Sunday Poster Session
Category: Stomach and Spleen
P2029 - Optimizing Dyspepsia Referrals: A Machine Learning Approach to Alarm Feature Detection
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Advait Suvarnakar, MD, BS
Montefiore Medical Center, Albert Einstein College of Medicine
Clifton, NJ
Presenting Author(s)
Advait Suvarnakar, MD, BS1, Akash Kumar, MD2, Faisal Nagarwala, MD3
1Montefiore Medical Center, Albert Einstein College of Medicine, Clifton, NJ; 2Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 3St. Joseph's Hospital and Medical Center, Clifton, NJ
Introduction: Dyspepsia is a common condition addressed in primary care visits. Yet, despite established clinical guidelines emphasizing alarm features and demographic parameters for endoscopic evaluations, there is a significant amount of variability in patient referrals. This ultimately leads to two critical points: over referral of low-risk patients to an already inundated system, and potential missed malignancies (approximately 11% of neoplasms are overlooked). Artificial intelligence (AI) has a role to parse through structured electronic health record (EHR) data and act as a tool to aid physicians in better sorting individuals for endoscopy. We created an AI model to identify dyspepsia patients requiring endoscopy, aiming to reduce unnecessary referrals while maintaining diagnostic safety.
Methods: We conducted a retrospective cohort study (2021-2024) of 293 patients with dyspepsia from multi-center primary care clinics and its EHR. Using Bio_ClinicalBERT, a natural language process (NLP) model, we extracted search terms such as “melena” and “unintentional weight loss”. Utilizing the XGBoost machine learning model, we combined these terms with quantifiable trends such as “hemoglobin decline >2g/dL”, “% weight loss” and “age” to create an Alarm Score. Primary endpoints include sensitivity for significant endoscopic findings, and net benefit analysis compared to actual practice.
Results: Our AI Model exhibited an improvement compared to clinical practice, achieving an area under the receiving operator curve of 0.83 (95% CI 0.81-0.85) compared to 0.76 for physician practice. Additionally, it missed 0/13 malignancies, compared to 2/13 missed in usual care (99% sensitivity). Implementation of our model would have resulted in 28% fewer overall referrals to endoscopy, from 29% to 21%. The strongest predictive factors include NLP identified weight loss documentation (OR 8.2), melena (7.3), and men over 60 with NSAID use (9.1). Average cost savings per procedure were estimated to be $1,200.
Discussion: This study presents a new AI model to triage patients with dyspepsia for endoscopic referrals. Our model’s high sensitivity addresses an important safety concern, and it’s proposed reduction in unnecessary referrals presents significant cost savings and improving physician’s workloads. A limitation is the model’s reliance on documentation quality where it may miss some colloquial terms. Future direction would be to implement clinical decision tools like our model in real time to enhance clinical judgement.
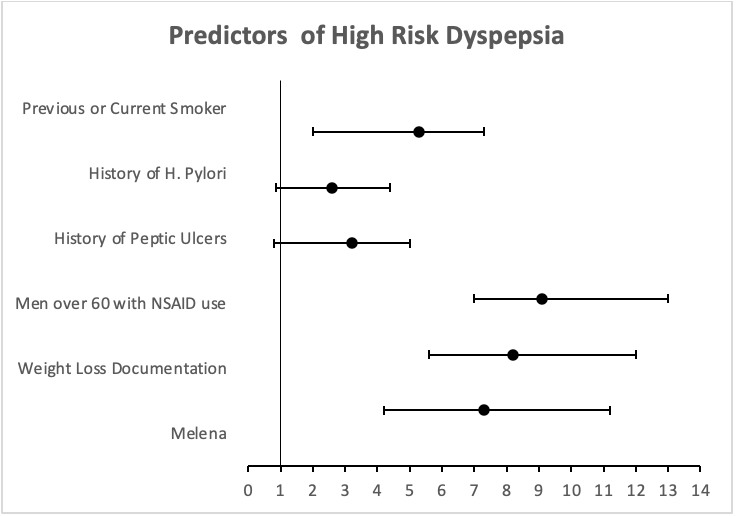
Figure: Forest plot of top predictors for high-risk dyspepsia identified by AI triage. Odds ratios (OR) with 95% confidence intervals (CI) are derived from multivariate logistic regression. Men over 60 with concurrent NSAID use (9.1)and unexplained weight loss (8.2) were highest predictors. Histories of H. Pylori and Peptic Ulcers were not significant predictors in our cohort.
Disclosures:
Advait Suvarnakar indicated no relevant financial relationships.
Akash Kumar indicated no relevant financial relationships.
Faisal Nagarwala indicated no relevant financial relationships.
