Monday Poster Session
Category: Biliary/Pancreas
P2360 - A Case of Hypercalcemia Induced Acute Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hyder Alikhan, MD
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Hyder Alikhan, MD1, Chelsea Edirisuriya, MD1, William Lai, DO1, Sharan Parikh, DO2, Kunal Dalal, MD3
1Cooper University Hospital, Camden, NJ; 2Cooper University Health Care, Cherry Hill, NJ; 3Cooper University Health Care, Marlton, NJ
Introduction: Acute pancreatitis is a common abdominal concern; however, hypercalcemia is a rare etiology. Hypercalcemia induced pancreatitis has been previously reported in individuals with multiple myeloma or multiple parathyroid adenomas. We present a case of acute pancreatitis induced by hypercalcemia in a patient with a single parathyroid adenoma.
Case Description/
Methods: A 55-year-old female with no significant past medical history presents with acute epigastric pain with associated nausea and vomiting. Initial lab work revealed elevated calcium of 12.4 mg/dL, elevated lipase of 1,121 Units/L, intact parathyroid hormone (PTH) elevated at 165 pg/mL, and vitamin D levels were low at 11 ng/mL. CT scan revealed acute pancreatitis and 2.6 cm nodule that extended inferiorly off of the left thyroid lobe. Right upper quadrant ultrasound revealed cholelithiasis and gallbladder wall thickening, concerning for possible gallstone pancreatitis. However, magnetic resonance cholangiopancreatography (MRCP) revealed no evidence for choledocholithiasis and no biliary or pancreatic duct dilatation. Cholecystectomy was performed. Her symptoms continued to flare despite cholecystectomy. Endocrinology was consulted for hypercalcemia. Radionuclide parathyroid scintigraphy revealed left inferior gland uptake, consistent with parathyroid adenoma. 