Monday Poster Session
Category: Biliary/Pancreas
P2165 - National Trends in ERCP Utilization and Indications: A Comparative Analysis from 2018 to 2021
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Bassel Dakkak, MD
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Bassel Dakkak, MD1, Abdelwahap Elghezewi, MD2, Yasmeen Obeidat, MD1, Tareq Alsaleh, MD3, Elizabeth Harris, MD1, Hafiz Zarsham Ali Ikram, MD1, Amro Altarawneh, MD1, Wesam Frandah, MD1, Ahmed Sherif, MD1
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Barboursville, WV; 3Department of Internal Medicine, AdventHealth Orlando, Orlando, FL
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) remains an important intervention in managing biliary and pancreatic disorders. Understanding shifts in indications, utilization patterns, and patient characteristics is essential to optimize care delivery and healthcare planning.
Methods: We used the National Inpatient Sample (NIS) 2018-2021 to identify ERCP hospitalizations using ICD-10-PCS codes, and associated common principle diagnosis using ICD-10-CM codes. Non-codable indications included cases where none of these primary diagnoses were present. Trends in patient demographics, hospital characteristics, and ERCP indications were evaluated. Survey-weighted analyses assessed changes over time, with adjusted analysis comparing outcomes such as length of stay and total hospital charges.
Results: A total of 631,245 weighted ERCP cases were analyzed (155,990 in 2018 vs. 159,465 in 2021). Patient age remained stable (mean 61 years), while the proportion of female patients declined slightly (56.4% to 54.9%, p< 0.001). Racial, insurance, and income distributions showed minimal variation. The proportion of admissions over weekends rose modestly (23.9% to 24.1%, p=0.020). Patients with Charlson Comorbidity Index ≥3 increased from 30.9% to 34.7% (p< 0.001), indicating rising complexity.
Most ERCPs occurred at urban teaching hospitals (78.9% in 2018 to 82.3% in 2021, p=0.048), with large hospitals accounting for most cases. The median length of stay remained unchanged at 6 days (p=0.27), while mean total hospital charges increased from $87,710 to $105,080—an adjusted difference of $16,087 (95% CI: $10,519–$21,654, p< 0.01).
Clinical indications shifted notably. Cases for choledocholithiasis and biliary pancreatitis declined (–1.2% and –1.3%, respectively), while ascending cholangitis saw the most pronounced drop (16.6% to 9.9%, –6.7%). Conversely, unspecified obstruction and pancreatic head mass indications rose modestly (+1.5% and +0.4%, respectively). Proportion of non-codable ERCP indications increased from 40.8% to 43.6% (+2.8%).
Discussion: ERCP utilization remained steady from 2018 to 2021, but patient complexity and hospital charges increased. The significant decline in classic indications, particularly cholangitis, alongside a rise in non-codable indications, may reflect evolving diagnostic strategies or documentation practices. These findings highlight the need for improved coding precision and targeted quality measures to ensure appropriate ERCP use. AI was used to refine language.
