Sunday Poster Session
Category: Small Intestine
When Gas Crosses the Gut Wall: <i>Pneumatosis intestinalis</i> - Side Effect, Obstruction, or Ischemia?
P2005 - When Gas Crosses the Gut Wall: Pneumatosis intestinalis - Side Effect, Obstruction, or Ischemia?
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Balkrishna R. Sapariya, MBBS (he/him/his)
Western Reserve Health Education
Dayton, OH
Presenting Author(s)
Balkrishna R. Sapariya, MBBS1, Nathalie Freites Gonzalez, MD1, Nirali Sapariya, PA-C2, Larry Woods, DO1
1Western Reserve Health Education, Warren, OH; 2MetroHealth Medical Center, Cleveland, OH
Introduction: Pneumatosis intestinalis(PI) is presence of gas within intestinal wall. PI is idiopathic (15%) or secondary (85%) to GI(gastrointestinal) and non-GI illnesses. Pathogenesis of PI is multifactorial- mechanical, bacterial, and biochemical causes including lactulose. PI is a radiologic finding associated with high mortality rate 33–40% and 100% in cirrhotic patients with MELD(Model for End-Stage Liver Disease) > 16.
Case Description/
Methods: 53-year-old male with diabetes, hypothyroidism, alcoholic cirrhosis, esophageal varices, and ascites presented with altered mentation and unresponsiveness. He came from the acute long-term care facility and was on hemodialysis three times a week for acute kidney injury.
He was intubated for airway protection and transferred to critical care for Grade IV hepatic encephalopathy. His abdomen was distended, tense with stretched umbilicus. Lactulose 30g every 2 hours and rifaximin 550 mg twice daily were given. MELD was 26. (19.6% mortality in 90 days) Ultrasound showed moderately large ascites, followed by paracentesis with 4L fluid removal. Peritoneal fluid serum-ascites albumin gradient was 3.4, suggestive of portal hypertension with negative culture. Ceftriaxone was started for peritonitis prophylaxis.
