Monday Poster Session
Category: Biliary/Pancreas
P2230 - Predictors of Survival Outcomes After Pre-Operative Biliary Drainage for Patients With Malignant Obstructive Jaundice and Pancreatic Carcinoma; A Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hasan Al-Obaidi, MD
University of Toledo College of Medicine and Life Sciences
Toledo, OH
Presenting Author(s)
Hasan Al-Obaidi, MD1, Nooraldin Merza, MD1, Osamah Muslim, MD2, Omar Saab, MD3, Mushfiqur Siddique, MD4, Mohannad Bitar, MD4, Sana Rabeeah, MD5, Bisher Sawaf, MD6, Hayder Alamily, MD7, Mustafa Al-Obaidi, MD8, Amy Mackenzie, MD9, Eunice Kwak, MD10, Fatima A. Merza, BS11, Yusuf Nawras, BSc1, Patel Manthanbhai, MD1, Hussein Harb, MD12, Abdallah Kobeissy, MD, MPH5
1University of Toledo College of Medicine and Life Sciences, Toledo, OH; 2Al-Qadisiyah University College of medicine, Diwaniyah, Al Qadisiyah, Iraq; 3University of Texas Health Science Center, Houston, TX; 4Jamaica Hospital Medical Center, Jamaica, NY; 5The University of Toledo, Toledo, OH; 6University of Toledo Medical Center, Toledo, OH; 7University of Colorado Anschutz Medical Campus, Denver, CO; 8Hassleholm hospital, Malmo, Skane Lan, Sweden; 9HCA Florida Orange Park Hospital, Orange Park, FL; 10University of Toledo Health Sciences Campus, Toledo, OH; 11University of Michigan-Dearborn, Canton, MI; 12Jamaica Hospital Medical Center, New York, NY
Introduction: Pancreatic cancer is the fourth leading cause of cancer-related deaths in the United States. Pre-operative biliary drainage (PBD) is often palliative, and its contribution to survival outcomes in patients with malignant biliary obstruction (MBO) is debatable. The present meta-analysis was performed to evaluate factors associated with survival outcomes among patients with pancreatic cancer and MBO.
Methods: All clinical studies included patients with pancreatic cancer and developed MBO, and evaluated factors associated with survival outcomes were included. These studies have to implement the Cox regression model to calculate the hazard ratio (HR) for the time to relevant outcomes. The literature review was performed through twelve databases on 15th June 2024.
Results: This study included nine articles of retrospective design, including 2461 patients. There was a statistically significant association between PBD (P< 0.001) and overall survival with an HR of 1.22. There was a statistically significant association between percutaneous biliary drainage (HR; 1.32; 95%CI; 1.08,1.62; P=0.007) and overall survival. Patients with positive surgical margin (HR; 1.34 ,95%CI;1.16, 1.55, P< 0.001) and patients with venous invasion (HR; 1.21, 95%CI; 1.05, 1.41, P=0.01) were associated with overall survival. There was a statistically significant association between lymphatic invasion (HR; 2.13,95%CI;1.30,3.49,P=0.003), perineural invasion (HR;1.88, 95%CI;1.31,2.69,P=0.006) and overall survival.
Discussion: This meta-analysis highlights that pre-operative biliary drainage (PBD) is associated with poorer overall survival in patients with malignant biliary obstruction due to pancreatic cancer. In particular, percutaneous drainage appears to carry a higher risk. Additionally, pathological features such as positive surgical margins, venous invasion, lymphatic invasion, and perineural invasion were strong predictors of worse outcomes. These findings suggest the need for careful patient selection and individualized treatment planning. Further prospective studies are warranted to confirm these associations.
