Monday Poster Session
Category: Biliary/Pancreas
P2161 - Comparison of Outcomes With Early vs Delayed Biliary Decompression After Endoscopic Ultrasound of Head of Pancreas Mass: A Population-Level Retrospective Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- VP
Vanisha Patel, MD (she/her/hers)
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Vanisha Patel, MD1, Delvise Fogwe, MD1, Melica Nikahd, MS2, Thomas McCarty, MD, MPH3, Ahmad Bazarbashi, MD4, Kelly Hathorn, MD5, Tarek Sawas, MD6, Fadi Hawa, MD1, Richard Maradiaga, MD1, Stacey Culp, PhD1, Eric Swei, MD1, Erica Park, MD1, Jordan Burlen, MD1, Hamza Shah, DO1, Mitchell L. Ramsey, MD1, Peter Lee, MBBCh1, Somashekar Krishna, MD, MPH1, Ashish Manne, MBBS1, Susan Tsai, MD, MHS1, Georgios I. Papachristou, MD, PhD1, Philip A. Hart, MD1, Raj Shah, MD1
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University, Columbus, OH; 3Houston Methodist Hospital, Houston, TX; 4Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, WA; 5University of North Carolina at Chapel Hill, Durham, NC; 6University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Malignant biliary obstruction (MBO) can occur with head of the pancreas (HOP) masses and is often managed by endoscopic retrograde cholangiopancreatography (ERCP) or interventional radiology (IR) biliary decompression. We aimed to determine the rate of ERCP or IR drainage following endoscopic ultrasound (EUS) for HOP mass, and to assess the impact of timing on need for subsequent procedures, 30-day readmission rates, and duration of chemotherapy.
Methods: This retrospective study used the Market Scan Research Database from 2016 to 2022. Inclusion criteria comprised a diagnosis of malignant HOP mass (ICD-10: C25.0), an EUS CPT code and minimum 3-month follow-up. Patients were categorized into groups as per Figure 1. Early biliary drainage was defined as patients that had a CPT code for ERCP or IR procedure within 3 days of index EUS. Delayed biliary drainage was defined by patients with a CPT code for ERCP or IR procedure >3 days after index EUS. Surgical interventions included ICD-10 codes for Whipple surgery variants. Never ERCP/IR group included patients that never had biliary intervention. Secondary outcomes included incidence of repeat ERCP, 30-day readmission rate following EUS, and duration of chemotherapy treatment. Statistical analysis included Wilcoxon rank sum test for continuous variables and chi-square tests for categorical measures.
Results: A total of 4238 patients with HOP mass were identified; 39% had early ERCP drainage and 4% had early IR drainage (Figure 1). Of the group that underwent EUS alone, 26.9% (n=649) subsequently underwent delayed biliary drainage. Baseline characteristics between delayed decompression and no ERCP/IR drainage were similar except for higher Charlson Comorbidity Index (p< 0.001) in the delayed drainage group. Within 30-days of ERCP drainage, most patients did not require re-intervention with a second ERCP (96.3% in early drainage group vs 95.9% in delayed biliary drainage group). The rate of repeat hospitalization for pancreatitis was higher in the early drainage group (4.4% vs 2.5%) while the rate of sepsis was higher in the delayed ERCP group (5.5% vs 4%). The duration of chemotherapy treatment did not vary by timing of ERCP.
Discussion: In patients with a HOP mass, malignant biliary obstruction resulted in early biliary drainage procedure in 43% of patients and delayed biliary drainage in 27% of patients. The readmission rate within 30-days of EUS were similar between the groups and there was no significant impact on chemotherapy duration.