24-hour urine calcium and creatinine ruled out familial hypocalciuric hypercalcemia. Due to these findings, she then underwent left inferior parathyroidectomy with an appropriate drop of the intraoperative PTH from 325 pg/mL to 61 pg/mL. Pathology revealed atypical parathyroid adenoma. She was supplemented with 50,000 international units of vitamin D and 1 g elemental calcium to decrease the risk of post-op hypocalcemia.
Discussion: Hypercalcemia induced pancreatitis due to parathyroid adenoma is a curable cause of pancreatitis and is an indication for adenoma resection, especially in symptomatic cases. This diagnosis is often disregarded in setting of more common etiologies like in our patient's case, which led to an unnecessary inpatient cholecystectomy, excessive use of hospital resources, and longer hospital stay. Our case highlights the importance of multispecialty care in early diagnosis and broader investigation of etiology of pancreatitis, as delay may lead to worsening pancreatitis.
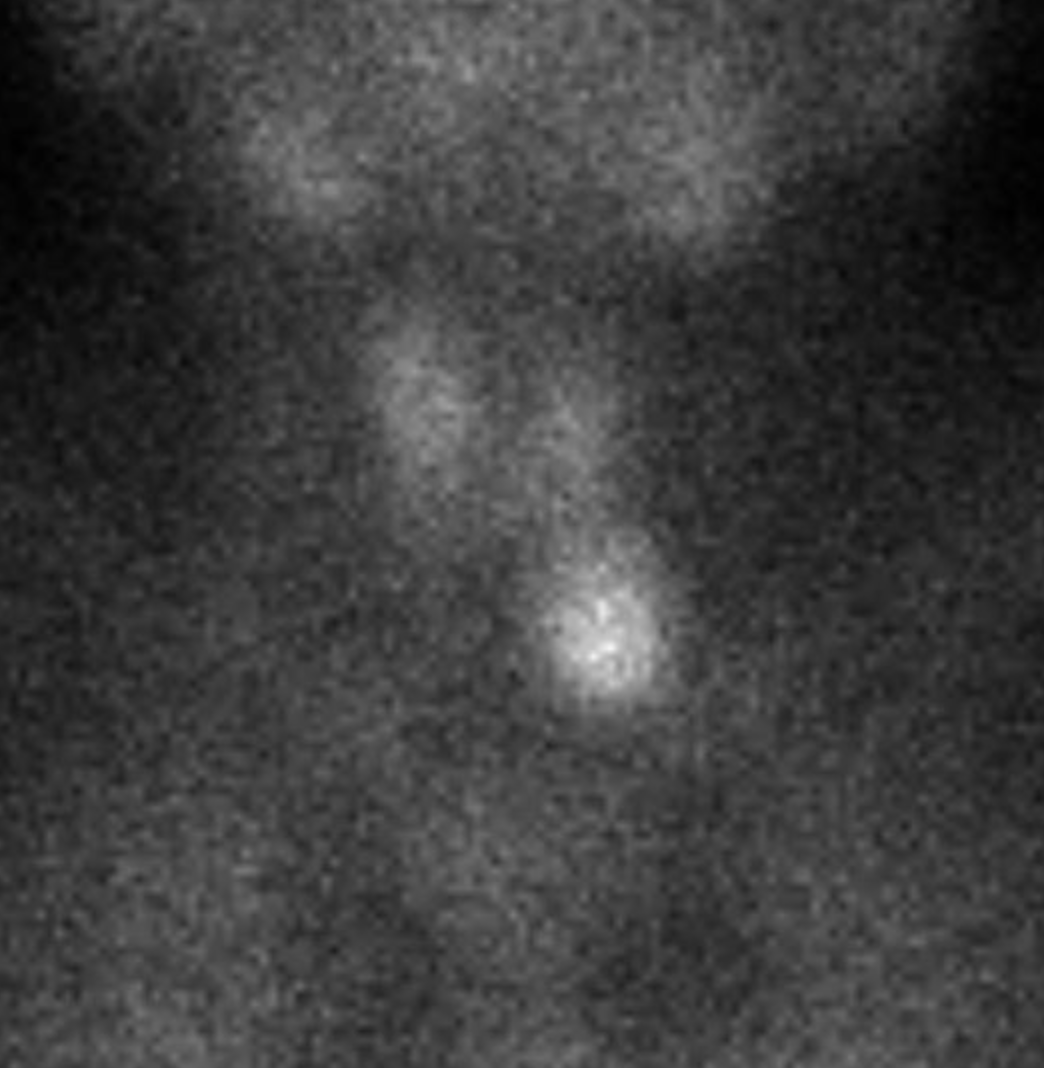
Figure: Figure 1. Radionuclide parathyroid scintigraphy with increased uptake of the left inferior parathyroid gland.
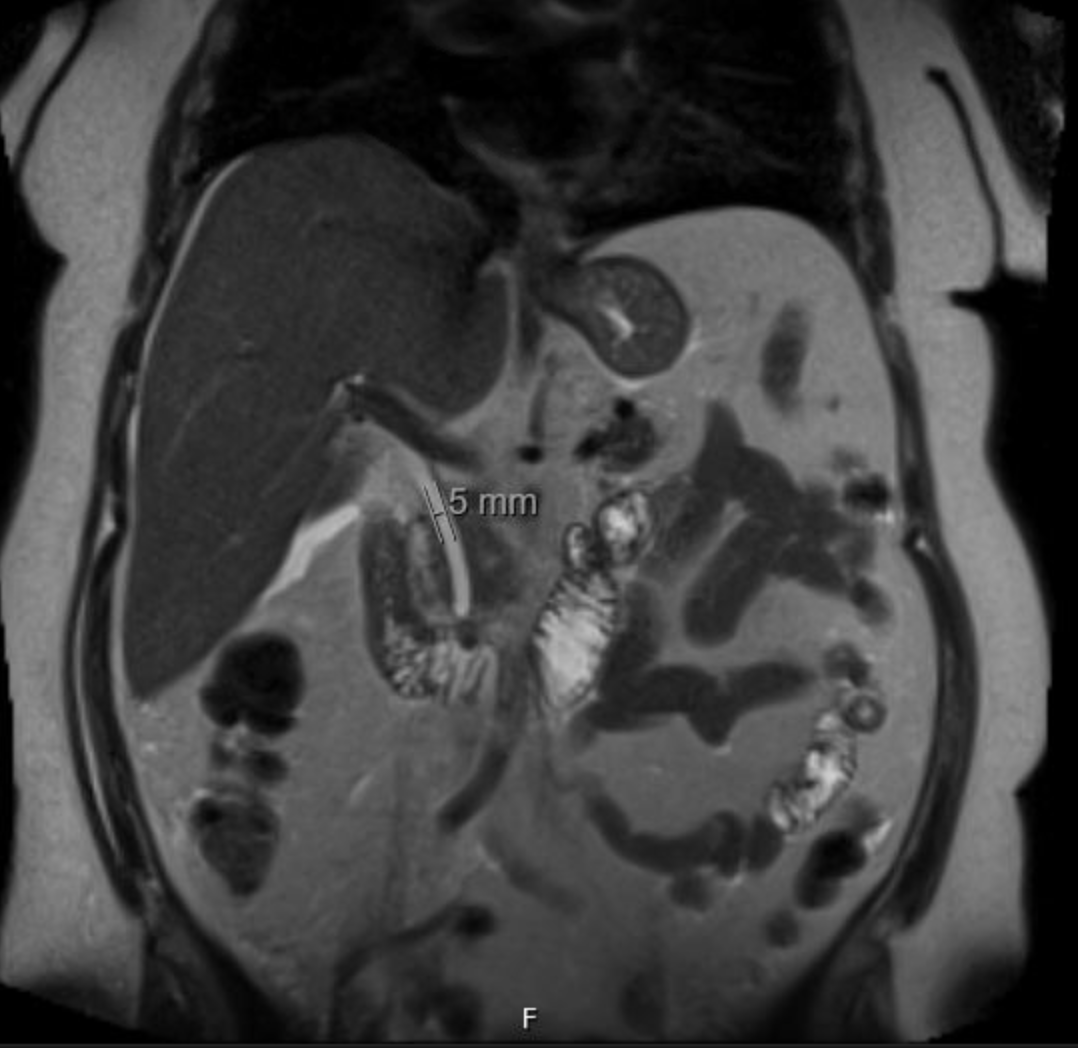
Figure: Figure 2. MRCP revealing no evidence of choledocholithiasis.
Disclosures:
Hyder Alikhan indicated no relevant financial relationships.
Chelsea Edirisuriya indicated no relevant financial relationships.
William Lai indicated no relevant financial relationships.
Sharan Parikh indicated no relevant financial relationships.
Kunal Dalal indicated no relevant financial relationships.
Hyder Alikhan, MD1, Chelsea Edirisuriya, MD1, William Lai, DO1, Sharan Parikh, DO2, Kunal Dalal, MD3. P2360 - A Case of Hypercalcemia Induced Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper University Health Care, Cherry Hill, NJ; 3Cooper University Health Care, Marlton, NJ
