failure (AHF), acute kidney injury (AKI), hemodialysis, respiratory failure (ARF), acute cerebrovascular accident (CVA), and length of stay (LOS). After controlling for comorbidities (diabetes, chronic kidney disease, dyslipidemia, obesity, CAD, stroke, COPD, smoking, and hypertension), age, sex, and race, logistic multivariable regression models were employed.
Results: Gastroparesis was present in 20,443 (0.97%) of the 2,097,879 CHF hospitalizations. Most of these patients are older than 65. Gastroparesis was associated with lower mortality (OR 0.60, 95% CI 0.56–0.65, P < 0.0001), AKI (OR 0.80, 95% CI 0.77–0.83, P < 0.0001), AHF (OR 0.57, 95% CI 0.55–0.58, P < 0.0001), ARF (OR 0.66, 95% CI 0.63–0.69, P < 0.0001), CVA (OR 0.56, 95% CI 0.47–0.67, P < 0.0001), and cardiogenic shock (OR 0.40, 95% CI 0.35–0.45, P < 0.0001). On the other hand, gastroparesis raised the odds of LOS (OR 1.19, 95% CI 1.05–1.35, P < 0.0001) and hemodialysis (OR 1.31, 95% CI 1.25–1.36, P < 0.0001). According to demographic analysis, the prevalence was higher in older age groups (70.68% aged 65 years or older vs. 36.65% overall, P < 0.0001), males (52.57% vs. 35.55%, P < 0.0001), and Whites (67.63% vs. 54.35%, P < 0.0001). Obesity (OR 1.54) and chronic kidney disease (CKD) were significant predictors of LOS.
Discussion: Gastroparesis in hospitalized adults with CHF was linked to increased odds of hemodialysis and extended hospitalization, but decreased odds of in-hospital mortality and a number of acute complications in this sizable cohort. Further prospective research is needed to elucidate the clinical significance of these associations.
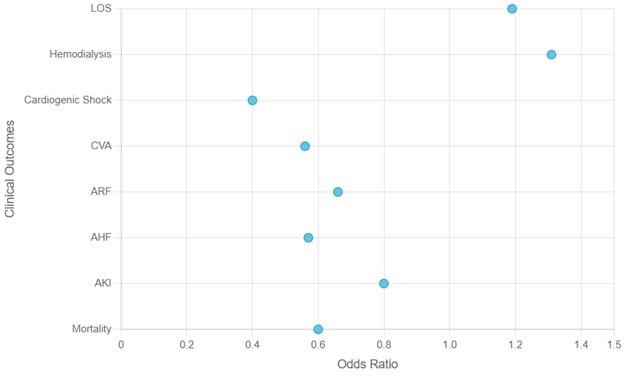
Figure: Figure1. Odds ratio of clinical outcomes

Figure: Table 1.
Disclosures:
Ahmad Alnasarat indicated no relevant financial relationships.
Montaser Elkholy indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Ahmed Abdelrahman indicated no relevant financial relationships.
Ahmad Alnasarat, MD1, Montaser Elkholy, MD2, Mohammad Kloub, MD3, Ahmed Abdelrahman, MD4. P2055 - Gastroparesis Impacts on Congestive Heart Failure Clinical Outcomes: Retroactive Analysis Based on the NIS Database (2020-2021), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
