Monday Poster Session
Category: Biliary/Pancreas
P2358 - From Inflammation to Exsanguination: A Case of Severe Pancreatitis Complicated by a Fatal Hemorrhagic Pseudoaneurysm in a 23-Year-Old
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anjali Rajagopal, MBBS
University of Connecticut
Hartford, CT
Presenting Author(s)
Anjali Rajagopal, MBBS1, Ruchir Paladiya, MBBS2, Osama Siddique, MD3
1University of Connecticut, Hartford, CT; 2University of Connecticut School of Medicine, Farmington, CT; 3Connecticut GI, Wallingford, CT
Introduction: Severe acute pancreatitis (SAP) refers to AP with persistent organ failure in one or more organs for >48 hours and has mortality rates as high as 50%. Scoring systems & imaging alone do not accurately determine which patients develop severe pancreatitis. This case highlights clinical deterioration in a patient with an indolent presentation of alcoholic pancreatitis.
Case Description/
Methods: A 23-year-old woman with a history of alcohol use presented to the ED with worsening abdominal pain, nausea & retching over two weeks. She had prior visits for nausea & diarrhea; initially attributed to IBS. Patient was hemodynamically stable on admission & labs were notable for WBC 41.1 K/µL, Hb 15.1 g/dL Na 117 mEq/L, BUN 23 mg/dL, Ca 12.4 mg/dL, lactate 4.2 mmol/L, lipase 48 U/L. CECT of the abdomen & pelvis demonstrated severe pancreatitis with swelling, necrosis, & peripancreatic/free abdominal fluid. She received intravenous hydration and pain control. By day 4, hemoglobin dropped to 5.9 g/dL, with increased fluid collection & hemorrhagic features on CT. She was intubated for respiratory failure and required vasopressor support & blood transfusions in the ICU. Due to persistent abdominal pain, she underwent ERCP & cystogastrostomy and prophylactic IR embolization of the gastroduodenal artery & a dorsal pancreatic artery pseudoaneurysm. She later suffered a PEA arrest with ROSC achieved after six rounds of CPR. Due to a Hb of 5.3 & active hemorrhage on CTA massive transfusion protocol was initiated. She continued to decompensate with abdominal compartment syndrome and was not a candidate for ECMO. She was transitioned to comfort measures.
Discussion: Early (< 24 hours) prognostication of SAP remains challenging, despite the existence of scoring criteria. Only 20% of patients develop SAP, & sequelae such as pseudoaneurysms occur in 1.3-10% of patients, with 3% developing active bleeding independent of size. Management is guided by the size, anatomy, and hemodynamic status of the patient. Transcatheter arterial embolization is first line therapy however has a rebleeding rate of 10-20%. Other approaches include endovascular techniques such as coil embolization, EUS-guided procedures, percutaneous embolization, and surgical options in severe cases. Combined approaches with EUS-guided drainage are often used in patients with pancreatic fluid collections. Despite embolization, & transient improvement, our patient suffered fatal rupture, highlighting its unpredictable course.
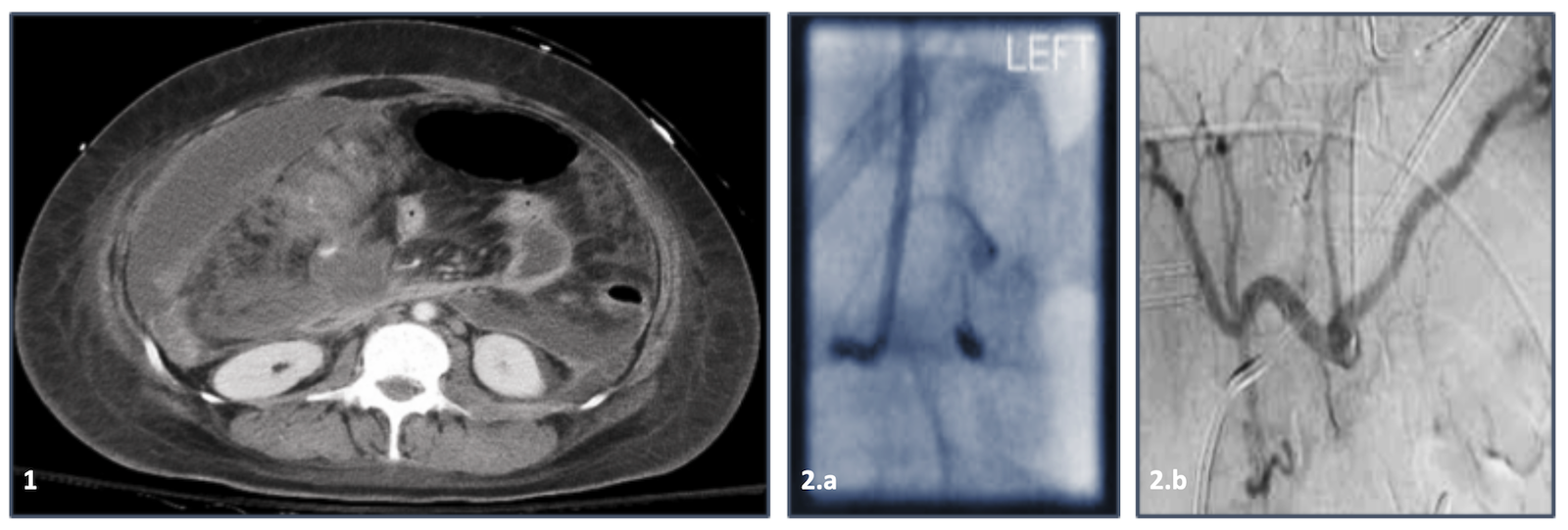
Figure: Fig. 1. CT abdomen/pelvis with contrast depicting worsening multifocal mixed density fluid collections in the abdomen and pelvis, with hemorrhagic components and extensive peripancreatic inflammatory changes.
