Monday Poster Session
Category: Biliary/Pancreas
P2251 - A Common Finding With an Uncommon Etiology: Biliary Stricture Secondary to Metastatic Lung Cancer
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

John Thesing, DO
University of Kansas School of Medicine - Wichita
Wichita, KS
Presenting Author(s)
Award: ACG Presidential Poster Award
John Thesing, DO1, Erica Wunderlich, BS2, Nader Al Souky, MD2, William J.. Salyers, MD, MPH1
1University of Kansas School of Medicine - Wichita, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS
Introduction: Biliary strictures, with an estimated incidence of 1–2 per 100,000 annually, are often secondary to malignancy. The most common causes include pancreatic adenocarcinoma, cholangiocarcinoma, ampullary and gallbladder cancers, and metastases from distant primaries.
Case Description/
Methods: A 77-year-old male with right lung adenocarcinoma, previously treated with chemotherapy and radiation and currently on immunotherapy, presented with jaundice, right upper quadrant pain, and poor appetite. Exam revealed scleral icterus and right upper quadrant tenderness. Labs showed elevated bilirubin of 14.7 mg/dL, AST of 262 U/L, ALT of 192 U/L, alkaline phosphatase of 469 IU/L, and lipase of 303 U/L. Abdominal computed tomography (CT) demonstrated intrahepatic ductal dilation, gallbladder wall thickening, pericholecystic fluid, common bile duct dilation (1.8 cm), and small ascites. Chest X-ray showed a right lower lobe pleural effusion with thickening, concerning for empyema. Diagnoses included pancreatitis, biliary obstruction, and pleural effusion; ceftriaxone and metronidazole were initiated. Magnetic resonance cholangiopancreatography showed intra- and extrahepatic ductal dilation, a cystic mass in the pancreatic head, pancreatitis, and a