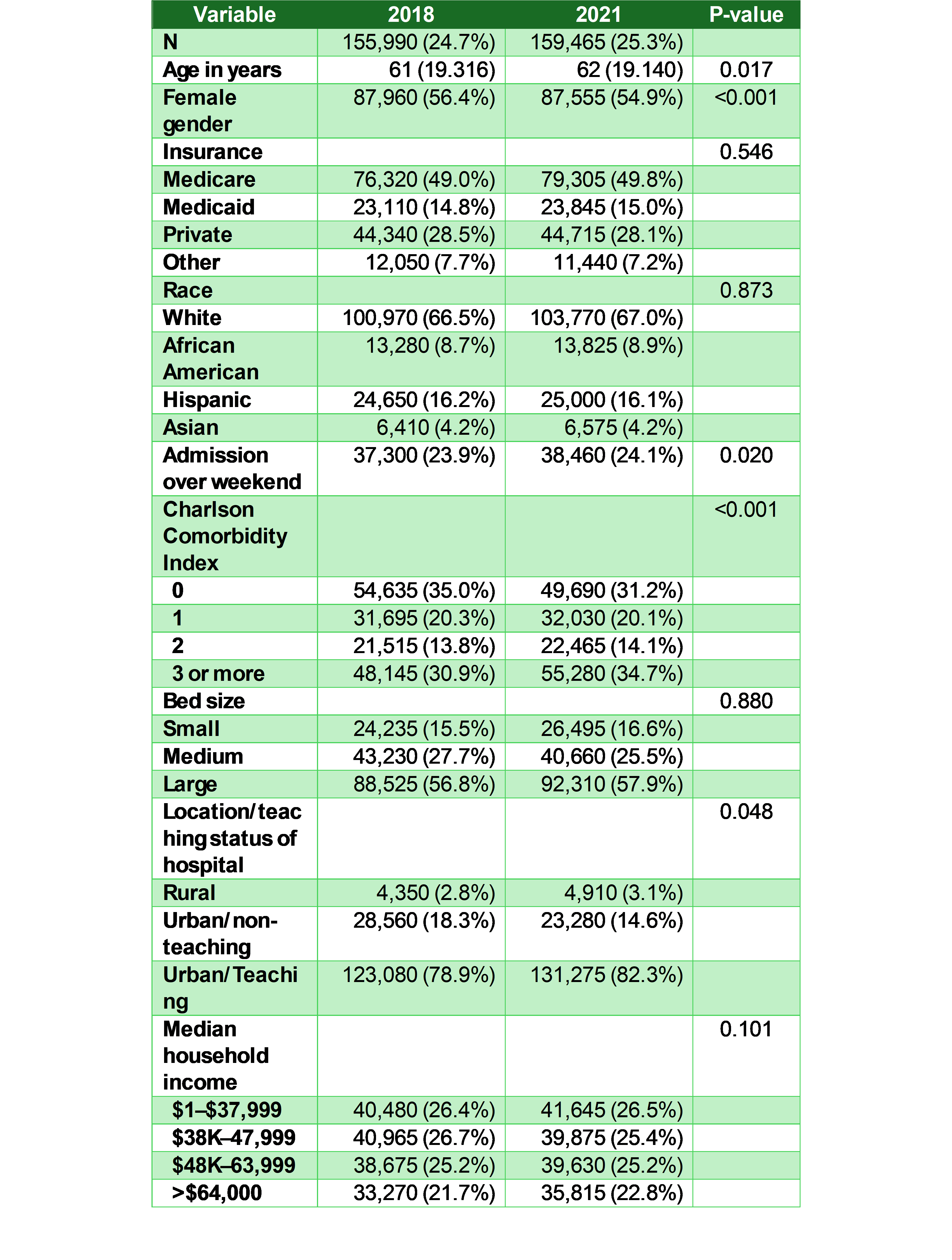
Figure: Table 1. Demographic and Hospital Characteristics of ERCP Hospitalizations in 2018 vs 2021
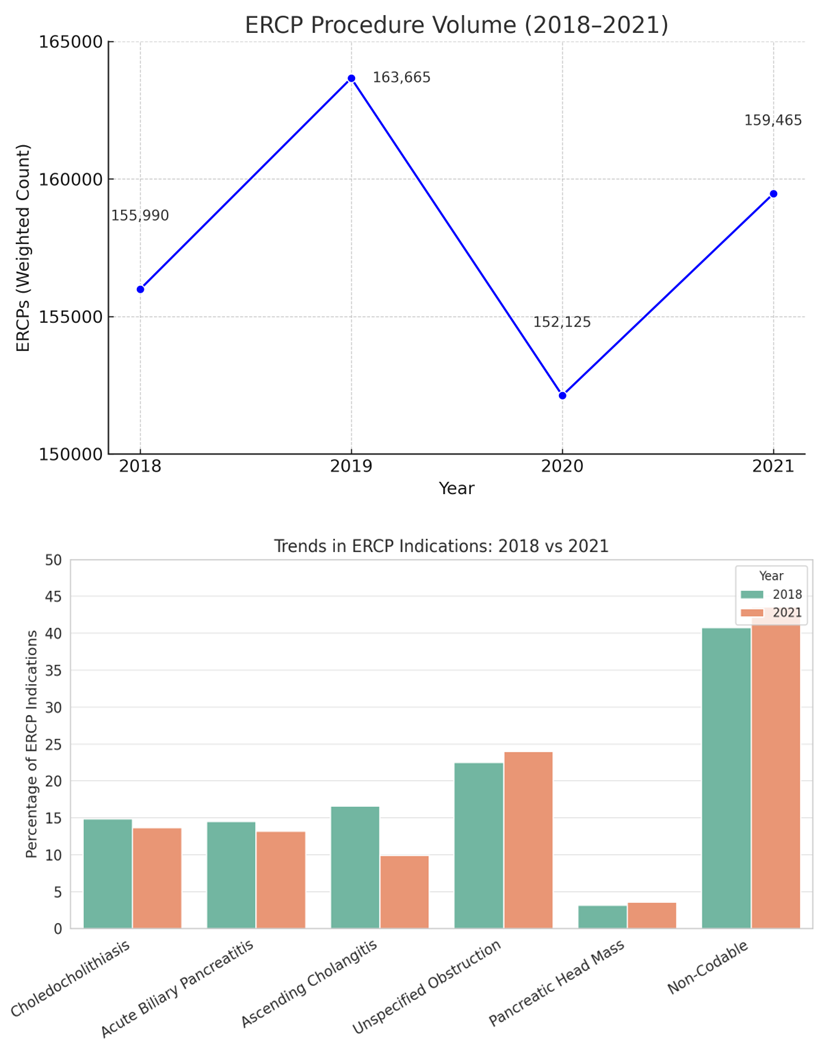
Figure: Figure 1. Trends in ERCP Utilization and Indications (2018 vs 2021)
Disclosures:
Bassel Dakkak indicated no relevant financial relationships.
Abdelwahap Elghezewi indicated no relevant financial relationships.
Yasmeen Obeidat indicated no relevant financial relationships.
Tareq Alsaleh indicated no relevant financial relationships.
Elizabeth Harris indicated no relevant financial relationships.
Hafiz Zarsham Ali Ikram indicated no relevant financial relationships.
Amro Altarawneh indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Ahmed Sherif indicated no relevant financial relationships.
Bassel Dakkak, MD1, Abdelwahap Elghezewi, MD2, Yasmeen Obeidat, MD1, Tareq Alsaleh, MD3, Elizabeth Harris, MD1, Hafiz Zarsham Ali Ikram, MD1, Amro Altarawneh, MD1, Wesam Frandah, MD1, Ahmed Sherif, MD1. P2165 - National Trends in ERCP Utilization and Indications: A Comparative Analysis from 2018 to 2021, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Barboursville, WV; 3Department of Internal Medicine, AdventHealth Orlando, Orlando, FL
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) remains an important intervention in managing biliary and pancreatic disorders. Understanding shifts in indications, utilization patterns, and patient characteristics is essential to optimize care delivery and healthcare planning.