Fig. 2.a&b depicting dorsal pancreatic artery and gastroduodenal artery pseudoaneurysms.
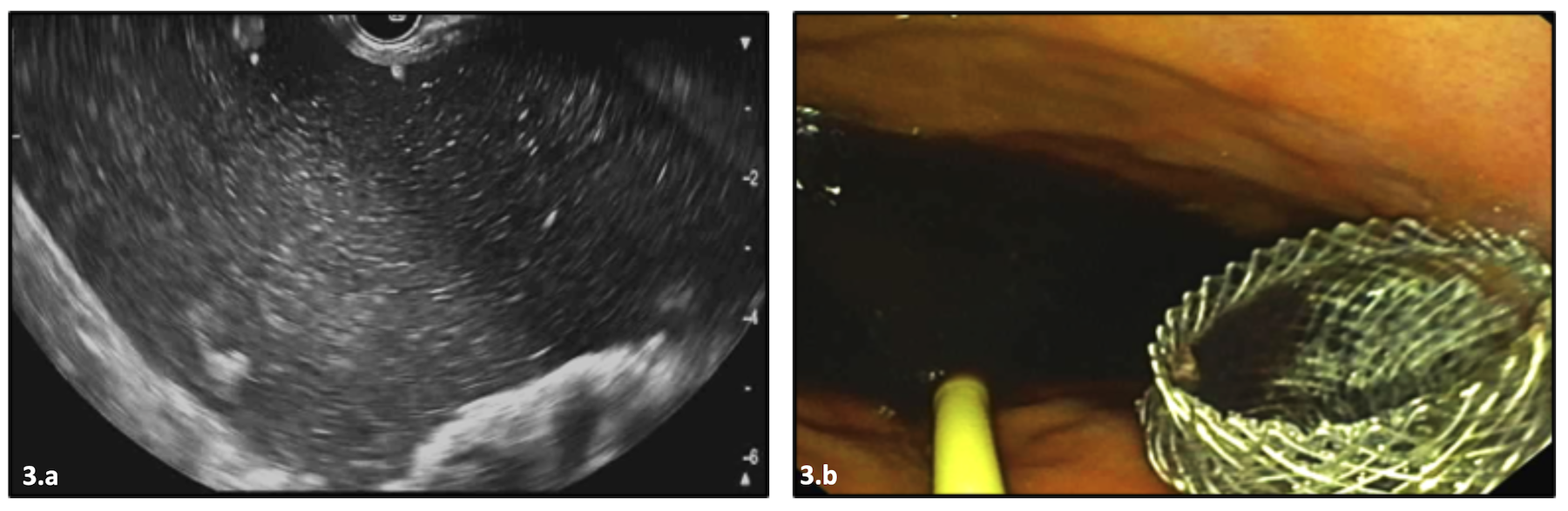
Figure: Fig. 3. Endoscopic ultrasound notable for cystic pancreatic head lesion.
Fig. 3.a depicting fluid collection. Fig. 3.b depicting the deployment of an AXIOS stent.
Disclosures:
Anjali Rajagopal indicated no relevant financial relationships.
Ruchir Paladiya indicated no relevant financial relationships.
Osama Siddique indicated no relevant financial relationships.
