Sunday Poster Session
Category: Small Intestine
P2003 - Anasarca in Children, Facing the Challenges of Broad Differential Diagnosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Laura Molineros, MD (she/her/hers)
Memorial Healthcare System
Pembroke Pines, FL
Presenting Author(s)
Laura Molineros, MD1, Airam Rangel, MD2, Palack Agrawal, MD2, Claudia Rojas, MD2
1Memorial Healthcare System, Pembroke Pines, FL; 2Memorial Healthcare System, Hollywood, FL
Introduction: Anasarca can be caused by increased capillary hydrostatic pressure, decreased capillary oncotic pressure or increased capillary permeability. It can be a manifestation of heart failure, primary kidney disease, protein-losing enteropathy (PLE), juvenile dermatomyositis, systemic lupus erythematosus, and congenital superior vena cava obstruction in children. A cause of PLE is celiac disease, which is triggered by the ingestion of gluten and characterized by damage to the small intestine.
Case Description/
Methods: We present a 3-year-old male with a history of stagnant weight for a year, with anasarca, decreased activity, and large, formed stools. Family history of Hashimoto's and Sjögren's disease in mom and optic neuritis in father. Initial labs show normocytic anemia (Hb 11.3 g/dL, MCV 80.5), hypoalbuminemia (3.3 g/dL), mild transaminitis (ALT 75), negative tissue transglutaminase IgA and deaminated gliadin peptide IgA. CT scan abdomen/pelvis reported nonspecific diffuse anasarca and suspected ileus versus early small bowel obstruction; nonspecific mild bilateral pleural effusions. Endoscopy showed significant villous blunting, increased intraepithelial lymphocytes, and crypt abscesses in the duodenum and ileum. Immunoglobulin levels revealed IgA < 2 mg/dL, suggesting Immunoglobulin A (IgA) deficiency, with elevated tTG IgG and DGP IgG. Other labs were normal, including NBNP, troponin I, EKG, and echocardiogram, which showed a small pericardial effusion with normal systolic function. Diagnosis of celiac disease was made and managed with a gluten-free diet and budesonide.
Discussion: Celiac disease affects about 1% of children, but diagnosis rates are much lower, with 83-91% remaining undiagnosed, one contributing factor being the variability in clinical presentation. Clinical manifestations include gastrointestinal (GI) symptoms, such as PLE, which can present as anasarca, as in this case. Other non-GI symptoms include dermatitis herpetiformis, osteopenia/osteoporosis, short stature, delayed puberty, and iron-deficiency anemia. Initial serological testing typically checks for tissue transglutaminase antibodies (TTG-IgA). IgA deficiency has a prevalence of 2-3% among patients with celiac disease. The primary treatment is strict gluten elimination from the diet. Open-capsule budesonide is effective in severe or refractory cases.
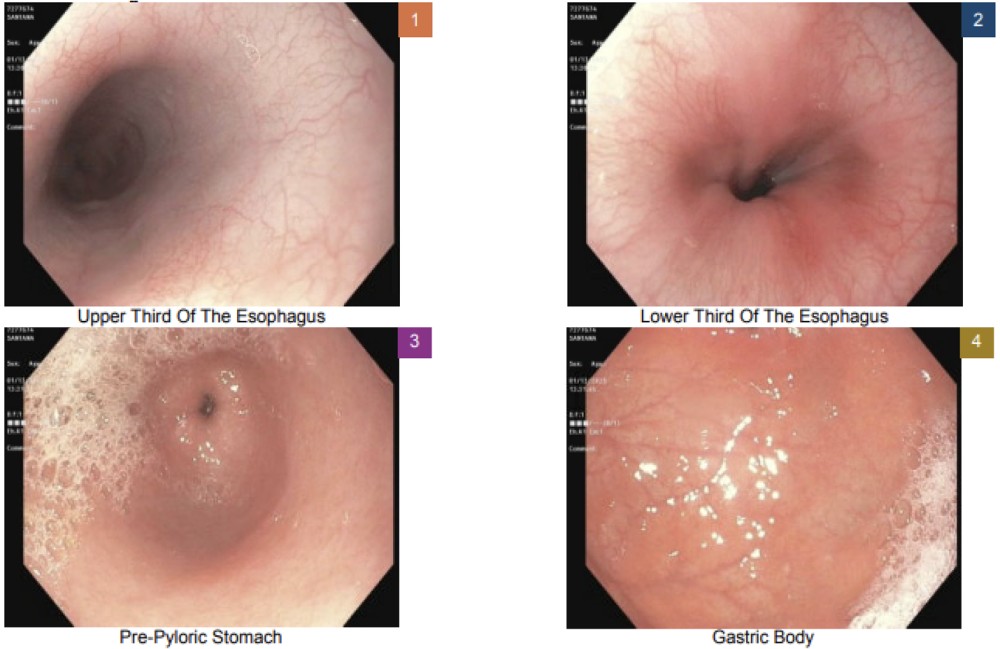
Figure: Low power. Duodenum with villous blunting
High power. Shows the numerous intraepithelial lymphocytes
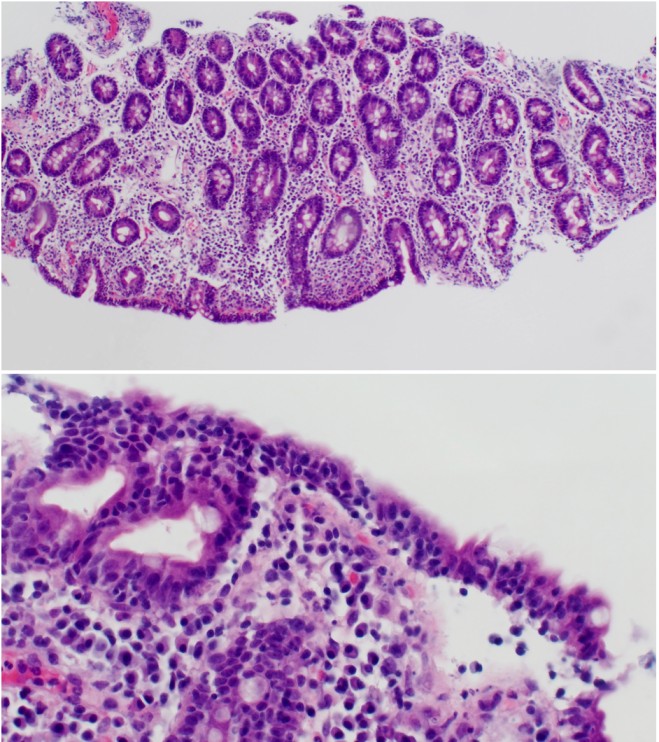
