Monday Poster Session
Category: Biliary/Pancreas
P2233 - From Bottle to Stone: A Comparative Study of Pancreatitis Outcomes
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmed Ali Aziz, MD
INTEGRIS Health Baptist Medical Center
Edmond, OK
Presenting Author(s)
Ahmed Ali Aziz, MD1, Muhammad Ali Aziz, MD2, Rehan Shah, MD3, Ijlal Akbar. Ali, MD4
1INTEGRIS Health Baptist Medical Center, Edmond, OK; 2University of Kentucky College of Medicine, Lexington, KY; 3CarePoint Health - Bayonne Medical Center, Bayonne, NJ; 4University of Oklahoma, Oklahoma City, OK
Introduction: Alcohol induced acute pancreatitis (AIP) and gallstone pancreatitis (GP) are among the most common etiologies of acute pancreatitis (AP). Each influences the clinical course, complications, and prognosis of AP differently. Understanding the differences in outcomes between AIP and GP is crucial for informing treatment strategies and enhancing patient care. In this study, we compare the variations in hospitalization outcomes of AIP and GP.
Methods: We used the Nationwide Inpatient Sample (NIS) database from 2020 - 2022, and ICD-10 codes to identify patients with a primary discharge diagnosis of AIP and GP. We compared inpatient outcomes, including length of stay (LOS), hospitalization costs adjusted to the year 2022, in-hospital mortality, odds of sepsis, acute renal failure (ARF), shock, and need for ICU admission, between the two groups. We used multivariate regression analysis to adjust for confounders.
Results: A total of 353,960 patients were admitted with either AIP or GP from 2020 - 2022. 125,540 (35.46%) patients had GP, and 228,420 (64.53%) patients had AIP. Patients with GP had a higher mean age (50.9 years) as compared to patients with AIP (48.6 years) (Table 1). Patients with AIP had higher odds of inpatient mortality (aOR: 1.30, 95% CI: 1.01-1.69, P = 0.03), developing shock (aOR: 1.35, 95% CI: 1.13 – 1.60, P < 0.01), sepsis (aOR: 1.26, 95% CI: 1.16 – 1.36, P < 0.01), and ARF (aOR: 1.32, 95% CI: 1.25 – 1.40, P < 0.01). Patients with AIP had shorter hospital LOS (aOR: -0.18, 95% CI: -0.27 - -0.08, P < 0.01), lesser total hospitalization costs (aOR: -22,395, 95% CI: -23919 – -20,871, P < 0.01) and lower odds of requiring ICU admission (aOR: 0.82, 95% CI: 0.73 – 0.93, P < 0.01).
Discussion: Patients with AIP had higher odds of ARF, likely due to decreased appetite and malnourishment in alcoholics, leading to pre-renal AKI. AIP patients had higher odds of sepsis and shock, likely because alcohol impairs immune function, leads to systemic inflammation, infected pancreatic necrosis, and increased risk of ARDS. Overall, AIP patients had higher mortality, likely due to higher odds of ARF, cirrhosis, sepsis, and shock.
Patients with GP had longer LOS and hospitalization charges, likely due to the need for procedures such as ERCP and cholecystectomy. Patients had higher odds of needing ICU admission, likely due to post-procedure intubation or shock. GP were also older and required a prolonged time and had a higher comorbidity burden, including CHF, CKD, DM1, and took longer to recover.
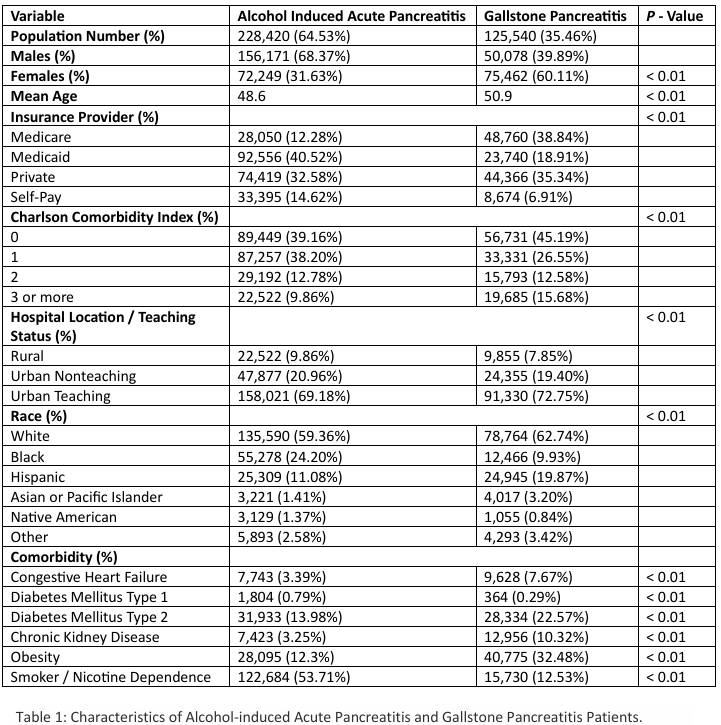
Figure: Table 1: Characteristics of Alcohol-induced Acute Pancreatitis and Gallstone Pancreatitis Patients.
Disclosures:
Ahmed Ali Aziz indicated no relevant financial relationships.
Muhammad Ali Aziz indicated no relevant financial relationships.