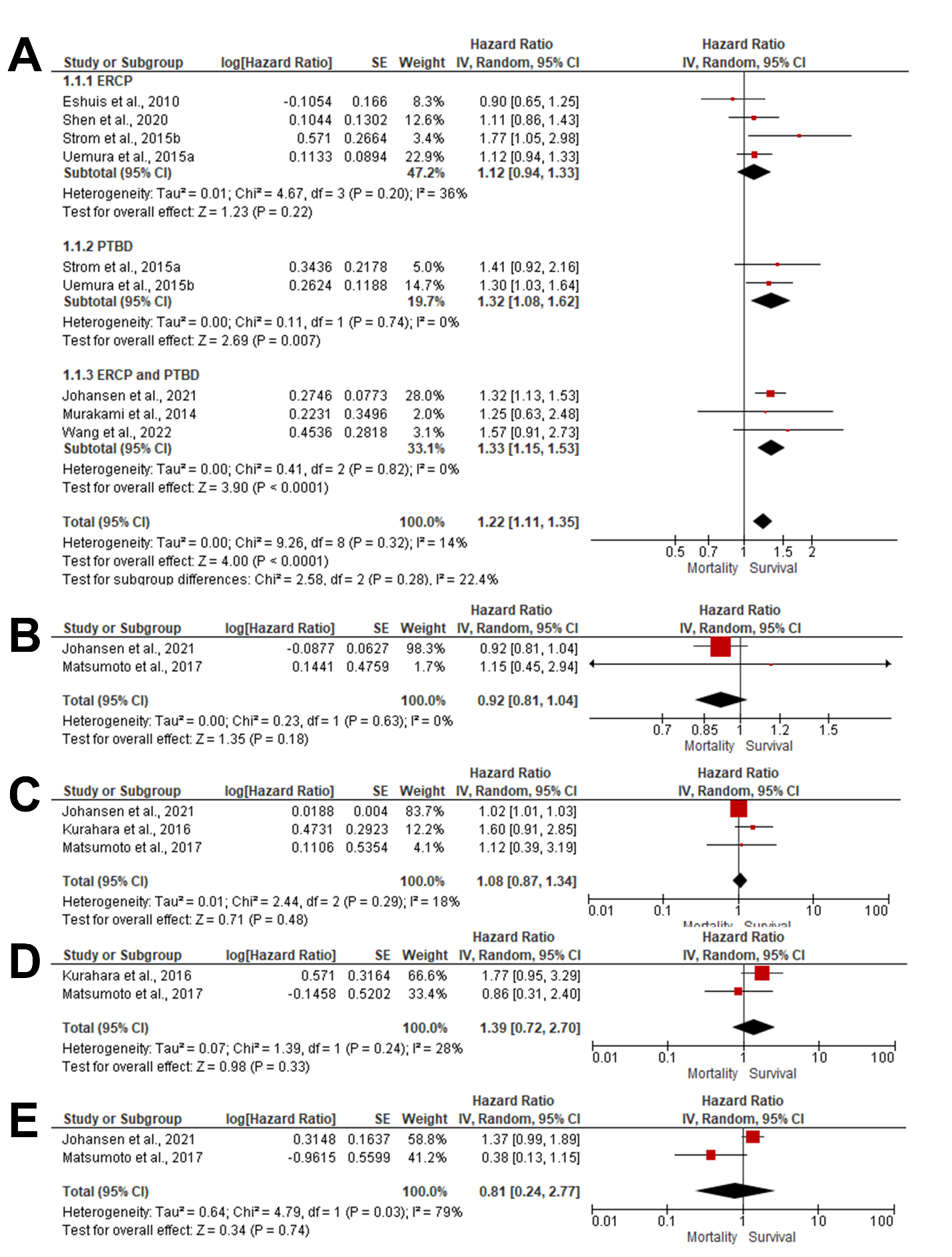
Figure: Figure1:Forest plot of summary analysis of the (A) Hazard ratio (HR) and 95% CI of the association between preoperative biliary drainage and overall survival (B) Hazard ratio (HR) and 95% CI of the association between female gender and overall survival (C) Hazard ratio (HR) and 95% CI of the association between age (years) and overall survival (D) Hazard ratio (HR) and 95% CI of the association between Serum Cancer antigen 19-9 and overall survival (E) Hazard ratio (HR) and 95% CI of the association between neoadjuvant therapy and overall survival. The size of red squares is proportional to the statistical weight of each trial. The Black diamond represents the pooled point estimate. The positioning of both diamonds and squares (along with 95% CIs) beyond the vertical line (unit value) suggests a significant outcome.
Disclosures:
Hasan Al-Obaidi indicated no relevant financial relationships.
Nooraldin Merza indicated no relevant financial relationships.
Osamah Muslim indicated no relevant financial relationships.
Omar Saab indicated no relevant financial relationships.
Mushfiqur Siddique indicated no relevant financial relationships.
Mohannad Bitar indicated no relevant financial relationships.
Sana Rabeeah indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Hayder Alamily indicated no relevant financial relationships.
Mustafa Al-Obaidi indicated no relevant financial relationships.
Amy Mackenzie indicated no relevant financial relationships.
Eunice Kwak indicated no relevant financial relationships.
Fatima Merza indicated no relevant financial relationships.
Yusuf Nawras indicated no relevant financial relationships.
Patel Manthanbhai indicated no relevant financial relationships.
Hussein Harb indicated no relevant financial relationships.
Abdallah Kobeissy indicated no relevant financial relationships.