large loculated pleural effusion (Figure 1). Thoracentesis cytology confirmed metastatic lung adenocarcinoma. Pancreatic CT raised concern for cholangiocarcinoma. Endoscopic retrograde cholangiopancreatography with right hepatic duct stenting led to transient improvement in jaundice and lab abnormalities (Figure 2). Biopsies from the distal bile duct stricture and hepatic duct revealed metastatic lung adenocarcinoma. Both had positive immunostaining for CK7, TTF-1, and napsin a. They were negative for CDX2. A biopsy taken from a gastric ulcer also confirmed metastatic lung adenocarcinoma with immunostaining positive for CK7 and TTF-1. Despite initial improvement and following progression of abdominal symptoms and worsening imaging findings, a biliary drainage catheter was placed. The patient was discharged to home hospice with stage IV metastatic lung adenocarcinoma.
Discussion: Biliary strictures from metastatic disease are rare, with lung adenocarcinoma being an especially uncommon source. Awareness of this etiology is essential for prognosis and management. While outcomes are poor, palliative interventions can offer meaningful symptom relief and aid in diagnostic confirmation in patients with advanced malignancy.
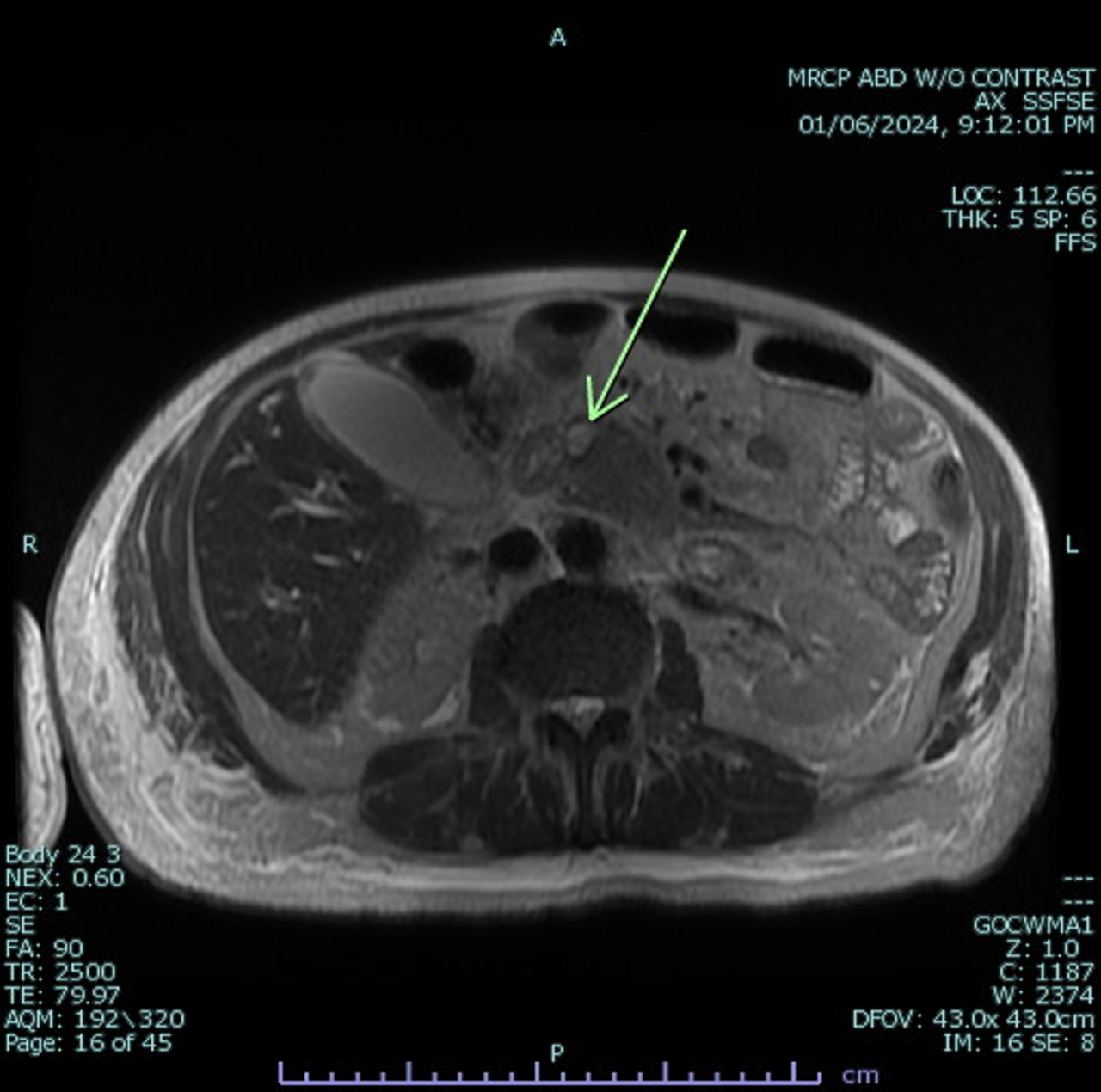
Figure: Figure 1: MRCP demonstrating a cystic mass in the pancreatic head. Intra- and extrahepatic biliary duct dilatation, common bile duct dilation, acute interstitial pancreatitis, and a moderately large loculated pleural effusion were also noted.
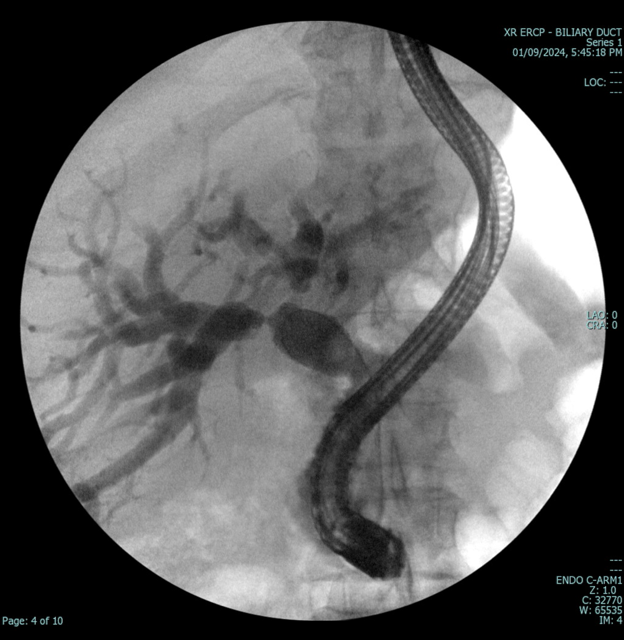
Figure: Figure 2: ERCP was done with stenting of the right hepatic duct and resulted in clinical improvement
Disclosures:
John Thesing indicated no relevant financial relationships.
Erica Wunderlich indicated no relevant financial relationships.