Advait Suvarnakar, MD, BS1, Akash Kumar, MD2, Faisal Nagarwala, MD3. P2029 - Optimizing Dyspepsia Referrals: A Machine Learning Approach to Alarm Feature Detection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Montefiore Medical Center, Albert Einstein College of Medicine, Clifton, NJ; 2Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 3St. Joseph's Hospital and Medical Center, Clifton, NJ
Introduction: Dyspepsia is a common condition addressed in primary care visits. Yet, despite established clinical guidelines emphasizing alarm features and demographic parameters for endoscopic evaluations, there is a significant amount of variability in patient referrals. This ultimately leads to two critical points: over referral of low-risk patients to an already inundated system, and potential missed malignancies (approximately 11% of neoplasms are overlooked). Artificial intelligence (AI) has a role to parse through structured electronic health record (EHR) data and act as a tool to aid physicians in better sorting individuals for endoscopy. We created an AI model to identify dyspepsia patients requiring endoscopy, aiming to reduce unnecessary referrals while maintaining diagnostic safety.
Methods: We conducted a retrospective cohort study (2021-2024) of 293 patients with dyspepsia from multi-center primary care clinics and its EHR. Using Bio_ClinicalBERT, a natural language process (NLP) model, we extracted search terms such as “melena” and “unintentional weight loss”. Utilizing the XGBoost machine learning model, we combined these terms with quantifiable trends such as “hemoglobin decline >2g/dL”, “% weight loss” and “age” to create an Alarm Score. Primary endpoints include sensitivity for significant endoscopic findings, and net benefit analysis compared to actual practice.
Results: Our AI Model exhibited an improvement compared to clinical practice, achieving an area under the receiving operator curve of 0.83 (95% CI 0.81-0.85) compared to 0.76 for physician practice. Additionally, it missed 0/13 malignancies, compared to 2/13 missed in usual care (99% sensitivity). Implementation of our model would have resulted in 28% fewer overall referrals to endoscopy, from 29% to 21%. The strongest predictive factors include NLP identified weight loss documentation (OR 8.2), melena (7.3), and men over 60 with NSAID use (9.1). Average cost savings per procedure were estimated to be $1,200.
Discussion: This study presents a new AI model to triage patients with dyspepsia for endoscopic referrals. Our model’s high sensitivity addresses an important safety concern, and it’s proposed reduction in unnecessary referrals presents significant cost savings and improving physician’s workloads. A limitation is the model’s reliance on documentation quality where it may miss some colloquial terms. Future direction would be to implement clinical decision tools like our model in real time to enhance clinical judgement.
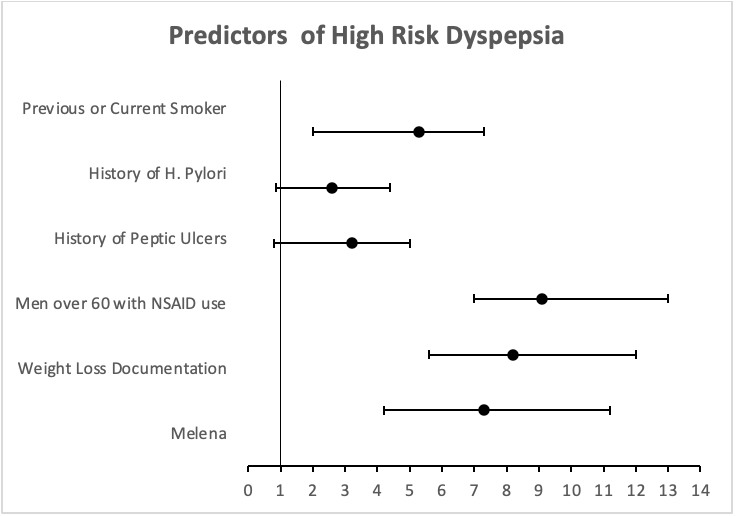
Figure: Forest plot of top predictors for high-risk dyspepsia identified by AI triage. Odds ratios (OR) with 95% confidence intervals (CI) are derived from multivariate logistic regression. Men over 60 with concurrent NSAID use (9.1)and unexplained weight loss (8.2) were highest predictors. Histories of H. Pylori and Peptic Ulcers were not significant predictors in our cohort.
Disclosures:
Advait Suvarnakar indicated no relevant financial relationships.
Akash Kumar indicated no relevant financial relationships.
Faisal Nagarwala indicated no relevant financial relationships.
Advait Suvarnakar, MD, BS1, Akash Kumar, MD2, Faisal Nagarwala, MD3. P2029 - Optimizing Dyspepsia Referrals: A Machine Learning Approach to Alarm Feature Detection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