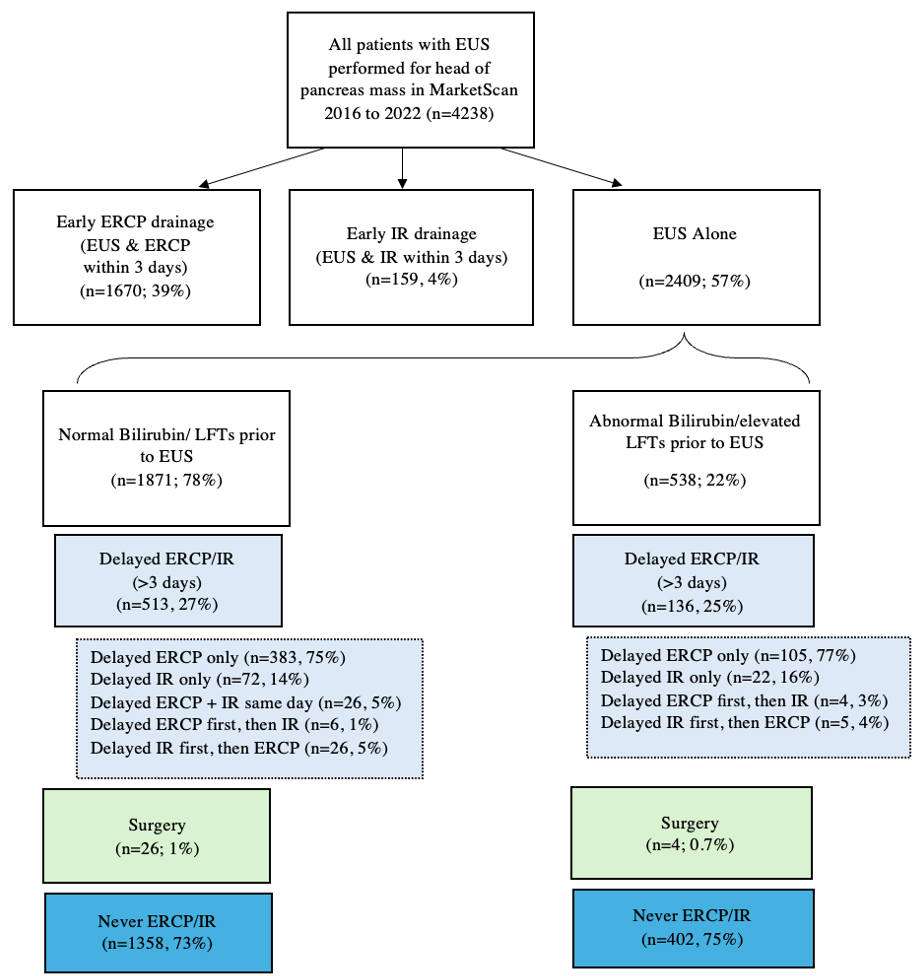
Figure: Figure 1: Flow diagram representing the timing and approach to biliary decompression for patients who underwent endoscopic ultrasound for head of pancreas mass.
Abbreviations: Endoscopic ultrasound (EUS), Endoscopic retrograde cholangiopancreatography (ERCP), Interventional radiology (IR), Interquartile range (IQR), Liver function tests (LFTs)
Disclosures:
Vanisha Patel indicated no relevant financial relationships.
Delvise Fogwe indicated no relevant financial relationships.
Melica Nikahd indicated no relevant financial relationships.
Thomas McCarty indicated no relevant financial relationships.
Ahmad Bazarbashi indicated no relevant financial relationships.
Kelly Hathorn indicated no relevant financial relationships.
Tarek Sawas indicated no relevant financial relationships.
Fadi Hawa indicated no relevant financial relationships.
Richard Maradiaga indicated no relevant financial relationships.
Stacey Culp indicated no relevant financial relationships.
Eric Swei indicated no relevant financial relationships.
Erica Park indicated no relevant financial relationships.
Jordan Burlen indicated no relevant financial relationships.
Hamza Shah indicated no relevant financial relationships.
Mitchell Ramsey indicated no relevant financial relationships.
Peter Lee indicated no relevant financial relationships.
Somashekar Krishna indicated no relevant financial relationships.
Ashish Manne indicated no relevant financial relationships.
Susan Tsai indicated no relevant financial relationships.
Georgios Papachristou: AbbVie – Grant/Research Support.
