Monday Poster Session
Category: Biliary/Pancreas
P2338 - Hemobilia Presenting as Hematemesis in Acute Cholecystitis: A Rare Gastrointestinal Bleed
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Erika Haviland, DO (she/her/hers)
Louisiana State University
New Orleans, LA
Presenting Author(s)
Erika Haviland, DO1, Nikki Seraji, MD1, Catherine Loehr, MD1, Katherine Westbrook Cates, DO2, Daniel Raines, MD, FACG1
1Louisiana State University, New Orleans, LA; 2Louisiana State University School of Medicine, New Orleans, LA
Introduction: Hemobilia is relatively rare as a cause of gastrointestinal bleeds, and it usually presents itself as biliary colic. Most often it is caused by trauma from iatrogenic sources such as ERCP or surgery. Less commonly, it can be caused by hepatic or biliary malignancies. In a small percentage of cases, cholecystitis alone causes hemobilia1. Laboratory evaluation in cholecystitis is typically a hepatocellular pattern of injury. Rarely is acute cholecystitis without choledocolithiasis documented with both hepatocellular and cholestatic patterns of injury2. This case serves as a rare presentation of hemobilia, acute cholecystitis, and a mixed pattern of liver injury.
Case Description/
Methods: A 70-year-old female presented with a syncopal event after three days of vomiting, diarrhea and abdominal pain. Noted episodic events of dark stools and blood in emesis. On arrival, she was pale, hypotensive to 80/46, tachycardic to 110s. Labs as seen in figure 1. Was appropriately resuscitated with intravenous fluids, blood products and started on IV protonix. Had a witnessed episode of hematemesis.
Computed tomography angiography (CTA) of the abdomen showed an enlarged gallbladder with a thickened wall and multiple lamellated gallstones without biliary ductal dilatation. An abdominal ultrasound showed a partially distended gallbladder containing base intraluminal sludge/debris and shadowing stones. Esophagoduodenoscopy (EGD) showed red blood in duodenal bulb and second portion of the duodenum, with a blood clot visualized on the ampulla of Vater with some active oozing which raised suspicions for malignancy. MRCP showed a 2.5 cm gallbladder polyp. Pathology after robotic cholecystectomy showed grossly polypoid tissue protrusion into the gallbladder lumen with necrotic tissue, acute inflammation, and blot clot with no evidence of malignancy. The patient was discharged and two months after her discharge her liver function tests normalized.
Discussion: This case highlights a nonmalignant cause of hemobilia and importance of keeping on differential in cases of unclear sources of injury.
1. Zhornitskiy A, Berry R, Han JY, Tabibian JH. Hemobilia: Historical overview, clinical update, and current practices. Liver International. 2019;39(8):1378-1388. doi:10.1111/liv.1411
2. Padda MS, Singh S, Tang SJ, Rockey DC. Liver test patterns in patients with acute calculous cholecystitis and/or choledocholithiasis. Alimentary Pharmacology & Therapeutics. 2009;29(9):1011-1018. doi:10.1111/j.1365-2036.2009.03956.x

Figure: Figure 1: significant labs.
Image (below): There is a 2.5 cm pedunculated mass with homogeneous enhancement in the gallbladder neck. There is biliary sludge is well. The gallbladder is distended, measuring 6.0 cm in diameter. There is gallbladder wall thickening and pericholecystic edema. Moderate intrahepatic biliary ductal dilatation.
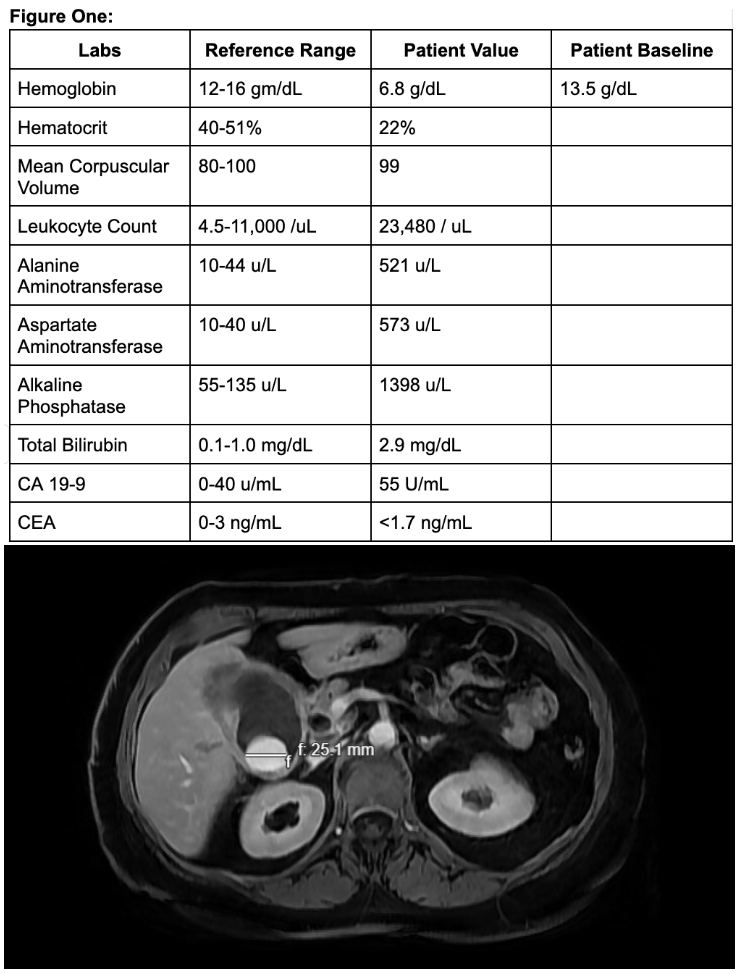
Figure: Left: bloot clot covering papilla. Right: polyp on the papilla with oozing seen into the second portion of duodenum.
