Sunday Poster Session
Category: Stomach and Spleen
P2036 - Effect of Nutritional Deficiencies on the Complication of Gastroparesis and Hospital Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- BX
Brian Xu, MD
Morehouse School of Medicine
Atlanta, GA
Presenting Author(s)
Brian Xu, MD1, Adedeji Adenusi, MD, MPH2, Chima Amadi, MD1, Julia Liu, MD1
1Morehouse School of Medicine, Atlanta, GA; 2One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY
Introduction: Gastroparesis (GP) is a debilitating motility disorder that can cause nutritional deficiencies, negatively affecting health outcomes. Despite this, assessing nutritional deficiencies in hospitalized GP patients is not routine. This study evaluates the prevalence of these deficiencies and their impact on hospital outcomes, including length of stay (LOS).
Methods: Data from the National Inpatient Sample (2016–2020) were analyzed. GP patients were stratified into diabetic gastroparesis (DG) and non-diabetic gastroparesis (NDG). Nutritional deficiencies (vitamin D, vitamin B12, and copper) and outcomes (GERD and LOS) were examined. Chi-square tests, descriptive analyses, and logistic regressions assessed the impact of deficiencies on outcomes.
Results: A total of 263,710 patients were diagnosed with GP; 75% had DG, 25% had NDG. Among them, 33.35% had GERD, < 1% were iron- or copper-deficient, < 2% had vitamin B deficiencies, and < 4% had vitamin D deficiencies. The mean age was 53, mean hospital charges $63,974, and mean LOS 6 days. DG patients with B12 or D deficiencies were more likely to have GERD than non-deficient patients (Table 1). NDG patients with vitamin D deficiency also had increased GERD likelihood. DG patients with iron or D deficiencies had longer LOS ( >6 days), while NDG patients with B12 deficiency alone were linked to increased LOS.
Discussion: Discussion
Iron, B12, and D deficiencies are linked to GERD and/or increased LOS in GP patients. These findings align with Patel et al. (2023), who reported malnutrition in GP raised LOS risk. Similarly, Amjab et al. (2023) found GP patients had higher iron, B12, and D deficiency rates than the general population, but only 19.4% received a nutrition consult. These results suggest routine screening and supplementation of D, B12, and iron may reduce GERD complications and LOS.
Limitations
This study's retrospective design limits causal inference; using the NIS dataset may introduce coding variability. Future studies should explore whether supplementation reduces LOS and complications.
Conclusion
Nutritional deficiencies significantly impact hospitalized GP patients, highlighting the need for routine screening and intervention to improve outcomes.
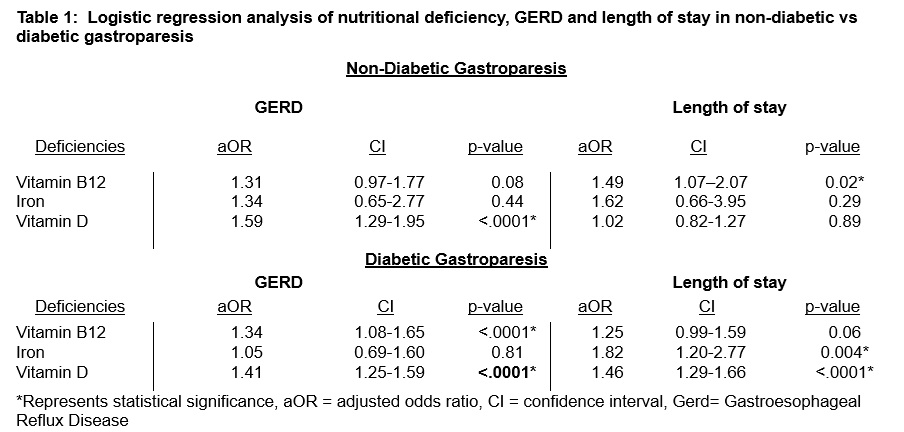
Figure: Table 1 - Logistic Regression Analysis of Nutritional Deficiency, GERD and LoS in Non-Diabetic vs Diabetic Gastroparesis
Disclosures:
Brian Xu indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Chima Amadi indicated no relevant financial relationships.
Julia Liu indicated no relevant financial relationships.