Philip Hart indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Vanisha Patel, MD1, Delvise Fogwe, MD1, Melica Nikahd, MS2, Thomas McCarty, MD, MPH3, Ahmad Bazarbashi, MD4, Kelly Hathorn, MD5, Tarek Sawas, MD6, Fadi Hawa, MD1, Richard Maradiaga, MD1, Stacey Culp, PhD1, Eric Swei, MD1, Erica Park, MD1, Jordan Burlen, MD1, Hamza Shah, DO1, Mitchell L. Ramsey, MD1, Peter Lee, MBBCh1, Somashekar Krishna, MD, MPH1, Ashish Manne, MBBS1, Susan Tsai, MD, MHS1, Georgios I. Papachristou, MD, PhD1, Philip A. Hart, MD1, Raj Shah, MD1. P2161 - Comparison of Outcomes With Early vs Delayed Biliary Decompression After Endoscopic Ultrasound of Head of Pancreas Mass: A Population-Level Retrospective Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University, Columbus, OH; 3Houston Methodist Hospital, Houston, TX; 4Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, WA; 5University of North Carolina at Chapel Hill, Durham, NC; 6University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Malignant biliary obstruction (MBO) can occur with head of the pancreas (HOP) masses and is often managed by endoscopic retrograde cholangiopancreatography (ERCP) or interventional radiology (IR) biliary decompression. We aimed to determine the rate of ERCP or IR drainage following endoscopic ultrasound (EUS) for HOP mass, and to assess the impact of timing on need for subsequent procedures, 30-day readmission rates, and duration of chemotherapy.
Methods: This retrospective study used the Market Scan Research Database from 2016 to 2022. Inclusion criteria comprised a diagnosis of malignant HOP mass (ICD-10: C25.0), an EUS CPT code and minimum 3-month follow-up. Patients were categorized into groups as per Figure 1. Early biliary drainage was defined as patients that had a CPT code for ERCP or IR procedure within 3 days of index EUS. Delayed biliary drainage was defined by patients with a CPT code for ERCP or IR procedure >3 days after index EUS. Surgical interventions included ICD-10 codes for Whipple surgery variants. Never ERCP/IR group included patients that never had biliary intervention. Secondary outcomes included incidence of repeat ERCP, 30-day readmission rate following EUS, and duration of chemotherapy treatment. Statistical analysis included Wilcoxon rank sum test for continuous variables and chi-square tests for categorical measures.
Results: A total of 4238 patients with HOP mass were identified; 39% had early ERCP drainage and 4% had early IR drainage (Figure 1). Of the group that underwent EUS alone, 26.9% (n=649) subsequently underwent delayed biliary drainage. Baseline characteristics between delayed decompression and no ERCP/IR drainage were similar except for higher Charlson Comorbidity Index (p< 0.001) in the delayed drainage group. Within 30-days of ERCP drainage, most patients did not require re-intervention with a second ERCP (96.3% in early drainage group vs 95.9% in delayed biliary drainage group). The rate of repeat hospitalization for pancreatitis was higher in the early drainage group (4.4% vs 2.5%) while the rate of sepsis was higher in the delayed ERCP group (5.5% vs 4%). The duration of chemotherapy treatment did not vary by timing of ERCP.
Discussion: In patients with a HOP mass, malignant biliary obstruction resulted in early biliary drainage procedure in 43% of patients and delayed biliary drainage in 27% of patients. The readmission rate within 30-days of EUS were similar between the groups and there was no significant impact on chemotherapy duration.
