Monday Poster Session
Category: Biliary/Pancreas
P2167 - Addiction, Anxiety, and Access: Mental Health Comorbidities and Procedural Disparities in Acute Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmet Sakiri, MD
Mercyhealth Internal Medicine Residency
Rockford, IL
Presenting Author(s)
Ahmet Sakiri, MD1, Abu Fahad Abbasi, MD2, Fahad Sarvari, MD3, Luqman Baloch, MD3, Ammar Aqeel, MD3, Mubeen Khan Mohammed Abdul, MD3, Thayer Hamoudah, MD4, Altaf Dawood, MD4, Naser Khan, MD4
1Mercyhealth Internal Medicine Residency, Rockford, IL; 2Mercyhealth Gastroenterology Fellowship, Rockford, IL; 3Mercyhealth, Rockford, IL; 4Mercyhealth Gastroenterology, Rockford, IL
Introduction: Psychiatric illness, especially substance use disorders (SUD), is highly prevalent amongst patients hospitalized with acute pancreatitis (AP), yet its impact on procedural outcomes and delivery has not been well studied on a national scale. We aimed to assess how six psychiatric diagnostic categories influence access to guideline recommended interventions, hospital resource utilization, and timing of ERCP in AP.
Methods: We analyzed adult AP admissions (ICD-10 K85.) from the 2019-2021 NIS, grouping psychiatric comorbidities (ICD-10 F10-F69) into six categories. We excluded pregnancy, chronic pancreatitis, and pancreatic cancer. The primary outcome was receipt of any guideline directed intervention (ERCP ≤48 h, cholecystectomy ≤72 h, or drainage ≥14 d). Secondary outcomes were LOS, charges, and time to ERCP in biliary AP cohort, adjusted for covariates.
Results: Among 219,225 unweighted AP stays (weighted N ≈1,096,124), mean age was 53 years, mean LOS 5.6 days, and mean charges $72,700. Psychiatric diagnoses were present in 57% of acute pancreatitis admissions, with SUD alone in 45%. SUD was associated with 77% lower odds of receiving any guideline intervention (aOR 0.23, 95% CI 0.21–0.24, P< 0.001), while mood (aOR 0.91, P=0.024) and anxiety disorders (aOR 0.86, P=0.002) showed smaller effects. Access was independently increased at large hospitals (aOR 1.36) and urban-teaching centers (aOR 1.80). Each additional comorbidity reduced odds (aOR 0.85 per condition). SUD reduced LOS by 13% and charges by 22% (both P< 0.001); mood disorders reduced LOS by 8.5% and charges by 12.9% (P< 0.001); anxiety slightly prolonged LOS (3.4%, P=0.001). In the biliary AP subgroup (n=24,553; 481 ERCPs), psychiatric status did not affect time-to-ERCP (P >0.23), though urban-teaching hospitals nearly doubled ERCP speed (aHR 1.99, P=0.008), and each additional comorbidity delayed ERCP by 15% (aHR 0.85, P< 0.001).
Discussion: In this cohort of patients admitted with AP, SUD was linked to significant disparities procedural care, however, subgroup analyses revealed that lower ERCP rates in SUD largely reflected clinical appropriateness, rather than under-utilization of procedures. In the subgroup analysis of the biliary AP cohort, psychiatric status did not delay ERCP delivery. Instead, medical complexity and rural hospital settings were the main barriers, emphasizing the need for targeted care strategies and equitable resource distribution to ensure timely, evidence-based management for complex AP patients.
