Monday Poster Session
Category: Biliary/Pancreas
P2355 - Scleredema in a Patient With Autoimmune Pancreatitis: A Rare Clinical Finding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LA
Leen Azeez, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Leen Azeez, MD, Sungmo Hong, BS, Laura Rosenkranz, MD, Souleymane Y. Diallo, DO, MBA
University of Texas Health San Antonio, San Antonio, TX
Introduction: IgG4 related disease (IgG4-RD) is a systemic, pro-fibrotic condition that involves infiltration of IgG4+ plasma cells into organs with resultant masses. IgG4-RD skin manifestations are characterized by lymphoplasmacytic infiltrates and include cutaneous plasmacytosis and angiolymphoid hyperplasia among others. We present the case of scleredema, a rare skin manifestation in a patient diagnosed with autoimmune pancreatitis.
Case Description/
Methods: A 72-year-old man with sole history of prostate cancer treated with radiation presented to the emergency department with abdominal pain, headaches and nausea of 2-week duration. A diagnosis of acute pancreatitis was established, based on clinical presentation, lipase elevation of 483 U/L (13-60 U/L) and acute interstitial edematous pancreatitis with enlargement of the gland (sausage-like swelling) on CT scan. Further workup revealed an elevated serum IgG4 of 120.18 mg/dL (4 - 86 mg/dL), an IgG4/IgG index >10% and an enlarged pancreas on repeat imaging. Etiologies other than autoimmune disease were excluded. The patient remained asymptomatic following his presentation. Surveillance imaging showed a persistently swollen pancreas with mild diffuse peripancreatic edema (figure 1).
A year following the diagnosis of autoimmune pancreatitis, the patient developed firm, ill-defined, non-tender, non-pruritic subcutaneous nodules on both sides of the upper back (figure 2). Pathology from punch biopsy revealed lichenoid, perivascular and periadnexal infiltrates of mostly CD3+ and CD4+ lymphocytes, and fibrotic papillary dermal collagen consistent with dermal mucinosis (scleromyxedema).
Although the patient remained asymptomatic without recurrent acute pancreatitis episodes, a 12-week course of oral steroid therapy was proposed for the fibrotic skin rash. The course was not completed due to patient reluctance to array of adverse effects.
Discussion: Scleredema, which is characterized by glycosaminoglycans and collagen deposition in the dermis, is associated with paraproteinemia and long-standing diabetes mellitus but is rare in association with IgG4-RD. The patient did not have diabetes or other systemic conditions like multiple myeloma. The rash was deemed idiopathic by dermatology. While steroid and anti-CD19 monoclonal antibody therapies may be used for the systemic manifestations of IgG4-RD, it is unknown whether they would provide any benefits for IgG4- related scleredema. Intralesional steroids may be tried for the treatment of these fibrotic skin lesions.
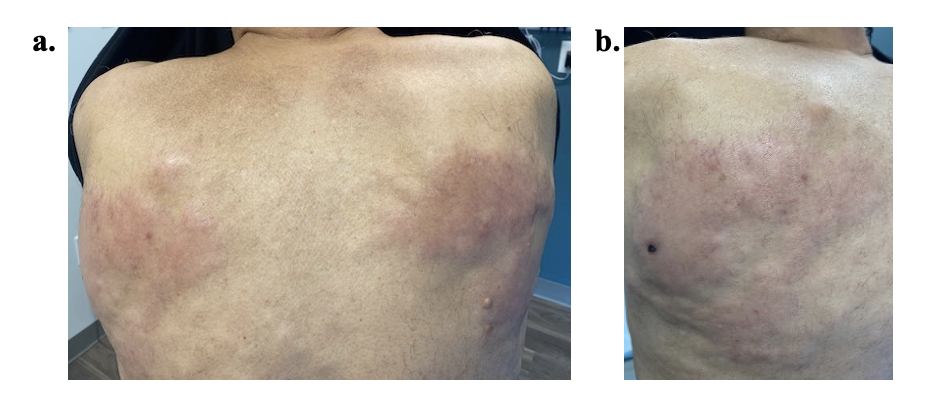
Figure: Figure 1. Surveillance imaging with multiphase computed tomography of the abdomen 10 months after the patient’s presentation with acute pancreatitis reveals an edematous pancreas, particularly in the distal body and tail, with peripancreatic fat stranding consistent with acute interstitial pancreatitis. No focal pancreatic lesions or dilation of the main pancreatic duct is noted.

Figure: Figure 2. Images of the firm, ill-defined, non-tender, non-pruritic subcutaneous nodules that appeared on both sides of the patient’s upper back one year after his presentation with acute pancreatitis.
Disclosures:
Leen Azeez indicated no relevant financial relationships.
Sungmo Hong indicated no relevant financial relationships.
Laura Rosenkranz indicated no relevant financial relationships.
Souleymane Diallo indicated no relevant financial relationships.