Figure: Upper endoscopy without gross evidence of inflammation, ulcerations, or any other abnormality
Disclosures:
Laura Molineros indicated no relevant financial relationships.
Airam Rangel indicated no relevant financial relationships.
Palack Agrawal indicated no relevant financial relationships.
Claudia Rojas indicated no relevant financial relationships.
Laura Molineros, MD1, Airam Rangel, MD2, Palack Agrawal, MD2, Claudia Rojas, MD2. P2003 - Anasarca in Children, Facing the Challenges of Broad Differential Diagnosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Memorial Healthcare System, Pembroke Pines, FL; 2Memorial Healthcare System, Hollywood, FL
Introduction: Anasarca can be caused by increased capillary hydrostatic pressure, decreased capillary oncotic pressure or increased capillary permeability. It can be a manifestation of heart failure, primary kidney disease, protein-losing enteropathy (PLE), juvenile dermatomyositis, systemic lupus erythematosus, and congenital superior vena cava obstruction in children. A cause of PLE is celiac disease, which is triggered by the ingestion of gluten and characterized by damage to the small intestine.
Case Description/
Methods: We present a 3-year-old male with a history of stagnant weight for a year, with anasarca, decreased activity, and large, formed stools. Family history of Hashimoto's and Sjögren's disease in mom and optic neuritis in father. Initial labs show normocytic anemia (Hb 11.3 g/dL, MCV 80.5), hypoalbuminemia (3.3 g/dL), mild transaminitis (ALT 75), negative tissue transglutaminase IgA and deaminated gliadin peptide IgA. CT scan abdomen/pelvis reported nonspecific diffuse anasarca and suspected ileus versus early small bowel obstruction; nonspecific mild bilateral pleural effusions. Endoscopy showed significant villous blunting, increased intraepithelial lymphocytes, and crypt abscesses in the duodenum and ileum. Immunoglobulin levels revealed IgA < 2 mg/dL, suggesting Immunoglobulin A (IgA) deficiency, with elevated tTG IgG and DGP IgG. Other labs were normal, including NBNP, troponin I, EKG, and echocardiogram, which showed a small pericardial effusion with normal systolic function. Diagnosis of celiac disease was made and managed with a gluten-free diet and budesonide.
Discussion: Celiac disease affects about 1% of children, but diagnosis rates are much lower, with 83-91% remaining undiagnosed, one contributing factor being the variability in clinical presentation. Clinical manifestations include gastrointestinal (GI) symptoms, such as PLE, which can present as anasarca, as in this case. Other non-GI symptoms include dermatitis herpetiformis, osteopenia/osteoporosis, short stature, delayed puberty, and iron-deficiency anemia. Initial serological testing typically checks for tissue transglutaminase antibodies (TTG-IgA). IgA deficiency has a prevalence of 2-3% among patients with celiac disease. The primary treatment is strict gluten elimination from the diet. Open-capsule budesonide is effective in severe or refractory cases.