Abdominal X-ray showed scattered air-fluid levels and small bowel obstruction, managed nonoperatively. 15 doses of lactulose were already given before X-ray. Blood culture was negative. Leukocytosis peaked at 37,500/uL. Lactic acid was 5.6, 2.1, and 7.6mmol/L associated with respiratory alkalosis with pH 7.44 initially and then down to 7.19. Ammonia came down from 314 to 137 by lactulose, but then rose to 623umol/L.
Bowel sounds were reduced on next day. CT scan abdomen/pelvis with contrast showed pneumatosis intestinalis involving the mid and distal small bowel- compatible with ischemia, portal venous gas, and ascites with liver cirrhosis. He deteriorated requiring 3 vasopressors. He had seizure-like activity and received benzodiazepines. Code status was changed to DNRCC due to poor prognosis. He passed away after terminal extubation.
Discussion: This case illustrates diagnostic challenges and requires an attentive approach for PI. PI on imaging with signs of peritonitis, lactic acidosis, or portal venous gas guides emergent surgical intervention. In this case, presence of multifactorial etiologies- lactulose, obstruction, and ischemia augments each other, leading to PI. High MELD-poor prognosis requires a balancing decision of emergent management versus comfort.
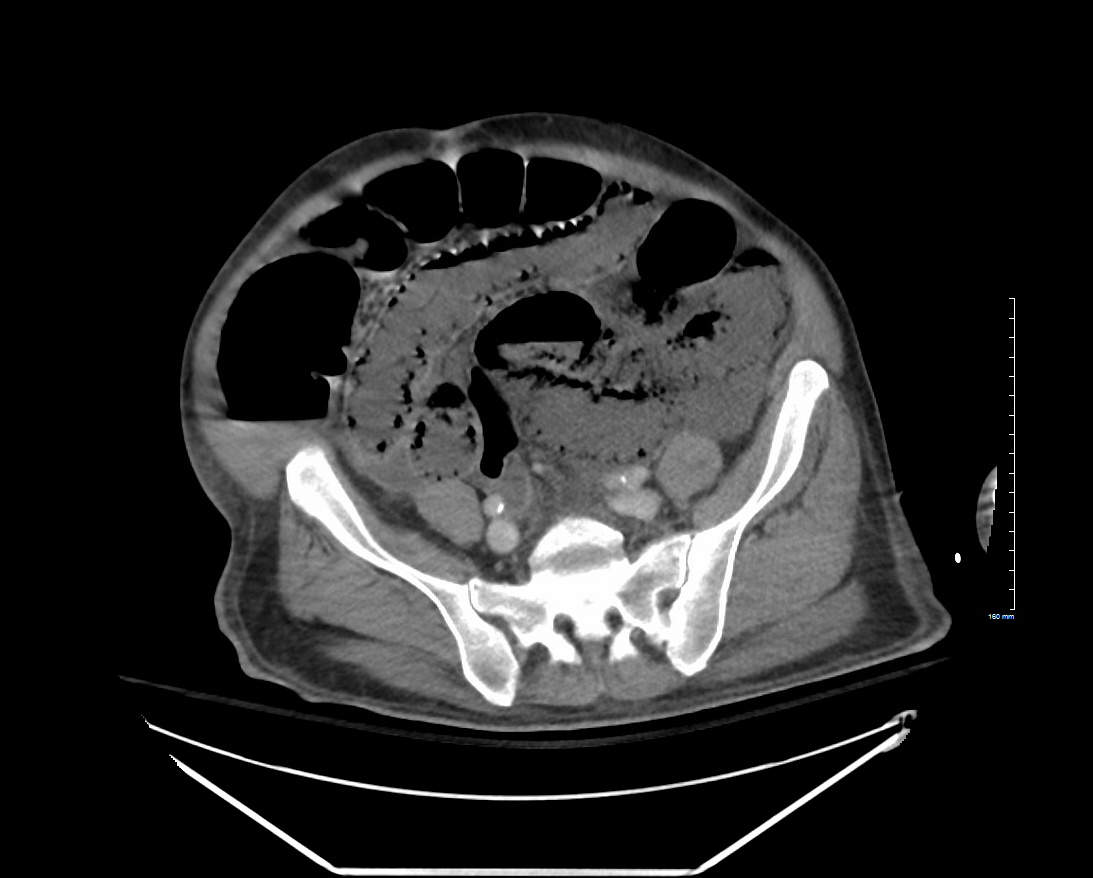
Figure: Gas in the intestinal wall on CT scan
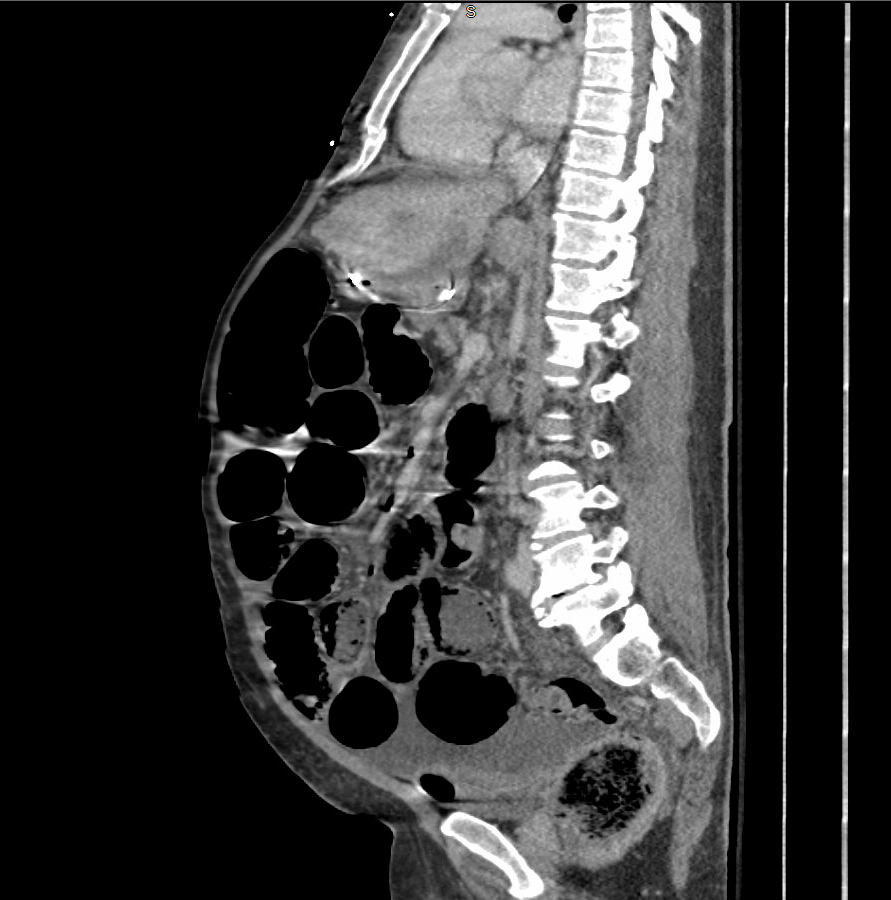
Figure: Gas in portal vein on CT scan
Disclosures:
Balkrishna Sapariya indicated no relevant financial relationships.
Nathalie Freites Gonzalez indicated no relevant financial relationships.
Nirali Sapariya indicated no relevant financial relationships.
Larry Woods indicated no relevant financial relationships.
