Monday Poster Session
Category: Biliary/Pancreas
P2239 - Hidden in the Bile Duct: When Lymphoma Masquerades as Cholangiocarcinoma
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jalal Samhoun, MD
Florida Atlantic University Charles E. Schmidt College of Medicine
Boca Raton, FL
Presenting Author(s)
Jalal Samhoun, MD1, Allison Chin, MD2, David Forcione, MD3
1Florida Atlantic University Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Florida Atlantic University Charles E. Schmidt College of Medicine, Miami, FL; 3Baptist Health, Boca Raton, FL
Introduction: Primary biliary non-Hodgkin’s lymphoma (PBNHL) is a rare lymphoma of the biliary tree, accounting for only ~0.016% of all non-Hodgkin lymphomas. It typically presents with obstructive jaundice and often mimics cholangiocarcinoma on imaging. While most PBNHLs are of B-cell origin, primary biliary T-cell lymphoma is exceptionally uncommon, with only a few cases reported. We present a case of PB-NHTCL in a 67-year-old woman, highlighting the diagnostic challenges and need for a multidisciplinary approach.
Case Description/
Methods: A 67-year-old woman presented with jaundice. A CT abdomen and pelvis revealed a porta hepatis mass causing hilar biliary obstruction, highly suspicious for cholangiocarcinoma (Figure 1). However, initial endoscopic evaluation (endoscopic ultrasound and ERCP with sampling) was nondiagnostic, showing only benign lymphoid tissue. Given persistent concern for malignancy, repeat sampling was performed with EUS-guided fine-needle biopsy (FNB) and single-operator cholangioscopic biopsy of the bile duct stricture. The second biopsies revealed atypical lymphoid cells in the bile duct; immunohistochemistry confirmed a CD3-positive, CD30-positive T-cell lymphoma, establishing the diagnosis of PB-NHTCL. Staging PET-CT showed uptake confined to periportal lymph nodes with no distant disease, and bone marrow biopsy was negative. The patient was started on chemotherapy with brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisone (BV-CHP), per the ECHELON-2 trial.
Discussion: This case illustrates how PBNHL can masquerade as cholangiocarcinoma. It highlights the importance of repeat advanced tissue sampling when initial biopsies are inconclusive. Lymphoma is often difficult to diagnose by EUS-FNA alone, so core biopsy is frequently required for definitive diagnosis. In our patient, EUS-FNB plus cholangioscopic biopsy was pivotal for obtaining a diagnosis and obviated the need for surgical resection. This case underscores the importance of multidisciplinary teamwork in recognizing and managing such unusual presentations. Early recognition enabled appropriate therapy with BV-CHP, a regimen that improves outcomes in CD30-positive T-cell lymphomas. Clinicians should include primary biliary lymphoma in the differential diagnosis of indeterminate biliary strictures, especially when initial workup is nondiagnostic.
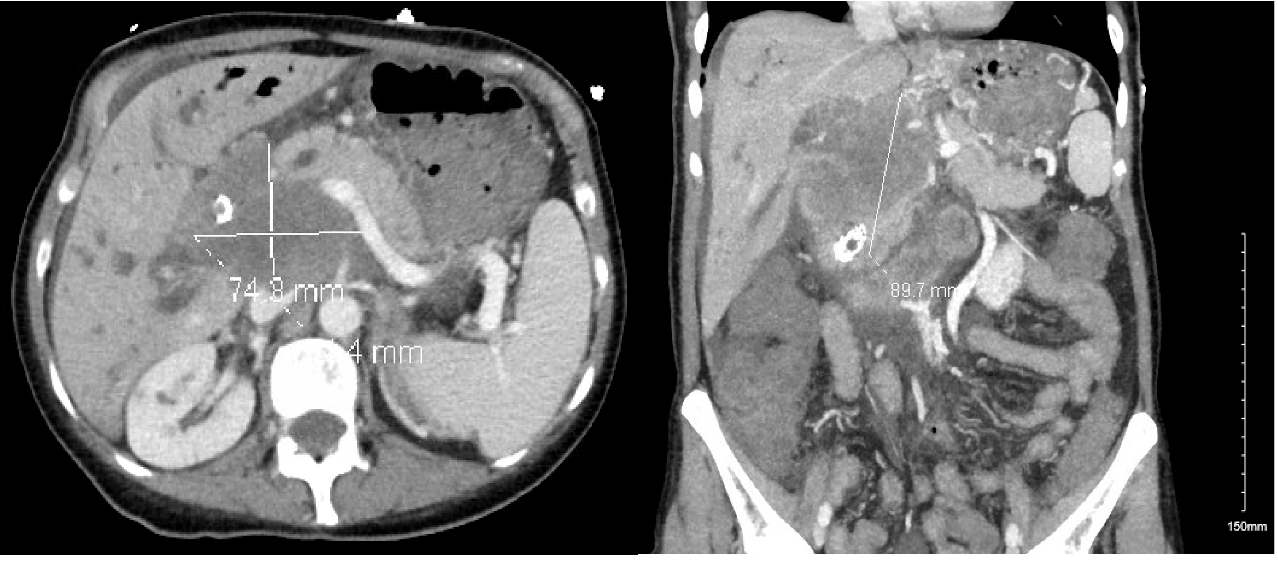
Figure: Figure 1: Axial (left) and coronal (right) CT imaging demonstrating a 74.8 mm by 91.7 mm porta hepatis mass causing significant biliary obstruction.
Disclosures:
Jalal Samhoun indicated no relevant financial relationships.
Allison Chin indicated no relevant financial relationships.
David Forcione indicated no relevant financial relationships.