Anjali Rajagopal, MBBS1, Ruchir Paladiya, MBBS2, Osama Siddique, MD3. P2358 - From Inflammation to Exsanguination: A Case of Severe Pancreatitis Complicated by a Fatal Hemorrhagic Pseudoaneurysm in a 23-Year-Old, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut, Hartford, CT; 2University of Connecticut School of Medicine, Farmington, CT; 3Connecticut GI, Wallingford, CT
Introduction: Severe acute pancreatitis (SAP) refers to AP with persistent organ failure in one or more organs for >48 hours and has mortality rates as high as 50%. Scoring systems & imaging alone do not accurately determine which patients develop severe pancreatitis. This case highlights clinical deterioration in a patient with an indolent presentation of alcoholic pancreatitis.
Case Description/
Methods: A 23-year-old woman with a history of alcohol use presented to the ED with worsening abdominal pain, nausea & retching over two weeks. She had prior visits for nausea & diarrhea; initially attributed to IBS. Patient was hemodynamically stable on admission & labs were notable for WBC 41.1 K/µL, Hb 15.1 g/dL Na 117 mEq/L, BUN 23 mg/dL, Ca 12.4 mg/dL, lactate 4.2 mmol/L, lipase 48 U/L. CECT of the abdomen & pelvis demonstrated severe pancreatitis with swelling, necrosis, & peripancreatic/free abdominal fluid. She received intravenous hydration and pain control. By day 4, hemoglobin dropped to 5.9 g/dL, with increased fluid collection & hemorrhagic features on CT. She was intubated for respiratory failure and required vasopressor support & blood transfusions in the ICU. Due to persistent abdominal pain, she underwent ERCP & cystogastrostomy and prophylactic IR embolization of the gastroduodenal artery & a dorsal pancreatic artery pseudoaneurysm. She later suffered a PEA arrest with ROSC achieved after six rounds of CPR. Due to a Hb of 5.3 & active hemorrhage on CTA massive transfusion protocol was initiated. She continued to decompensate with abdominal compartment syndrome and was not a candidate for ECMO. She was transitioned to comfort measures.
Discussion: Early (< 24 hours) prognostication of SAP remains challenging, despite the existence of scoring criteria. Only 20% of patients develop SAP, & sequelae such as pseudoaneurysms occur in 1.3-10% of patients, with 3% developing active bleeding independent of size. Management is guided by the size, anatomy, and hemodynamic status of the patient. Transcatheter arterial embolization is first line therapy however has a rebleeding rate of 10-20%. Other approaches include endovascular techniques such as coil embolization, EUS-guided procedures, percutaneous embolization, and surgical options in severe cases. Combined approaches with EUS-guided drainage are often used in patients with pancreatic fluid collections. Despite embolization, & transient improvement, our patient suffered fatal rupture, highlighting its unpredictable course.
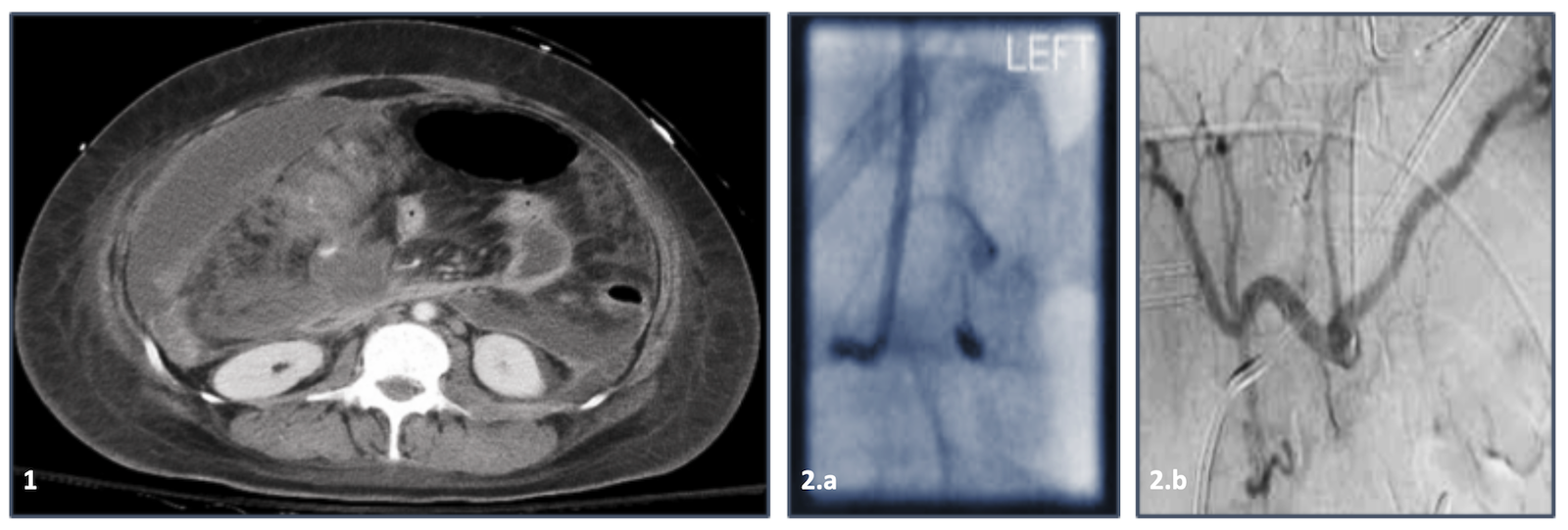
Figure: Fig. 1. CT abdomen/pelvis with contrast depicting worsening multifocal mixed density fluid collections in the abdomen and pelvis, with hemorrhagic components and extensive peripancreatic inflammatory changes.