Hasan Al-Obaidi, MD1, Nooraldin Merza, MD1, Osamah Muslim, MD2, Omar Saab, MD3, Mushfiqur Siddique, MD4, Mohannad Bitar, MD4, Sana Rabeeah, MD5, Bisher Sawaf, MD6, Hayder Alamily, MD7, Mustafa Al-Obaidi, MD8, Amy Mackenzie, MD9, Eunice Kwak, MD10, Fatima A. Merza, BS11, Yusuf Nawras, BSc1, Patel Manthanbhai, MD1, Hussein Harb, MD12, Abdallah Kobeissy, MD, MPH5. P2230 - Predictors of Survival Outcomes After Pre-Operative Biliary Drainage for Patients With Malignant Obstructive Jaundice and Pancreatic Carcinoma; A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Toledo College of Medicine and Life Sciences, Toledo, OH; 2Al-Qadisiyah University College of medicine, Diwaniyah, Al Qadisiyah, Iraq; 3University of Texas Health Science Center, Houston, TX; 4Jamaica Hospital Medical Center, Jamaica, NY; 5The University of Toledo, Toledo, OH; 6University of Toledo Medical Center, Toledo, OH; 7University of Colorado Anschutz Medical Campus, Denver, CO; 8Hassleholm hospital, Malmo, Skane Lan, Sweden; 9HCA Florida Orange Park Hospital, Orange Park, FL; 10University of Toledo Health Sciences Campus, Toledo, OH; 11University of Michigan-Dearborn, Canton, MI; 12Jamaica Hospital Medical Center, New York, NY
Introduction: Pancreatic cancer is the fourth leading cause of cancer-related deaths in the United States. Pre-operative biliary drainage (PBD) is often palliative, and its contribution to survival outcomes in patients with malignant biliary obstruction (MBO) is debatable. The present meta-analysis was performed to evaluate factors associated with survival outcomes among patients with pancreatic cancer and MBO.
Methods: All clinical studies included patients with pancreatic cancer and developed MBO, and evaluated factors associated with survival outcomes were included. These studies have to implement the Cox regression model to calculate the hazard ratio (HR) for the time to relevant outcomes. The literature review was performed through twelve databases on 15th June 2024.
Results: This study included nine articles of retrospective design, including 2461 patients. There was a statistically significant association between PBD (P< 0.001) and overall survival with an HR of 1.22. There was a statistically significant association between percutaneous biliary drainage (HR; 1.32; 95%CI; 1.08,1.62; P=0.007) and overall survival. Patients with positive surgical margin (HR; 1.34 ,95%CI;1.16, 1.55, P< 0.001) and patients with venous invasion (HR; 1.21, 95%CI; 1.05, 1.41, P=0.01) were associated with overall survival. There was a statistically significant association between lymphatic invasion (HR; 2.13,95%CI;1.30,3.49,P=0.003), perineural invasion (HR;1.88, 95%CI;1.31,2.69,P=0.006) and overall survival.