Rehan Shah indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Ahmed Ali Aziz, MD1, Muhammad Ali Aziz, MD2, Rehan Shah, MD3, Ijlal Akbar. Ali, MD4. P2233 - From Bottle to Stone: A Comparative Study of Pancreatitis Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1INTEGRIS Health Baptist Medical Center, Edmond, OK; 2University of Kentucky College of Medicine, Lexington, KY; 3CarePoint Health - Bayonne Medical Center, Bayonne, NJ; 4University of Oklahoma, Oklahoma City, OK
Introduction: Alcohol induced acute pancreatitis (AIP) and gallstone pancreatitis (GP) are among the most common etiologies of acute pancreatitis (AP). Each influences the clinical course, complications, and prognosis of AP differently. Understanding the differences in outcomes between AIP and GP is crucial for informing treatment strategies and enhancing patient care. In this study, we compare the variations in hospitalization outcomes of AIP and GP.
Methods: We used the Nationwide Inpatient Sample (NIS) database from 2020 - 2022, and ICD-10 codes to identify patients with a primary discharge diagnosis of AIP and GP. We compared inpatient outcomes, including length of stay (LOS), hospitalization costs adjusted to the year 2022, in-hospital mortality, odds of sepsis, acute renal failure (ARF), shock, and need for ICU admission, between the two groups. We used multivariate regression analysis to adjust for confounders.
Results: A total of 353,960 patients were admitted with either AIP or GP from 2020 - 2022. 125,540 (35.46%) patients had GP, and 228,420 (64.53%) patients had AIP. Patients with GP had a higher mean age (50.9 years) as compared to patients with AIP (48.6 years) (Table 1). Patients with AIP had higher odds of inpatient mortality (aOR: 1.30, 95% CI: 1.01-1.69, P = 0.03), developing shock (aOR: 1.35, 95% CI: 1.13 – 1.60, P < 0.01), sepsis (aOR: 1.26, 95% CI: 1.16 – 1.36, P < 0.01), and ARF (aOR: 1.32, 95% CI: 1.25 – 1.40, P < 0.01). Patients with AIP had shorter hospital LOS (aOR: -0.18, 95% CI: -0.27 - -0.08, P < 0.01), lesser total hospitalization costs (aOR: -22,395, 95% CI: -23919 – -20,871, P < 0.01) and lower odds of requiring ICU admission (aOR: 0.82, 95% CI: 0.73 – 0.93, P < 0.01).
Discussion: Patients with AIP had higher odds of ARF, likely due to decreased appetite and malnourishment in alcoholics, leading to pre-renal AKI. AIP patients had higher odds of sepsis and shock, likely because alcohol impairs immune function, leads to systemic inflammation, infected pancreatic necrosis, and increased risk of ARDS. Overall, AIP patients had higher mortality, likely due to higher odds of ARF, cirrhosis, sepsis, and shock.
Patients with GP had longer LOS and hospitalization charges, likely due to the need for procedures such as ERCP and cholecystectomy. Patients had higher odds of needing ICU admission, likely due to post-procedure intubation or shock. GP were also older and required a prolonged time and had a higher comorbidity burden, including CHF, CKD, DM1, and took longer to recover.
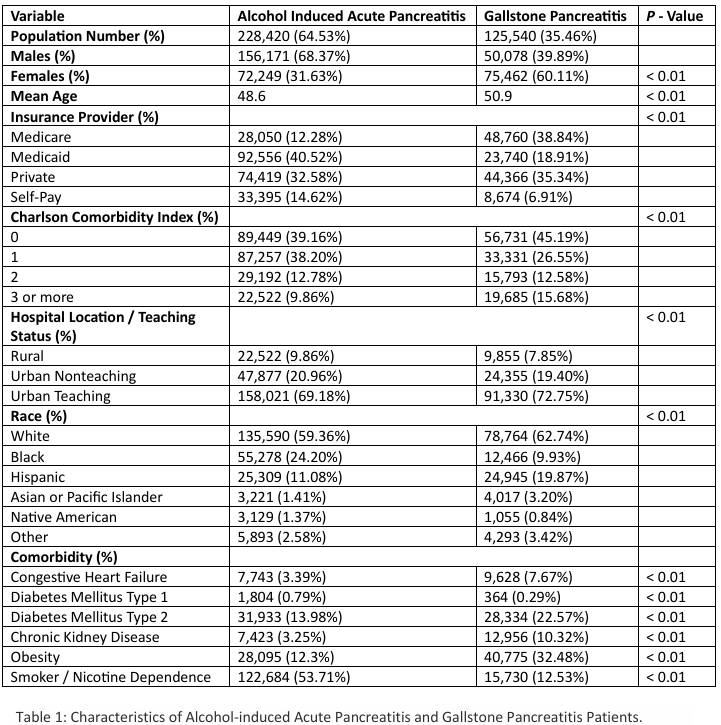
Figure: Table 1: Characteristics of Alcohol-induced Acute Pancreatitis and Gallstone Pancreatitis Patients.
Disclosures:
Ahmed Ali Aziz indicated no relevant financial relationships.
Muhammad Ali Aziz indicated no relevant financial relationships.
Rehan Shah indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Ahmed Ali Aziz, MD1, Muhammad Ali Aziz, MD2, Rehan Shah, MD3, Ijlal Akbar. Ali, MD4. P2233 - From Bottle to Stone: A Comparative Study of Pancreatitis Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
