Monday Poster Session
Category: Biliary/Pancreas
P2342 - A Rare Case of Hemoperitoneum in Acute Pancreatitis with Non-Arterial Source of Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TZ
Tiantian Zhang, MD, PhD
Department of Internal Medicine, University of Central Florida/HCA Florida West Hospital
Pensacola, FL
Presenting Author(s)
Tiantian Zhang, MD, PhD1, Peter Fahim, MD2
1Department of Internal Medicine, University of Central Florida/HCA Florida West Hospital, Pensacola, FL; 2Critical Care Medicine, University of Central Florida/HCA Florida West Hospital, Pensacola, FL
Introduction: Hemoperitoneum is a rare but potentially fatal complication of acute pancreatitis. It typically results from pseudoaneurysm rupture or arterial erosion. We present a case of hemoperitoneum in the absence of pseudoaneurysm or arterial extravasation, highlighting atypical hemorrhagic mechanisms.
Case Description/
Methods: A 43-year-old male with a history of alcohol use disorder, hypertension, asthma, and nephrolithiasis presented with severe epigastric pain radiating to the back. He reported intermittent abdominal pain over the past month, which had progressively worsened over the preceding two days. He denied any recent trauma. He was transferred from an outside hospital after imaging showed large hemoperitoneum.
On arrival, he was tachycardic and had diffuse abdominal tenderness. Laboratory studies revealed WBC 16.5 × 103/uL, hemoglobin of 11 g/dL. Platelets 237 × 103/uL, lipase 1051 U/L, amylase 241 U/L, ethanol level 47 mg/dL, and Coagulation parameters were within normal limits (PTT 19 seconds, INR 0.9). Lactic acid was normal.
CTA abdomen showed large-volume hemoperitoneum predominantly in the right upper quadrant, peripancreatic fat stranding, and suspected active extravasation near the gastroduodenal artery (GDA). Although angiography revealed no pseudoaneurysm or active arterial bleeding, hypervascularity in the GDA region prompted empiric coil embolization.
The patient was managed conservatively with intravenous fluids, analgesia, and serial abdominal exams. By hospital day 3, his hemoglobin remained stable, and his clinical condition improved. However, he left the hospital against medical advice.
Discussion: This case illustrates a rare instance of pancreatitis-associated hemoperitoneum without pseudoaneurysm or visible arterial extravasation. Potential etiologies include venous erosion, inflammatory vessel fragility, or occult vascular anomalies not detected by conventional imaging. In the presented case, empiric coil embolization of the GDA was performed despite the absence of active extravasation, reflecting a proactive approach to potential occult bleeding sources.
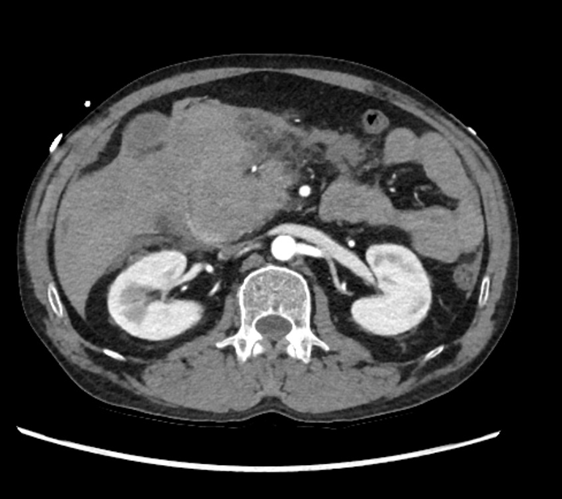
Figure: CT axial arterial phase: suspected crescentic contrast extravasation in the region of the descending portion of the duodenum.

Figure: Coronal delayed phase with large hemoperitoneum.
Disclosures:
Tiantian Zhang indicated no relevant financial relationships.
Peter Fahim indicated no relevant financial relationships.
Tiantian Zhang, MD, PhD1, Peter Fahim, MD2. P2342 - A Rare Case of Hemoperitoneum in Acute Pancreatitis with Non-Arterial Source of Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, University of Central Florida/HCA Florida West Hospital, Pensacola, FL; 2Critical Care Medicine, University of Central Florida/HCA Florida West Hospital, Pensacola, FL
Introduction: Hemoperitoneum is a rare but potentially fatal complication of acute pancreatitis. It typically results from pseudoaneurysm rupture or arterial erosion. We present a case of hemoperitoneum in the absence of pseudoaneurysm or arterial extravasation, highlighting atypical hemorrhagic mechanisms.
Case Description/
Methods: A 43-year-old male with a history of alcohol use disorder, hypertension, asthma, and nephrolithiasis presented with severe epigastric pain radiating to the back. He reported intermittent abdominal pain over the past month, which had progressively worsened over the preceding two days. He denied any recent trauma. He was transferred from an outside hospital after imaging showed large hemoperitoneum.
On arrival, he was tachycardic and had diffuse abdominal tenderness. Laboratory studies revealed WBC 16.5 × 103/uL, hemoglobin of 11 g/dL. Platelets 237 × 103/uL, lipase 1051 U/L, amylase 241 U/L, ethanol level 47 mg/dL, and Coagulation parameters were within normal limits (PTT 19 seconds, INR 0.9). Lactic acid was normal.
CTA abdomen showed large-volume hemoperitoneum predominantly in the right upper quadrant, peripancreatic fat stranding, and suspected active extravasation near the gastroduodenal artery (GDA). Although angiography revealed no pseudoaneurysm or active arterial bleeding, hypervascularity in the GDA region prompted empiric coil embolization.
The patient was managed conservatively with intravenous fluids, analgesia, and serial abdominal exams. By hospital day 3, his hemoglobin remained stable, and his clinical condition improved. However, he left the hospital against medical advice.
Discussion: This case illustrates a rare instance of pancreatitis-associated hemoperitoneum without pseudoaneurysm or visible arterial extravasation. Potential etiologies include venous erosion, inflammatory vessel fragility, or occult vascular anomalies not detected by conventional imaging. In the presented case, empiric coil embolization of the GDA was performed despite the absence of active extravasation, reflecting a proactive approach to potential occult bleeding sources.
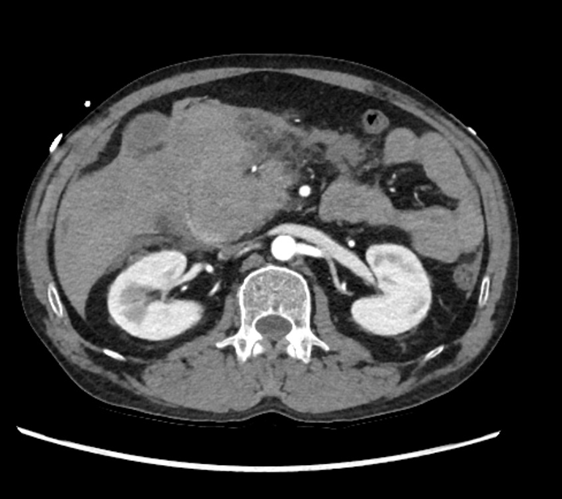
Figure: CT axial arterial phase: suspected crescentic contrast extravasation in the region of the descending portion of the duodenum.

Figure: Coronal delayed phase with large hemoperitoneum.
Disclosures:
Tiantian Zhang indicated no relevant financial relationships.
Peter Fahim indicated no relevant financial relationships.
Tiantian Zhang, MD, PhD1, Peter Fahim, MD2. P2342 - A Rare Case of Hemoperitoneum in Acute Pancreatitis with Non-Arterial Source of Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