Jalal Samhoun, MD1, Allison Chin, MD2, David Forcione, MD3. P2239 - Hidden in the Bile Duct: When Lymphoma Masquerades as Cholangiocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Florida Atlantic University Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Florida Atlantic University Charles E. Schmidt College of Medicine, Miami, FL; 3Baptist Health, Boca Raton, FL
Introduction: Primary biliary non-Hodgkin’s lymphoma (PBNHL) is a rare lymphoma of the biliary tree, accounting for only ~0.016% of all non-Hodgkin lymphomas. It typically presents with obstructive jaundice and often mimics cholangiocarcinoma on imaging. While most PBNHLs are of B-cell origin, primary biliary T-cell lymphoma is exceptionally uncommon, with only a few cases reported. We present a case of PB-NHTCL in a 67-year-old woman, highlighting the diagnostic challenges and need for a multidisciplinary approach.
Case Description/
Methods: A 67-year-old woman presented with jaundice. A CT abdomen and pelvis revealed a porta hepatis mass causing hilar biliary obstruction, highly suspicious for cholangiocarcinoma (Figure 1). However, initial endoscopic evaluation (endoscopic ultrasound and ERCP with sampling) was nondiagnostic, showing only benign lymphoid tissue. Given persistent concern for malignancy, repeat sampling was performed with EUS-guided fine-needle biopsy (FNB) and single-operator cholangioscopic biopsy of the bile duct stricture. The second biopsies revealed atypical lymphoid cells in the bile duct; immunohistochemistry confirmed a CD3-positive, CD30-positive T-cell lymphoma, establishing the diagnosis of PB-NHTCL. Staging PET-CT showed uptake confined to periportal lymph nodes with no distant disease, and bone marrow biopsy was negative. The patient was started on chemotherapy with brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisone (BV-CHP), per the ECHELON-2 trial.
Discussion: This case illustrates how PBNHL can masquerade as cholangiocarcinoma. It highlights the importance of repeat advanced tissue sampling when initial biopsies are inconclusive. Lymphoma is often difficult to diagnose by EUS-FNA alone, so core biopsy is frequently required for definitive diagnosis. In our patient, EUS-FNB plus cholangioscopic biopsy was pivotal for obtaining a diagnosis and obviated the need for surgical resection. This case underscores the importance of multidisciplinary teamwork in recognizing and managing such unusual presentations. Early recognition enabled appropriate therapy with BV-CHP, a regimen that improves outcomes in CD30-positive T-cell lymphomas. Clinicians should include primary biliary lymphoma in the differential diagnosis of indeterminate biliary strictures, especially when initial workup is nondiagnostic.
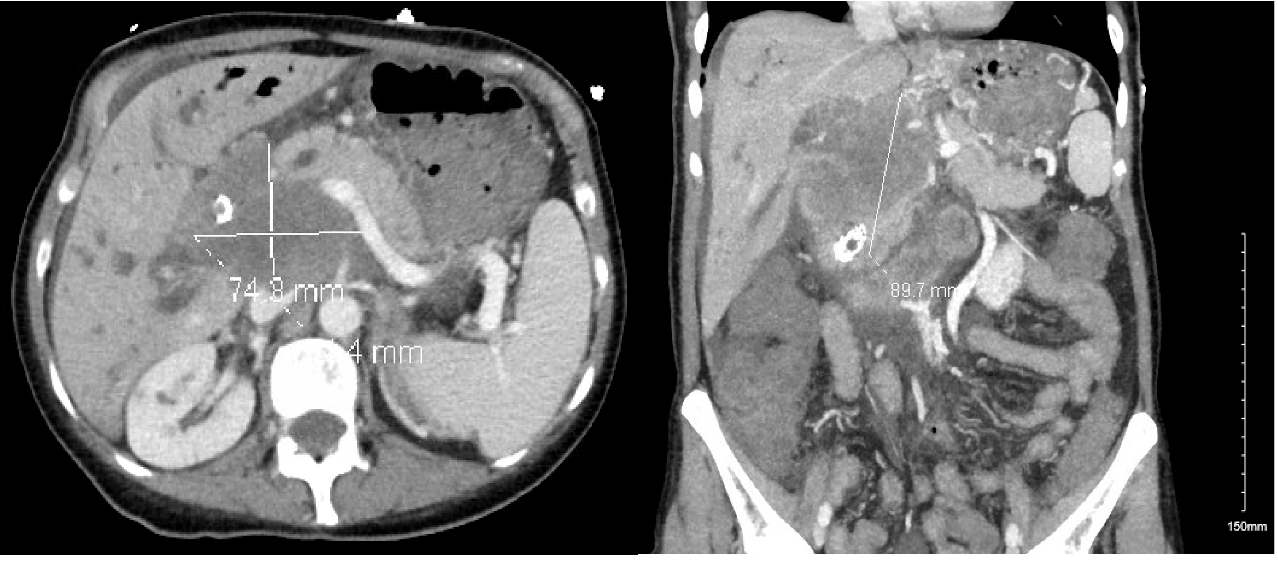
Figure: Figure 1: Axial (left) and coronal (right) CT imaging demonstrating a 74.8 mm by 91.7 mm porta hepatis mass causing significant biliary obstruction.
Disclosures:
Jalal Samhoun indicated no relevant financial relationships.
Allison Chin indicated no relevant financial relationships.
David Forcione indicated no relevant financial relationships.
Jalal Samhoun, MD1, Allison Chin, MD2, David Forcione, MD3. P2239 - Hidden in the Bile Duct: When Lymphoma Masquerades as Cholangiocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