Balkrishna R. Sapariya, MBBS1, Nathalie Freites Gonzalez, MD1, Nirali Sapariya, PA-C2, Larry Woods, DO1. P2005 - When Gas Crosses the Gut Wall: <i>Pneumatosis intestinalis</i> - Side Effect, Obstruction, or Ischemia?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Western Reserve Health Education, Warren, OH; 2MetroHealth Medical Center, Cleveland, OH
Introduction: Pneumatosis intestinalis(PI) is presence of gas within intestinal wall. PI is idiopathic (15%) or secondary (85%) to GI(gastrointestinal) and non-GI illnesses. Pathogenesis of PI is multifactorial- mechanical, bacterial, and biochemical causes including lactulose. PI is a radiologic finding associated with high mortality rate 33–40% and 100% in cirrhotic patients with MELD(Model for End-Stage Liver Disease) > 16.
Case Description/
Methods: 53-year-old male with diabetes, hypothyroidism, alcoholic cirrhosis, esophageal varices, and ascites presented with altered mentation and unresponsiveness. He came from the acute long-term care facility and was on hemodialysis three times a week for acute kidney injury.
He was intubated for airway protection and transferred to critical care for Grade IV hepatic encephalopathy. His abdomen was distended, tense with stretched umbilicus. Lactulose 30g every 2 hours and rifaximin 550 mg twice daily were given. MELD was 26. (19.6% mortality in 90 days) Ultrasound showed moderately large ascites, followed by paracentesis with 4L fluid removal. Peritoneal fluid serum-ascites albumin gradient was 3.4, suggestive of portal hypertension with negative culture. Ceftriaxone was started for peritonitis prophylaxis.