Brian Xu, MD1, Adedeji Adenusi, MD, MPH2, Chima Amadi, MD1, Julia Liu, MD1. P2036 - Effect of Nutritional Deficiencies on the Complication of Gastroparesis and Hospital Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Morehouse School of Medicine, Atlanta, GA; 2One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY
Introduction: Gastroparesis (GP) is a debilitating motility disorder that can cause nutritional deficiencies, negatively affecting health outcomes. Despite this, assessing nutritional deficiencies in hospitalized GP patients is not routine. This study evaluates the prevalence of these deficiencies and their impact on hospital outcomes, including length of stay (LOS).
Methods: Data from the National Inpatient Sample (2016–2020) were analyzed. GP patients were stratified into diabetic gastroparesis (DG) and non-diabetic gastroparesis (NDG). Nutritional deficiencies (vitamin D, vitamin B12, and copper) and outcomes (GERD and LOS) were examined. Chi-square tests, descriptive analyses, and logistic regressions assessed the impact of deficiencies on outcomes.
Results: A total of 263,710 patients were diagnosed with GP; 75% had DG, 25% had NDG. Among them, 33.35% had GERD, < 1% were iron- or copper-deficient, < 2% had vitamin B deficiencies, and < 4% had vitamin D deficiencies. The mean age was 53, mean hospital charges $63,974, and mean LOS 6 days. DG patients with B12 or D deficiencies were more likely to have GERD than non-deficient patients (Table 1). NDG patients with vitamin D deficiency also had increased GERD likelihood. DG patients with iron or D deficiencies had longer LOS ( >6 days), while NDG patients with B12 deficiency alone were linked to increased LOS.
Discussion: Discussion
Iron, B12, and D deficiencies are linked to GERD and/or increased LOS in GP patients. These findings align with Patel et al. (2023), who reported malnutrition in GP raised LOS risk. Similarly, Amjab et al. (2023) found GP patients had higher iron, B12, and D deficiency rates than the general population, but only 19.4% received a nutrition consult. These results suggest routine screening and supplementation of D, B12, and iron may reduce GERD complications and LOS.
Limitations
This study's retrospective design limits causal inference; using the NIS dataset may introduce coding variability. Future studies should explore whether supplementation reduces LOS and complications.
Conclusion
Nutritional deficiencies significantly impact hospitalized GP patients, highlighting the need for routine screening and intervention to improve outcomes.
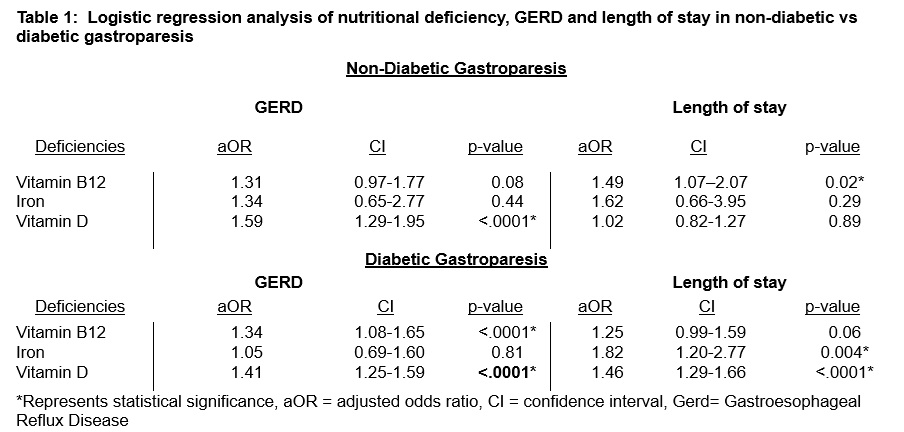
Figure: Table 1 - Logistic Regression Analysis of Nutritional Deficiency, GERD and LoS in Non-Diabetic vs Diabetic Gastroparesis
Disclosures:
Brian Xu indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Chima Amadi indicated no relevant financial relationships.
Julia Liu indicated no relevant financial relationships.
Brian Xu, MD1, Adedeji Adenusi, MD, MPH2, Chima Amadi, MD1, Julia Liu, MD1. P2036 - Effect of Nutritional Deficiencies on the Complication of Gastroparesis and Hospital Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