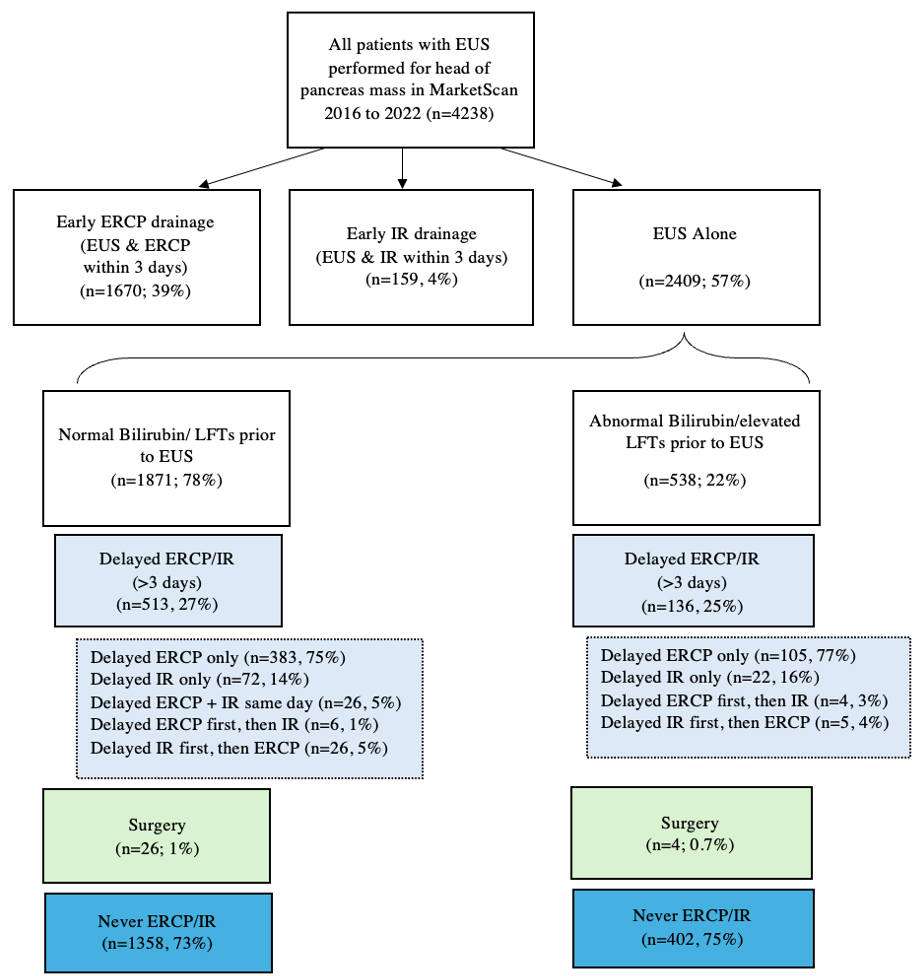
Figure: Figure 1: Flow diagram representing the timing and approach to biliary decompression for patients who underwent endoscopic ultrasound for head of pancreas mass.
Abbreviations: Endoscopic ultrasound (EUS), Endoscopic retrograde cholangiopancreatography (ERCP), Interventional radiology (IR), Interquartile range (IQR), Liver function tests (LFTs)
Disclosures:
Vanisha Patel indicated no relevant financial relationships.
Delvise Fogwe indicated no relevant financial relationships.
Melica Nikahd indicated no relevant financial relationships.
Thomas McCarty indicated no relevant financial relationships.
Ahmad Bazarbashi indicated no relevant financial relationships.
Kelly Hathorn indicated no relevant financial relationships.
Tarek Sawas indicated no relevant financial relationships.
Fadi Hawa indicated no relevant financial relationships.
Richard Maradiaga indicated no relevant financial relationships.
Stacey Culp indicated no relevant financial relationships.
Eric Swei indicated no relevant financial relationships.
Erica Park indicated no relevant financial relationships.
Jordan Burlen indicated no relevant financial relationships.
Hamza Shah indicated no relevant financial relationships.
Mitchell Ramsey indicated no relevant financial relationships.
Peter Lee indicated no relevant financial relationships.
Somashekar Krishna indicated no relevant financial relationships.
Ashish Manne indicated no relevant financial relationships.
Susan Tsai indicated no relevant financial relationships.
Georgios Papachristou: AbbVie – Grant/Research Support.
Philip Hart indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Vanisha Patel, MD1, Delvise Fogwe, MD1, Melica Nikahd, MS2, Thomas McCarty, MD, MPH3, Ahmad Bazarbashi, MD4, Kelly Hathorn, MD5, Tarek Sawas, MD6, Fadi Hawa, MD1, Richard Maradiaga, MD1, Stacey Culp, PhD1, Eric Swei, MD1, Erica Park, MD1, Jordan Burlen, MD1, Hamza Shah, DO1, Mitchell L. Ramsey, MD1, Peter Lee, MBBCh1, Somashekar Krishna, MD, MPH1, Ashish Manne, MBBS1, Susan Tsai, MD, MHS1, Georgios I. Papachristou, MD, PhD1, Philip A. Hart, MD1, Raj Shah, MD1. P2161 - Comparison of Outcomes With Early vs Delayed Biliary Decompression After Endoscopic Ultrasound of Head of Pancreas Mass: A Population-Level Retrospective Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