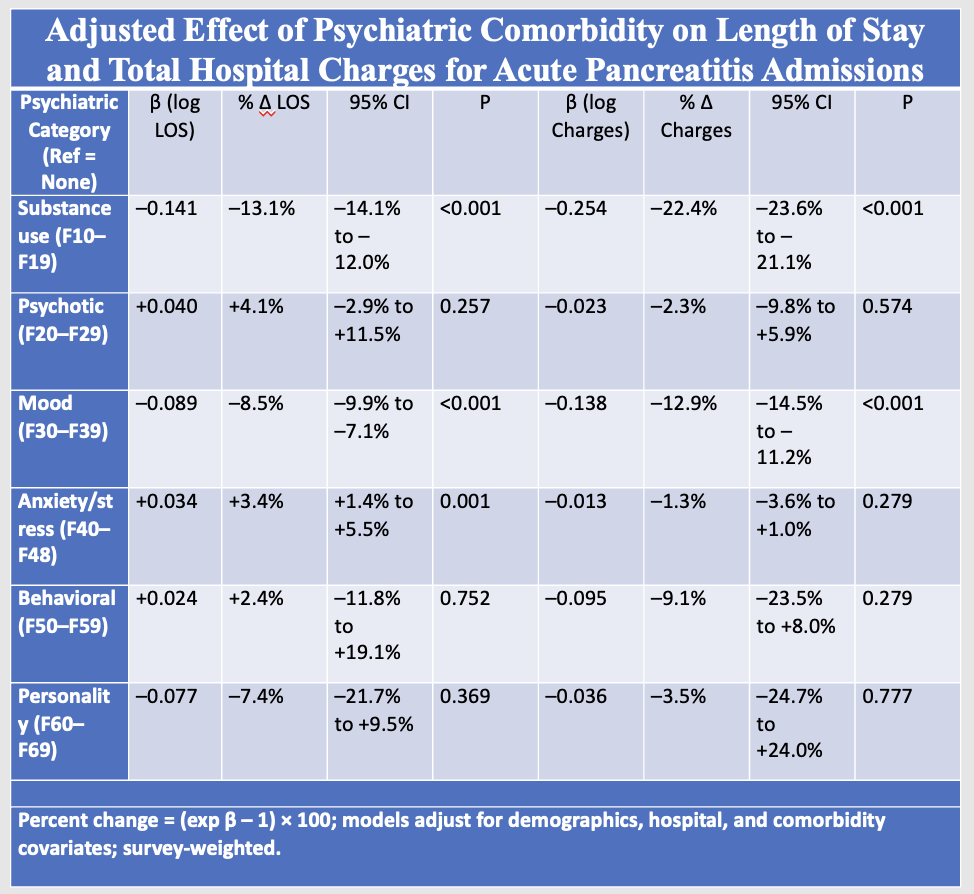
Figure: Adjusted beta coefficients (β) and percent changes in LOS and total hospital charges for acute pancreatitis admissions by psychiatric comorbidity. Models controlled for demographic, hospital, and clinical covariates with survey-weighted analysis (R² = 0.11 for LOS; adj. R² = 0.18 for charges; weighted N ≈ 630,000).
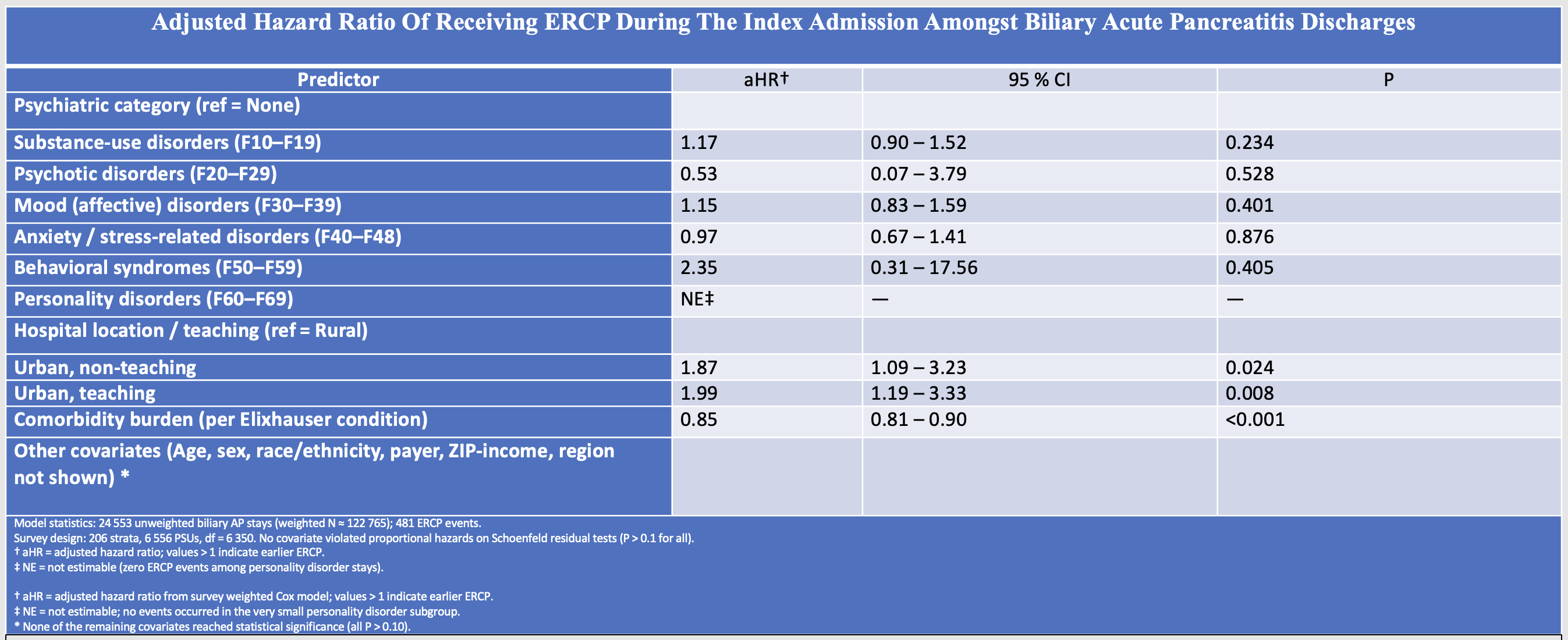
Figure: Among biliary‑acute‑pancreatitis admissions, psychiatric comorbidity was not independently associated with time‑to‑ERCP after adjustment. In contrast, treatment in urban hospitals nearly doubled the likelihood of receiving ERCP during the index stay, while higher Elixhauser burden delayed intervention by ~15 % per comorbidity.
Disclosures:
Ahmet Sakiri indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Fahad Sarvari indicated no relevant financial relationships.
Luqman Baloch indicated no relevant financial relationships.
Ammar Aqeel indicated no relevant financial relationships.
Mubeen Khan Mohammed Abdul indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Ahmet Sakiri, MD1, Abu Fahad Abbasi, MD2, Fahad Sarvari, MD3, Luqman Baloch, MD3, Ammar Aqeel, MD3, Mubeen Khan Mohammed Abdul, MD3, Thayer Hamoudah, MD4, Altaf Dawood, MD4, Naser Khan, MD4. P2167 - Addiction, Anxiety, and Access: Mental Health Comorbidities and Procedural Disparities in Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mercyhealth Internal Medicine Residency, Rockford, IL; 2Mercyhealth Gastroenterology Fellowship, Rockford, IL; 3Mercyhealth, Rockford, IL; 4Mercyhealth Gastroenterology, Rockford, IL