Methods: We used the National Inpatient Sample (NIS) 2018-2021 to identify ERCP hospitalizations using ICD-10-PCS codes, and associated common principle diagnosis using ICD-10-CM codes. Non-codable indications included cases where none of these primary diagnoses were present. Trends in patient demographics, hospital characteristics, and ERCP indications were evaluated. Survey-weighted analyses assessed changes over time, with adjusted analysis comparing outcomes such as length of stay and total hospital charges.
Results: A total of 631,245 weighted ERCP cases were analyzed (155,990 in 2018 vs. 159,465 in 2021). Patient age remained stable (mean 61 years), while the proportion of female patients declined slightly (56.4% to 54.9%, p< 0.001). Racial, insurance, and income distributions showed minimal variation. The proportion of admissions over weekends rose modestly (23.9% to 24.1%, p=0.020). Patients with Charlson Comorbidity Index ≥3 increased from 30.9% to 34.7% (p< 0.001), indicating rising complexity.
Most ERCPs occurred at urban teaching hospitals (78.9% in 2018 to 82.3% in 2021, p=0.048), with large hospitals accounting for most cases. The median length of stay remained unchanged at 6 days (p=0.27), while mean total hospital charges increased from $87,710 to $105,080—an adjusted difference of $16,087 (95% CI: $10,519–$21,654, p< 0.01).
Clinical indications shifted notably. Cases for choledocholithiasis and biliary pancreatitis declined (–1.2% and –1.3%, respectively), while ascending cholangitis saw the most pronounced drop (16.6% to 9.9%, –6.7%). Conversely, unspecified obstruction and pancreatic head mass indications rose modestly (+1.5% and +0.4%, respectively). Proportion of non-codable ERCP indications increased from 40.8% to 43.6% (+2.8%).