Discussion: This meta-analysis highlights that pre-operative biliary drainage (PBD) is associated with poorer overall survival in patients with malignant biliary obstruction due to pancreatic cancer. In particular, percutaneous drainage appears to carry a higher risk. Additionally, pathological features such as positive surgical margins, venous invasion, lymphatic invasion, and perineural invasion were strong predictors of worse outcomes. These findings suggest the need for careful patient selection and individualized treatment planning. Further prospective studies are warranted to confirm these associations.
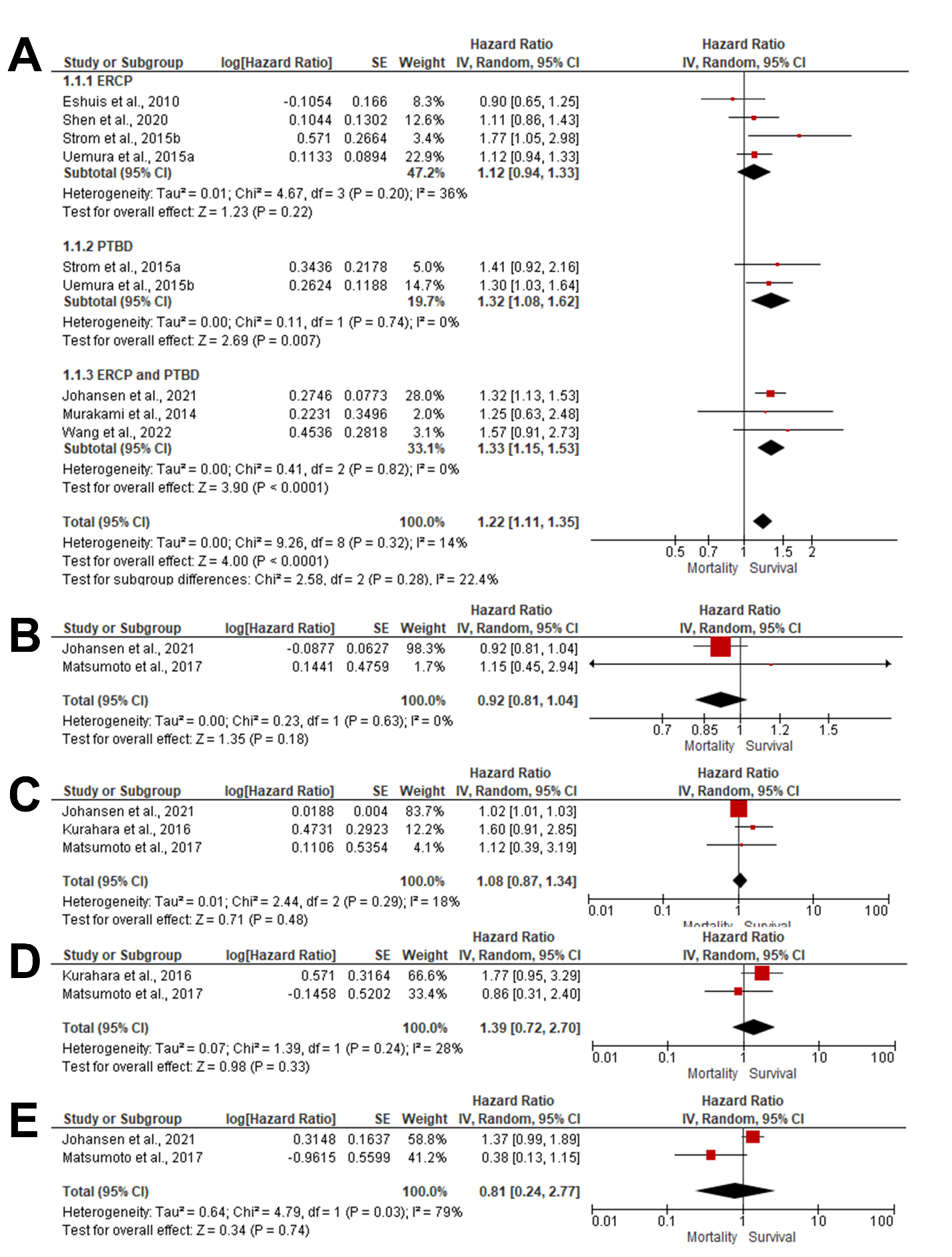
Figure: Figure1:Forest plot of summary analysis of the (A) Hazard ratio (HR) and 95% CI of the association between preoperative biliary drainage and overall survival (B) Hazard ratio (HR) and 95% CI of the association between female gender and overall survival (C) Hazard ratio (HR) and 95% CI of the association between age (years) and overall survival (D) Hazard ratio (HR) and 95% CI of the association between Serum Cancer antigen 19-9 and overall survival (E) Hazard ratio (HR) and 95% CI of the association between neoadjuvant therapy and overall survival. The size of red squares is proportional to the statistical weight of each trial. The Black diamond represents the pooled point estimate. The positioning of both diamonds and squares (along with 95% CIs) beyond the vertical line (unit value) suggests a significant outcome.
Disclosures:
Hasan Al-Obaidi indicated no relevant financial relationships.
Nooraldin Merza indicated no relevant financial relationships.
Osamah Muslim indicated no relevant financial relationships.
Omar Saab indicated no relevant financial relationships.
Mushfiqur Siddique indicated no relevant financial relationships.
Mohannad Bitar indicated no relevant financial relationships.
Sana Rabeeah indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Hayder Alamily indicated no relevant financial relationships.
Mustafa Al-Obaidi indicated no relevant financial relationships.
Amy Mackenzie indicated no relevant financial relationships.
Eunice Kwak indicated no relevant financial relationships.
Fatima Merza indicated no relevant financial relationships.
Yusuf Nawras indicated no relevant financial relationships.
Patel Manthanbhai indicated no relevant financial relationships.
Hussein Harb indicated no relevant financial relationships.
Abdallah Kobeissy indicated no relevant financial relationships.
Hasan Al-Obaidi, MD1, Nooraldin Merza, MD1, Osamah Muslim, MD2, Omar Saab, MD3, Mushfiqur Siddique, MD4, Mohannad Bitar, MD4, Sana Rabeeah, MD5, Bisher Sawaf, MD6, Hayder Alamily, MD7, Mustafa Al-Obaidi, MD8, Amy Mackenzie, MD9, Eunice Kwak, MD10, Fatima A. Merza, BS11, Yusuf Nawras, BSc1, Patel Manthanbhai, MD1, Hussein Harb, MD12, Abdallah Kobeissy, MD, MPH5. P2230 - Predictors of Survival Outcomes After Pre-Operative Biliary Drainage for Patients With Malignant Obstructive Jaundice and Pancreatic Carcinoma; A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