Introduction: Acute pancreatitis is a common abdominal concern; however, hypercalcemia is a rare etiology. Hypercalcemia induced pancreatitis has been previously reported in individuals with multiple myeloma or multiple parathyroid adenomas. We present a case of acute pancreatitis induced by hypercalcemia in a patient with a single parathyroid adenoma.
Case Description/
Methods: A 55-year-old female with no significant past medical history presents with acute epigastric pain with associated nausea and vomiting. Initial lab work revealed elevated calcium of 12.4 mg/dL, elevated lipase of 1,121 Units/L, intact parathyroid hormone (PTH) elevated at 165 pg/mL, and vitamin D levels were low at 11 ng/mL. CT scan revealed acute pancreatitis and 2.6 cm nodule that extended inferiorly off of the left thyroid lobe. Right upper quadrant ultrasound revealed cholelithiasis and gallbladder wall thickening, concerning for possible gallstone pancreatitis. However, magnetic resonance cholangiopancreatography (MRCP) revealed no evidence for choledocholithiasis and no biliary or pancreatic duct dilatation. Cholecystectomy was performed. Her symptoms continued to flare despite cholecystectomy. Endocrinology was consulted for hypercalcemia. Radionuclide parathyroid scintigraphy revealed left inferior gland uptake, consistent with parathyroid adenoma. 24-hour urine calcium and creatinine ruled out familial hypocalciuric hypercalcemia. Due to these findings, she then underwent left inferior parathyroidectomy with an appropriate drop of the intraoperative PTH from 325 pg/mL to 61 pg/mL. Pathology revealed atypical parathyroid adenoma. She was supplemented with 50,000 international units of vitamin D and 1 g elemental calcium to decrease the risk of post-op hypocalcemia.