Discussion: ERCP utilization remained steady from 2018 to 2021, but patient complexity and hospital charges increased. The significant decline in classic indications, particularly cholangitis, alongside a rise in non-codable indications, may reflect evolving diagnostic strategies or documentation practices. These findings highlight the need for improved coding precision and targeted quality measures to ensure appropriate ERCP use. AI was used to refine language.
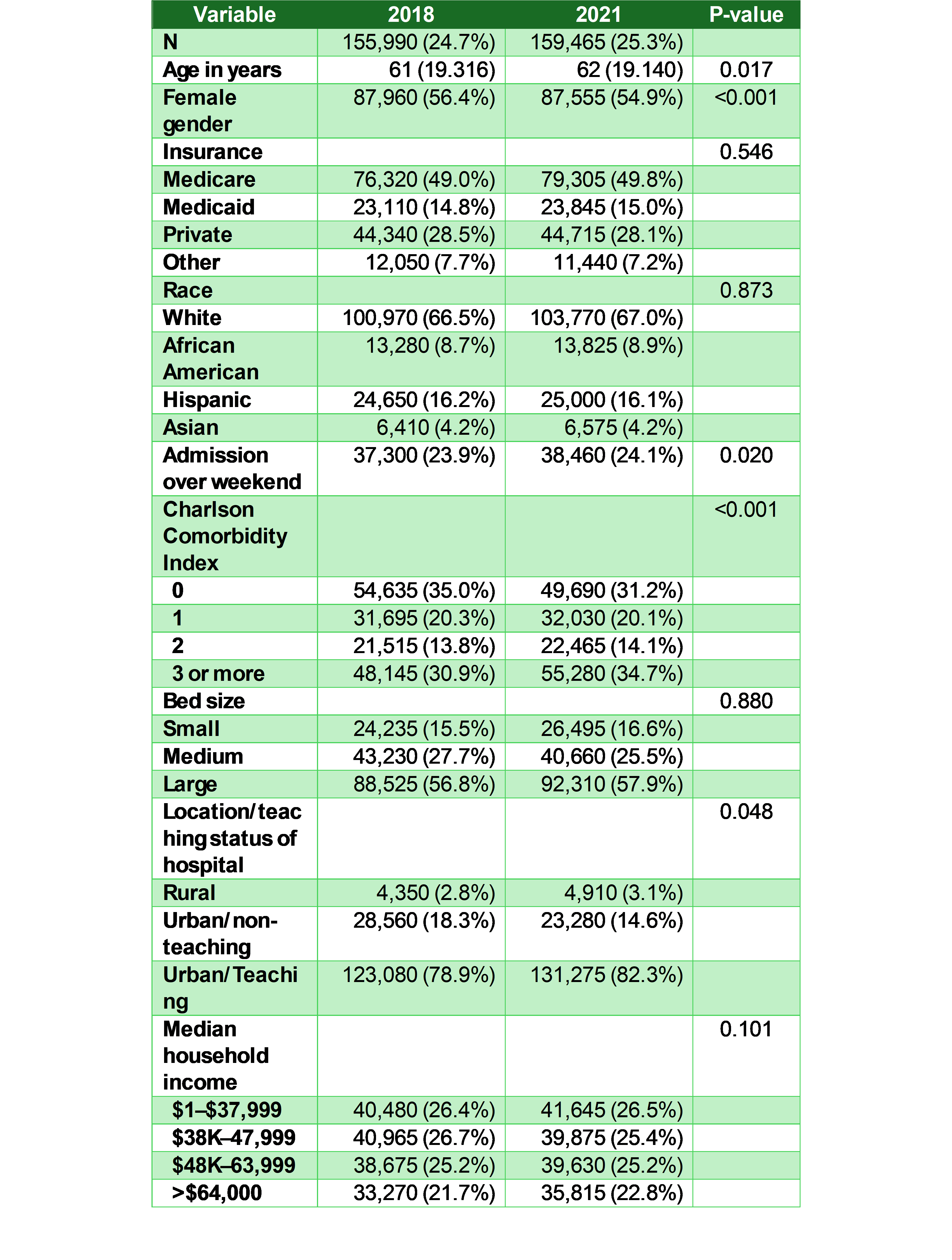
Figure: Table 1. Demographic and Hospital Characteristics of ERCP Hospitalizations in 2018 vs 2021
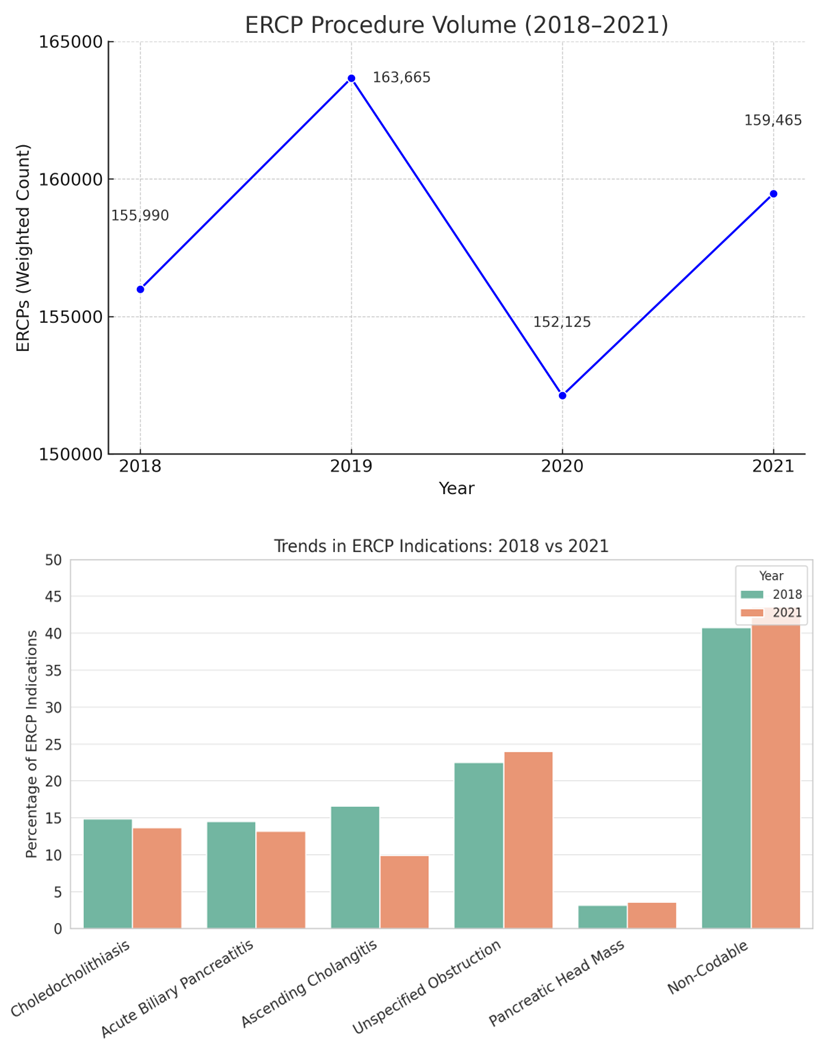
Figure: Figure 1. Trends in ERCP Utilization and Indications (2018 vs 2021)
Disclosures:
Bassel Dakkak indicated no relevant financial relationships.
Abdelwahap Elghezewi indicated no relevant financial relationships.
Yasmeen Obeidat indicated no relevant financial relationships.
Tareq Alsaleh indicated no relevant financial relationships.
Elizabeth Harris indicated no relevant financial relationships.
Hafiz Zarsham Ali Ikram indicated no relevant financial relationships.
Amro Altarawneh indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Ahmed Sherif indicated no relevant financial relationships.
Bassel Dakkak, MD1, Abdelwahap Elghezewi, MD2, Yasmeen Obeidat, MD1, Tareq Alsaleh, MD3, Elizabeth Harris, MD1, Hafiz Zarsham Ali Ikram, MD1, Amro Altarawneh, MD1, Wesam Frandah, MD1, Ahmed Sherif, MD1. P2165 - National Trends in ERCP Utilization and Indications: A Comparative Analysis from 2018 to 2021, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