Nader Al Souky indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
John Thesing, DO1, Erica Wunderlich, BS2, Nader Al Souky, MD2, William J.. Salyers, MD, MPH1. P2251 - A Common Finding With an Uncommon Etiology: Biliary Stricture Secondary to Metastatic Lung Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
John Thesing, DO1, Erica Wunderlich, BS2, Nader Al Souky, MD2, William J.. Salyers, MD, MPH1
1University of Kansas School of Medicine - Wichita, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS
Introduction: Biliary strictures, with an estimated incidence of 1–2 per 100,000 annually, are often secondary to malignancy. The most common causes include pancreatic adenocarcinoma, cholangiocarcinoma, ampullary and gallbladder cancers, and metastases from distant primaries.
Case Description/
Methods: A 77-year-old male with right lung adenocarcinoma, previously treated with chemotherapy and radiation and currently on immunotherapy, presented with jaundice, right upper quadrant pain, and poor appetite. Exam revealed scleral icterus and right upper quadrant tenderness. Labs showed elevated bilirubin of 14.7 mg/dL, AST of 262 U/L, ALT of 192 U/L, alkaline phosphatase of 469 IU/L, and lipase of 303 U/L. Abdominal computed tomography (CT) demonstrated intrahepatic ductal dilation, gallbladder wall thickening, pericholecystic fluid, common bile duct dilation (1.8 cm), and small ascites. Chest X-ray showed a right lower lobe pleural effusion with thickening, concerning for empyema. Diagnoses included pancreatitis, biliary obstruction, and pleural effusion; ceftriaxone and metronidazole were initiated. Magnetic resonance cholangiopancreatography showed intra- and extrahepatic ductal dilation, a cystic mass in the pancreatic head, pancreatitis, and a large loculated pleural effusion (Figure 1). Thoracentesis cytology confirmed metastatic lung adenocarcinoma. Pancreatic CT raised concern for cholangiocarcinoma. Endoscopic