Introduction: Psychiatric illness, especially substance use disorders (SUD), is highly prevalent amongst patients hospitalized with acute pancreatitis (AP), yet its impact on procedural outcomes and delivery has not been well studied on a national scale. We aimed to assess how six psychiatric diagnostic categories influence access to guideline recommended interventions, hospital resource utilization, and timing of ERCP in AP.
Methods: We analyzed adult AP admissions (ICD-10 K85.) from the 2019-2021 NIS, grouping psychiatric comorbidities (ICD-10 F10-F69) into six categories. We excluded pregnancy, chronic pancreatitis, and pancreatic cancer. The primary outcome was receipt of any guideline directed intervention (ERCP ≤48 h, cholecystectomy ≤72 h, or drainage ≥14 d). Secondary outcomes were LOS, charges, and time to ERCP in biliary AP cohort, adjusted for covariates.
Results: Among 219,225 unweighted AP stays (weighted N ≈1,096,124), mean age was 53 years, mean LOS 5.6 days, and mean charges $72,700. Psychiatric diagnoses were present in 57% of acute pancreatitis admissions, with SUD alone in 45%. SUD was associated with 77% lower odds of receiving any guideline intervention (aOR 0.23, 95% CI 0.21–0.24, P< 0.001), while mood (aOR 0.91, P=0.024) and anxiety disorders (aOR 0.86, P=0.002) showed smaller effects. Access was independently increased at large hospitals (aOR 1.36) and urban-teaching centers (aOR 1.80). Each additional comorbidity reduced odds (aOR 0.85 per condition). SUD reduced LOS by 13% and charges by 22% (both P< 0.001); mood disorders reduced LOS by 8.5% and charges by 12.9% (P< 0.001); anxiety slightly prolonged LOS (3.4%, P=0.001). In the biliary AP subgroup (n=24,553; 481 ERCPs), psychiatric status did not affect time-to-ERCP (P >0.23), though urban-teaching hospitals nearly doubled ERCP speed (aHR 1.99, P=0.008), and each additional comorbidity delayed ERCP by 15% (aHR 0.85, P< 0.001).