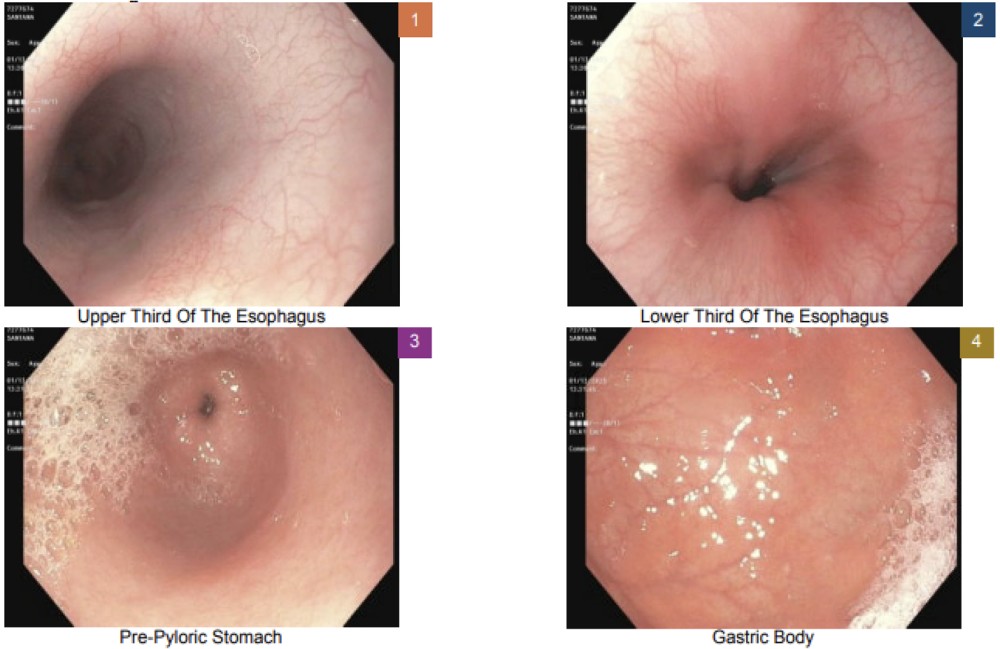
Figure: Low power. Duodenum with villous blunting
High power. Shows the numerous intraepithelial lymphocytes
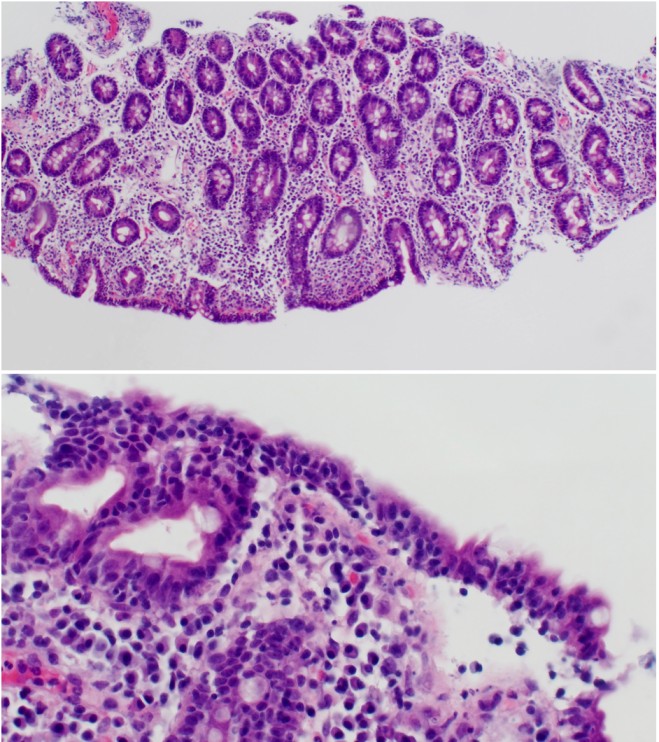
Figure: Upper endoscopy without gross evidence of inflammation, ulcerations, or any other abnormality
Disclosures:
Laura Molineros indicated no relevant financial relationships.
Airam Rangel indicated no relevant financial relationships.
Palack Agrawal indicated no relevant financial relationships.
Claudia Rojas indicated no relevant financial relationships.
Laura Molineros, MD1, Airam Rangel, MD2, Palack Agrawal, MD2, Claudia Rojas, MD2. P2003 - Anasarca in Children, Facing the Challenges of Broad Differential Diagnosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