Abdominal X-ray showed scattered air-fluid levels and small bowel obstruction, managed nonoperatively. 15 doses of lactulose were already given before X-ray. Blood culture was negative. Leukocytosis peaked at 37,500/uL. Lactic acid was 5.6, 2.1, and 7.6mmol/L associated with respiratory alkalosis with pH 7.44 initially and then down to 7.19. Ammonia came down from 314 to 137 by lactulose, but then rose to 623umol/L.
Bowel sounds were reduced on next day. CT scan abdomen/pelvis with contrast showed pneumatosis intestinalis involving the mid and distal small bowel- compatible with ischemia, portal venous gas, and ascites with liver cirrhosis. He deteriorated requiring 3 vasopressors. He had seizure-like activity and received benzodiazepines. Code status was changed to DNRCC due to poor prognosis. He passed away after terminal extubation.
Discussion: This case illustrates diagnostic challenges and requires an attentive approach for PI. PI on imaging with signs of peritonitis, lactic acidosis, or portal venous gas guides emergent surgical intervention. In this case, presence of multifactorial etiologies- lactulose, obstruction, and ischemia augments each other, leading to PI. High MELD-poor prognosis requires a balancing decision of emergent management versus comfort.
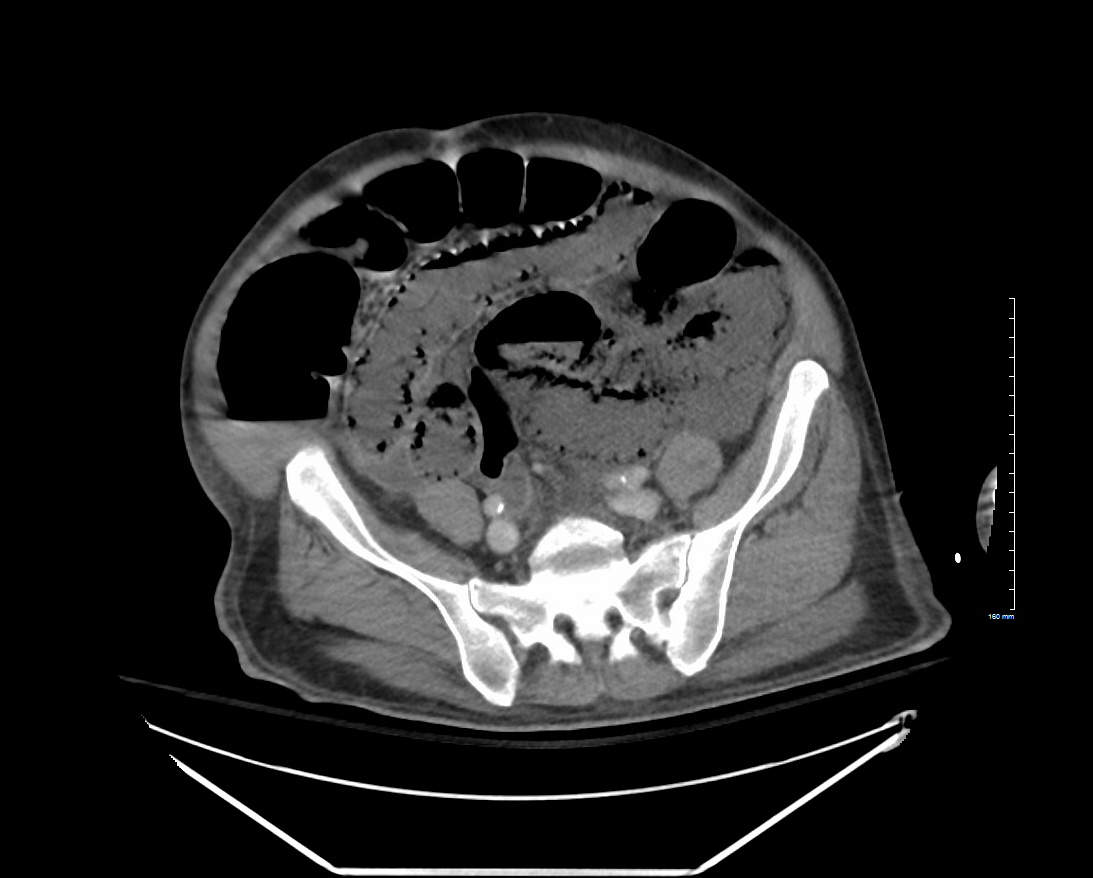
Figure: Gas in the intestinal wall on CT scan
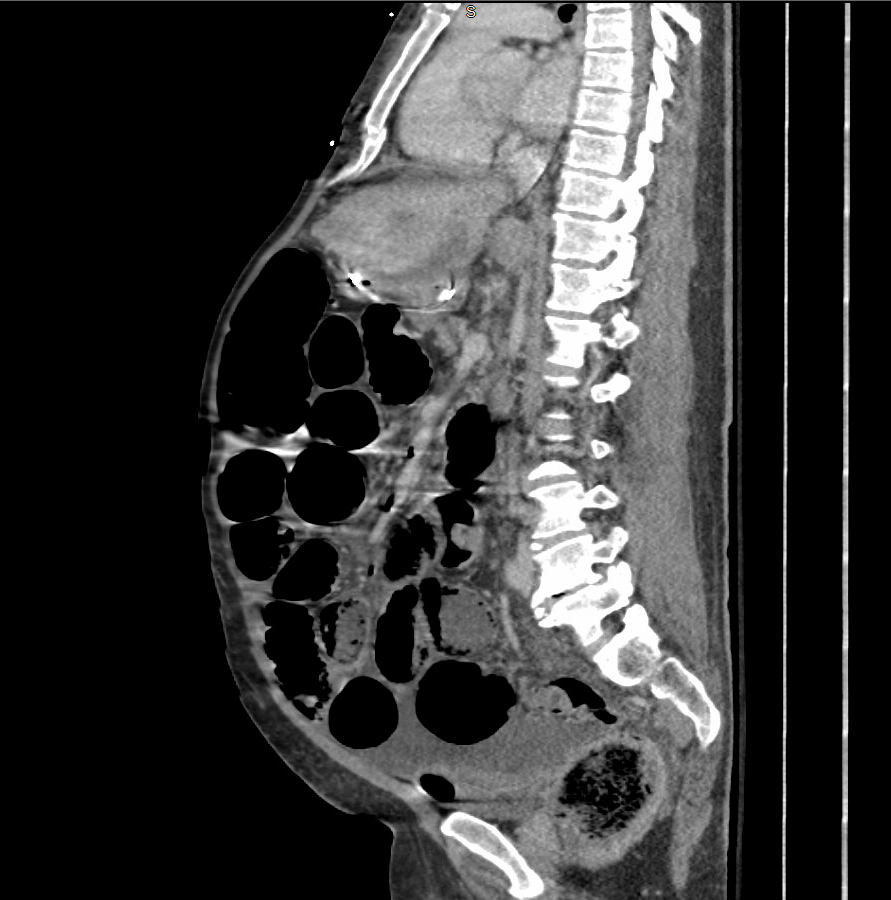
Figure: Gas in portal vein on CT scan
Disclosures:
Balkrishna Sapariya indicated no relevant financial relationships.
Nathalie Freites Gonzalez indicated no relevant financial relationships.
Nirali Sapariya indicated no relevant financial relationships.
Larry Woods indicated no relevant financial relationships.
Balkrishna R. Sapariya, MBBS1, Nathalie Freites Gonzalez, MD1, Nirali Sapariya, PA-C2, Larry Woods, DO1. P2005 - When Gas Crosses the Gut Wall: <i>Pneumatosis intestinalis</i> - Side Effect, Obstruction, or Ischemia?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