Discussion: In this cohort of patients admitted with AP, SUD was linked to significant disparities procedural care, however, subgroup analyses revealed that lower ERCP rates in SUD largely reflected clinical appropriateness, rather than under-utilization of procedures. In the subgroup analysis of the biliary AP cohort, psychiatric status did not delay ERCP delivery. Instead, medical complexity and rural hospital settings were the main barriers, emphasizing the need for targeted care strategies and equitable resource distribution to ensure timely, evidence-based management for complex AP patients.
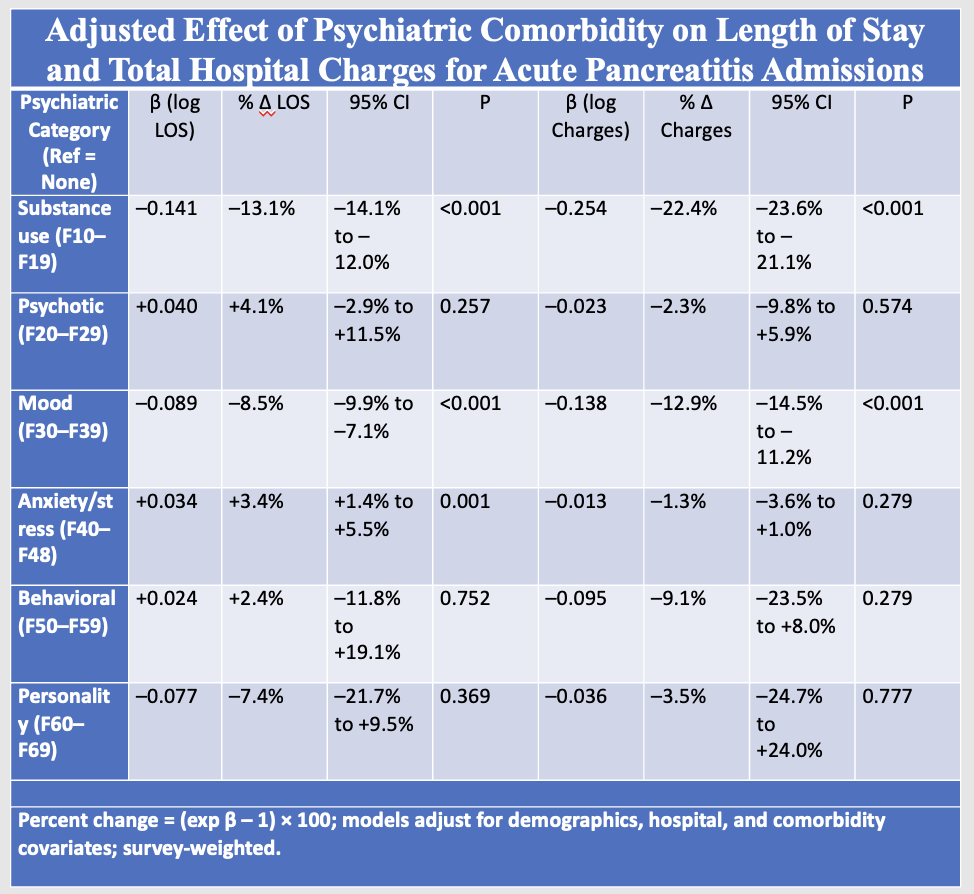
Figure: Adjusted beta coefficients (β) and percent changes in LOS and total hospital charges for acute pancreatitis admissions by psychiatric comorbidity. Models controlled for demographic, hospital, and clinical covariates with survey-weighted analysis (R² = 0.11 for LOS; adj. R² = 0.18 for charges; weighted N ≈ 630,000).