retrograde cholangiopancreatography with right hepatic duct stenting led to transient improvement in jaundice and lab abnormalities (Figure 2). Biopsies from the distal bile duct stricture and hepatic duct revealed metastatic lung adenocarcinoma. Both had positive immunostaining for CK7, TTF-1, and napsin a. They were negative for CDX2. A biopsy taken from a gastric ulcer also confirmed metastatic lung adenocarcinoma with immunostaining positive for CK7 and TTF-1. Despite initial improvement and following progression of abdominal symptoms and worsening imaging findings, a biliary drainage catheter was placed. The patient was discharged to home hospice with stage IV metastatic lung adenocarcinoma.
Discussion: Biliary strictures from metastatic disease are rare, with lung adenocarcinoma being an especially uncommon source. Awareness of this etiology is essential for prognosis and management. While outcomes are poor, palliative interventions can offer meaningful symptom relief and aid in diagnostic confirmation in patients with advanced malignancy.
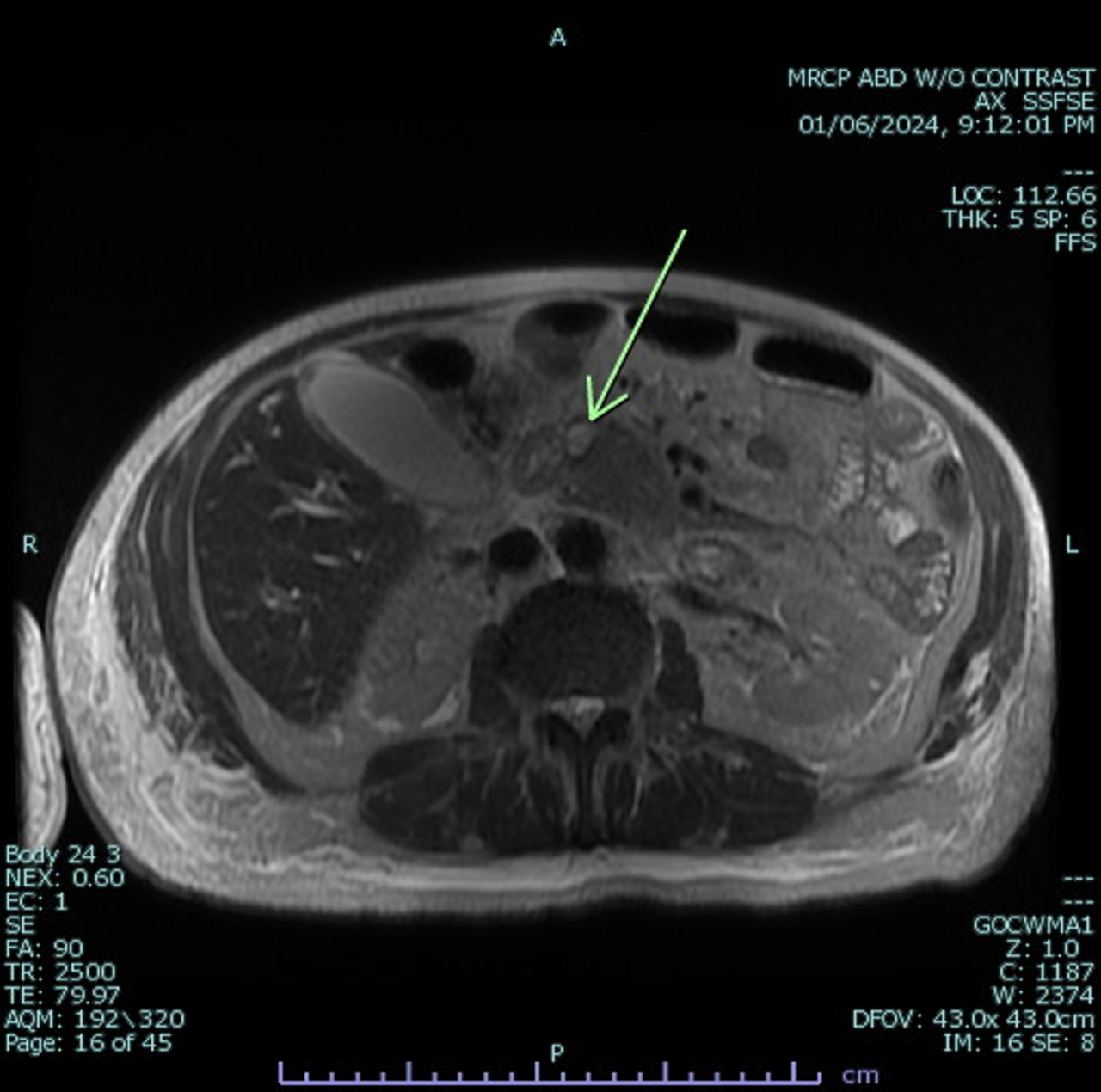
Figure: Figure 1: MRCP demonstrating a cystic mass in the pancreatic head. Intra- and extrahepatic biliary duct dilatation, common bile duct dilation, acute interstitial pancreatitis, and a moderately large loculated pleural effusion were also noted.
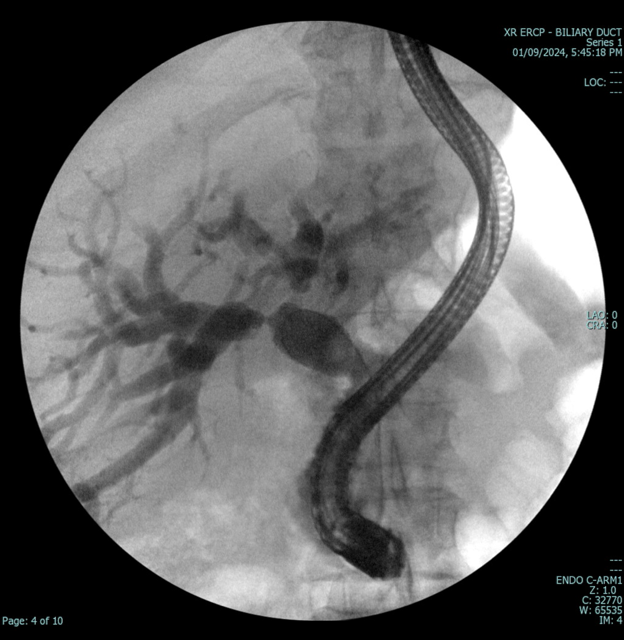
Figure: Figure 2: ERCP was done with stenting of the right hepatic duct and resulted in clinical improvement
Disclosures:
John Thesing indicated no relevant financial relationships.
Erica Wunderlich indicated no relevant financial relationships.
Nader Al Souky indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
John Thesing, DO1, Erica Wunderlich, BS2, Nader Al Souky, MD2, William J.. Salyers, MD, MPH1. P2251 - A Common Finding With an Uncommon Etiology: Biliary Stricture Secondary to Metastatic Lung Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