Leen Azeez, MD, Sungmo Hong, BS, Laura Rosenkranz, MD, Souleymane Y. Diallo, DO, MBA. P2355 - Scleredema in a Patient With Autoimmune Pancreatitis: A Rare Clinical Finding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: IgG4 related disease (IgG4-RD) is a systemic, pro-fibrotic condition that involves infiltration of IgG4+ plasma cells into organs with resultant masses. IgG4-RD skin manifestations are characterized by lymphoplasmacytic infiltrates and include cutaneous plasmacytosis and angiolymphoid hyperplasia among others. We present the case of scleredema, a rare skin manifestation in a patient diagnosed with autoimmune pancreatitis.
Case Description/
Methods: A 72-year-old man with sole history of prostate cancer treated with radiation presented to the emergency department with abdominal pain, headaches and nausea of 2-week duration. A diagnosis of acute pancreatitis was established, based on clinical presentation, lipase elevation of 483 U/L (13-60 U/L) and acute interstitial edematous pancreatitis with enlargement of the gland (sausage-like swelling) on CT scan. Further workup revealed an elevated serum IgG4 of 120.18 mg/dL (4 - 86 mg/dL), an IgG4/IgG index >10% and an enlarged pancreas on repeat imaging. Etiologies other than autoimmune disease were excluded. The patient remained asymptomatic following his presentation. Surveillance imaging showed a persistently swollen pancreas with mild diffuse peripancreatic edema (figure 1).
A year following the diagnosis of autoimmune pancreatitis, the patient developed firm, ill-defined, non-tender, non-pruritic subcutaneous nodules on both sides of the upper back (figure 2). Pathology from punch biopsy revealed lichenoid, perivascular and periadnexal infiltrates of mostly CD3+ and CD4+ lymphocytes, and fibrotic papillary dermal collagen consistent with dermal mucinosis (scleromyxedema).
Although the patient remained asymptomatic without recurrent acute pancreatitis episodes, a 12-week course of oral steroid therapy was proposed for the fibrotic skin rash. The course was not completed due to patient reluctance to array of adverse effects.
Discussion: Scleredema, which is characterized by glycosaminoglycans and collagen deposition in the dermis, is associated with paraproteinemia and long-standing diabetes mellitus but is rare in association with IgG4-RD. The patient did not have diabetes or other systemic conditions like multiple myeloma. The rash was deemed idiopathic by dermatology. While steroid and anti-CD19 monoclonal antibody therapies may be used for the systemic manifestations of IgG4-RD, it is unknown whether they would provide any benefits for IgG4- related scleredema. Intralesional steroids may be tried for the treatment of these fibrotic skin lesions.
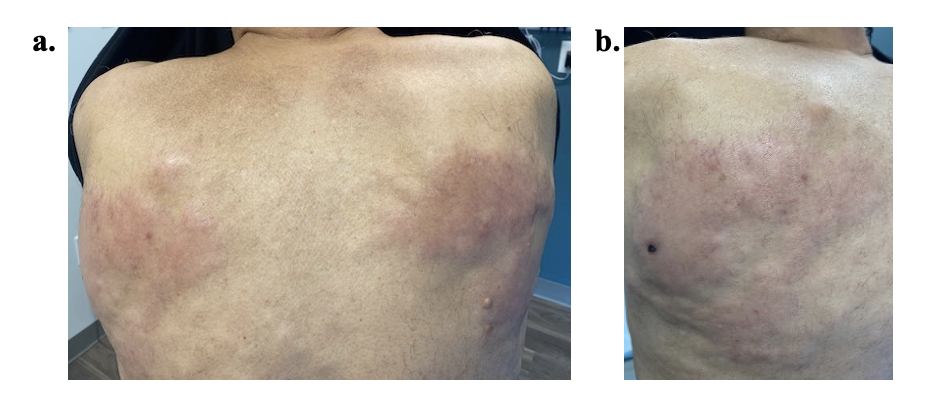
Figure: Figure 1. Surveillance imaging with multiphase computed tomography of the abdomen 10 months after the patient’s presentation with acute pancreatitis reveals an edematous pancreas, particularly in the distal body and tail, with peripancreatic fat stranding consistent with acute interstitial pancreatitis. No focal pancreatic lesions or dilation of the main pancreatic duct is noted.

Figure: Figure 2. Images of the firm, ill-defined, non-tender, non-pruritic subcutaneous nodules that appeared on both sides of the patient’s upper back one year after his presentation with acute pancreatitis.
Disclosures:
Leen Azeez indicated no relevant financial relationships.
Sungmo Hong indicated no relevant financial relationships.
Laura Rosenkranz indicated no relevant financial relationships.
Souleymane Diallo indicated no relevant financial relationships.
Leen Azeez, MD, Sungmo Hong, BS, Laura Rosenkranz, MD, Souleymane Y. Diallo, DO, MBA. P2355 - Scleredema in a Patient With Autoimmune Pancreatitis: A Rare Clinical Finding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