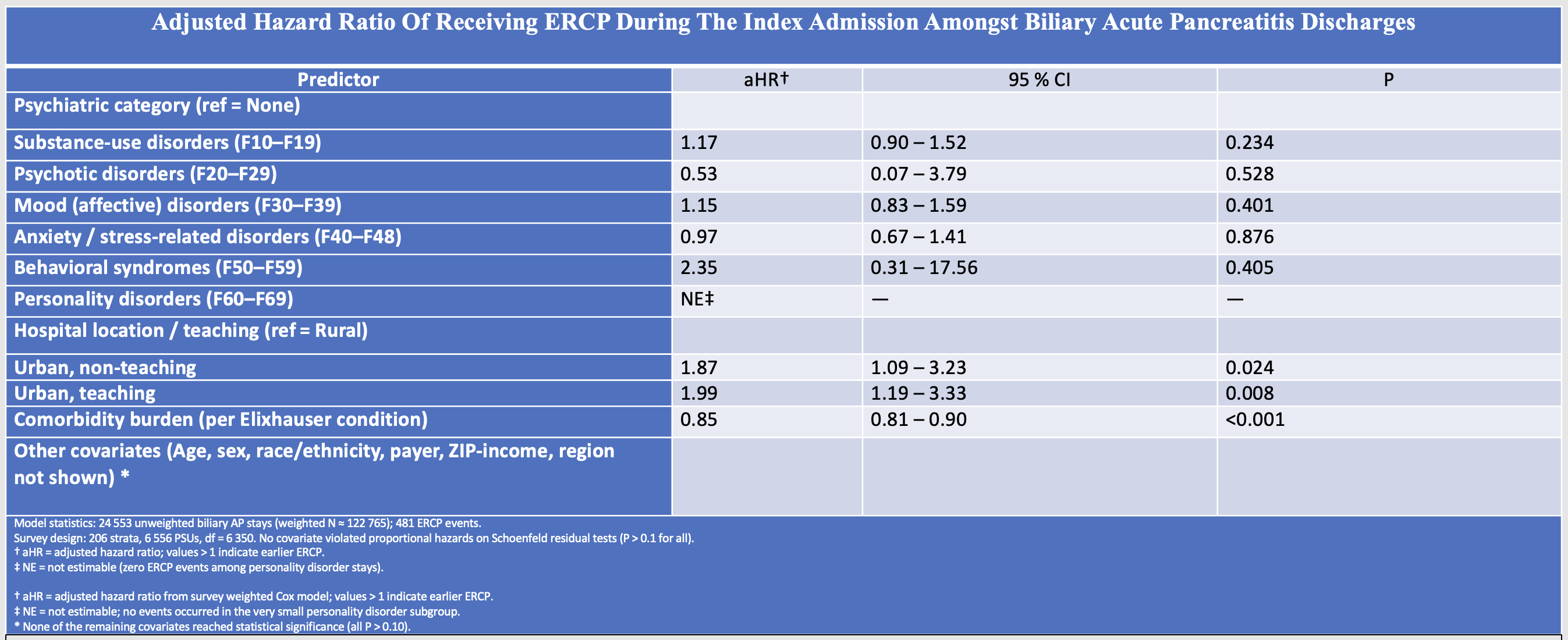
Figure: Among biliary‑acute‑pancreatitis admissions, psychiatric comorbidity was not independently associated with time‑to‑ERCP after adjustment. In contrast, treatment in urban hospitals nearly doubled the likelihood of receiving ERCP during the index stay, while higher Elixhauser burden delayed intervention by ~15 % per comorbidity.
Disclosures:
Ahmet Sakiri indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Fahad Sarvari indicated no relevant financial relationships.
Luqman Baloch indicated no relevant financial relationships.
Ammar Aqeel indicated no relevant financial relationships.
Mubeen Khan Mohammed Abdul indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Ahmet Sakiri, MD1, Abu Fahad Abbasi, MD2, Fahad Sarvari, MD3, Luqman Baloch, MD3, Ammar Aqeel, MD3, Mubeen Khan Mohammed Abdul, MD3, Thayer Hamoudah, MD4, Altaf Dawood, MD4, Naser Khan, MD4. P2167 - Addiction, Anxiety, and Access: Mental Health Comorbidities and Procedural Disparities in Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