Discussion: Hypercalcemia induced pancreatitis due to parathyroid adenoma is a curable cause of pancreatitis and is an indication for adenoma resection, especially in symptomatic cases. This diagnosis is often disregarded in setting of more common etiologies like in our patient's case, which led to an unnecessary inpatient cholecystectomy, excessive use of hospital resources, and longer hospital stay. Our case highlights the importance of multispecialty care in early diagnosis and broader investigation of etiology of pancreatitis, as delay may lead to worsening pancreatitis.
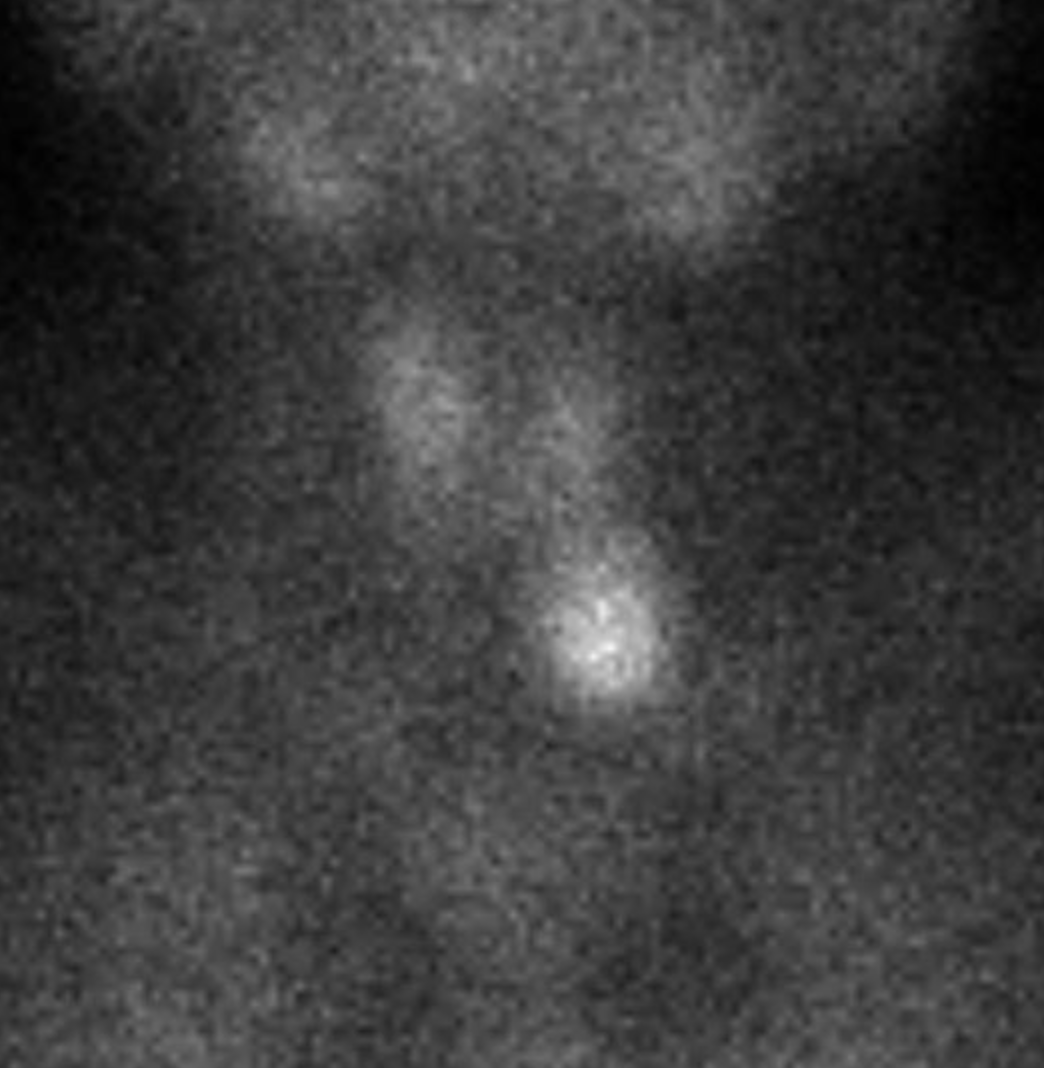
Figure: Figure 1. Radionuclide parathyroid scintigraphy with increased uptake of the left inferior parathyroid gland.