Fig. 2.a&b depicting dorsal pancreatic artery and gastroduodenal artery pseudoaneurysms.
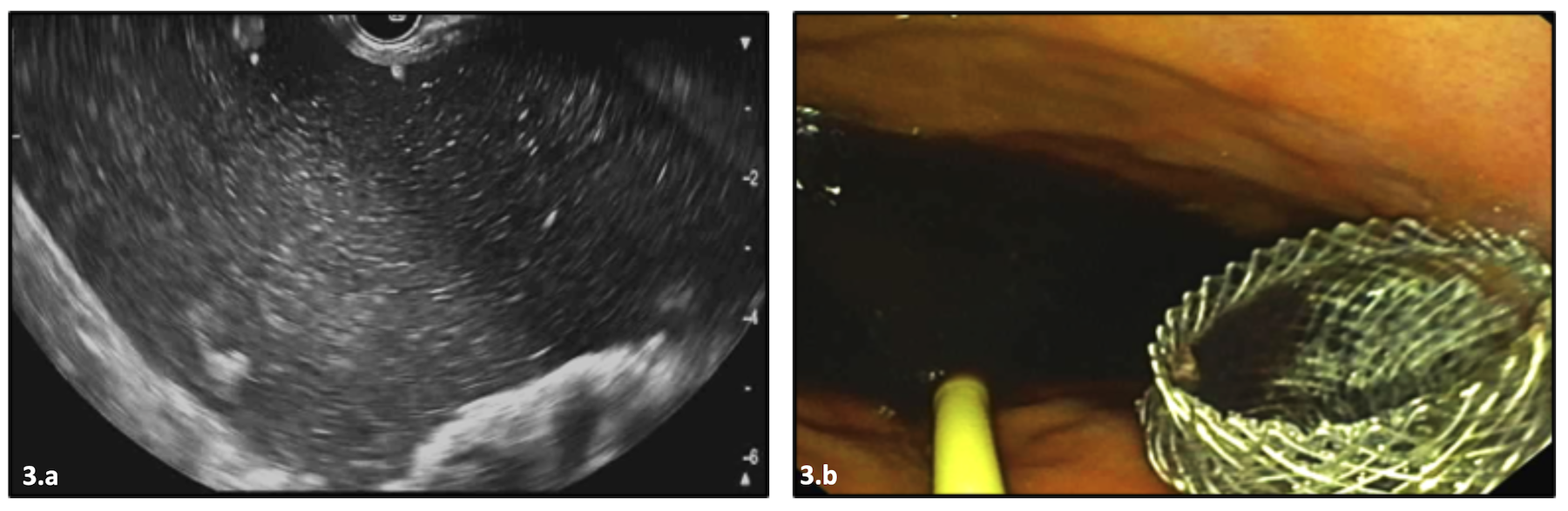
Figure: Fig. 3. Endoscopic ultrasound notable for cystic pancreatic head lesion.
Fig. 3.a depicting fluid collection. Fig. 3.b depicting the deployment of an AXIOS stent.
Disclosures:
Anjali Rajagopal indicated no relevant financial relationships.
Ruchir Paladiya indicated no relevant financial relationships.
Osama Siddique indicated no relevant financial relationships.
Anjali Rajagopal, MBBS1, Ruchir Paladiya, MBBS2, Osama Siddique, MD3. P2358 - From Inflammation to Exsanguination: A Case of Severe Pancreatitis Complicated by a Fatal Hemorrhagic Pseudoaneurysm in a 23-Year-Old, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