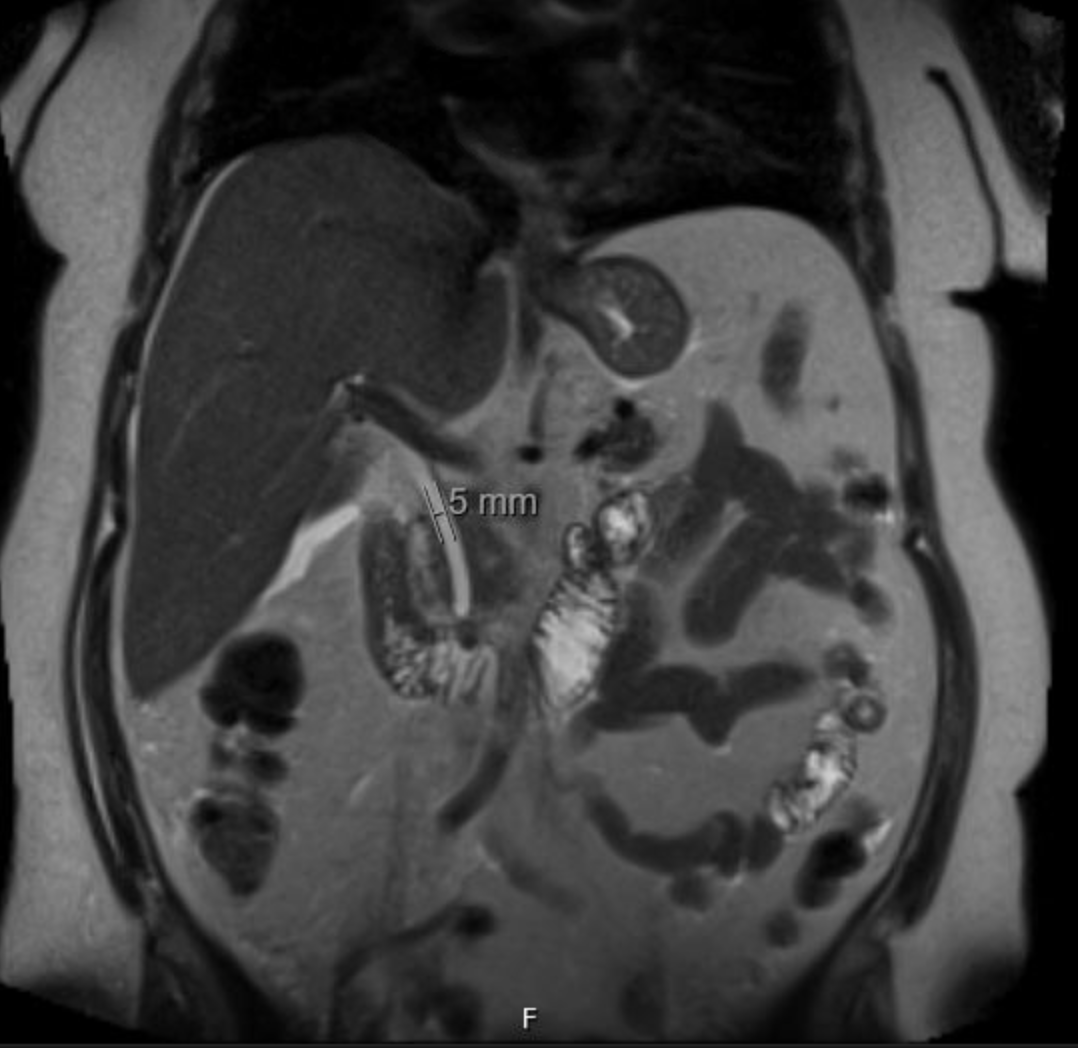
Figure: Figure 2. MRCP revealing no evidence of choledocholithiasis.
Disclosures:
Hyder Alikhan indicated no relevant financial relationships.
Chelsea Edirisuriya indicated no relevant financial relationships.
William Lai indicated no relevant financial relationships.
Sharan Parikh indicated no relevant financial relationships.
Kunal Dalal indicated no relevant financial relationships.
Hyder Alikhan, MD1, Chelsea Edirisuriya, MD1, William Lai, DO1, Sharan Parikh, DO2, Kunal Dalal, MD3. P2360 - A Case of Hypercalcemia Induced Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