Disclosures:
Erika Haviland indicated no relevant financial relationships.
Nikki Seraji indicated no relevant financial relationships.
Catherine Loehr indicated no relevant financial relationships.
Katherine Westbrook Cates indicated no relevant financial relationships.
Daniel Raines indicated no relevant financial relationships.
Erika Haviland, DO1, Nikki Seraji, MD1, Catherine Loehr, MD1, Katherine Westbrook Cates, DO2, Daniel Raines, MD, FACG1. P2338 - Hemobilia Presenting as Hematemesis in Acute Cholecystitis: A Rare Gastrointestinal Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Louisiana State University, New Orleans, LA; 2Louisiana State University School of Medicine, New Orleans, LA
Introduction: Hemobilia is relatively rare as a cause of gastrointestinal bleeds, and it usually presents itself as biliary colic. Most often it is caused by trauma from iatrogenic sources such as ERCP or surgery. Less commonly, it can be caused by hepatic or biliary malignancies. In a small percentage of cases, cholecystitis alone causes hemobilia1. Laboratory evaluation in cholecystitis is typically a hepatocellular pattern of injury. Rarely is acute cholecystitis without choledocolithiasis documented with both hepatocellular and cholestatic patterns of injury2. This case serves as a rare presentation of hemobilia, acute cholecystitis, and a mixed pattern of liver injury.
Case Description/
Methods: A 70-year-old female presented with a syncopal event after three days of vomiting, diarrhea and abdominal pain. Noted episodic events of dark stools and blood in emesis. On arrival, she was pale, hypotensive to 80/46, tachycardic to 110s. Labs as seen in figure 1. Was appropriately resuscitated with intravenous fluids, blood products and started on IV protonix. Had a witnessed episode of hematemesis.
Computed tomography angiography (CTA) of the abdomen showed an enlarged gallbladder with a thickened wall and multiple lamellated gallstones without biliary ductal dilatation. An abdominal ultrasound showed a partially distended gallbladder containing base intraluminal sludge/debris and shadowing stones. Esophagoduodenoscopy (EGD) showed red blood in duodenal bulb and second portion of the duodenum, with a blood clot visualized on the ampulla of Vater with some active oozing which raised suspicions for malignancy. MRCP showed a 2.5 cm gallbladder polyp. Pathology after robotic cholecystectomy showed grossly polypoid tissue protrusion into the gallbladder lumen with necrotic tissue, acute inflammation, and blot clot with no evidence of malignancy. The patient was discharged and two months after her discharge her liver function tests normalized.
Discussion: This case highlights a nonmalignant cause of hemobilia and importance of keeping on differential in cases of unclear sources of injury.
1. Zhornitskiy A, Berry R, Han JY, Tabibian JH. Hemobilia: Historical overview, clinical update, and current practices. Liver International. 2019;39(8):1378-1388. doi:10.1111/liv.1411
2. Padda MS, Singh S, Tang SJ, Rockey DC. Liver test patterns in patients with acute calculous cholecystitis and/or choledocholithiasis. Alimentary Pharmacology & Therapeutics. 2009;29(9):1011-1018. doi:10.1111/j.1365-2036.2009.03956.x

Figure: Figure 1: significant labs.
Image (below): There is a 2.5 cm pedunculated mass with homogeneous enhancement in the gallbladder neck. There is biliary sludge is well. The gallbladder is distended, measuring 6.0 cm in diameter. There is gallbladder wall thickening and pericholecystic edema. Moderate intrahepatic biliary ductal dilatation.
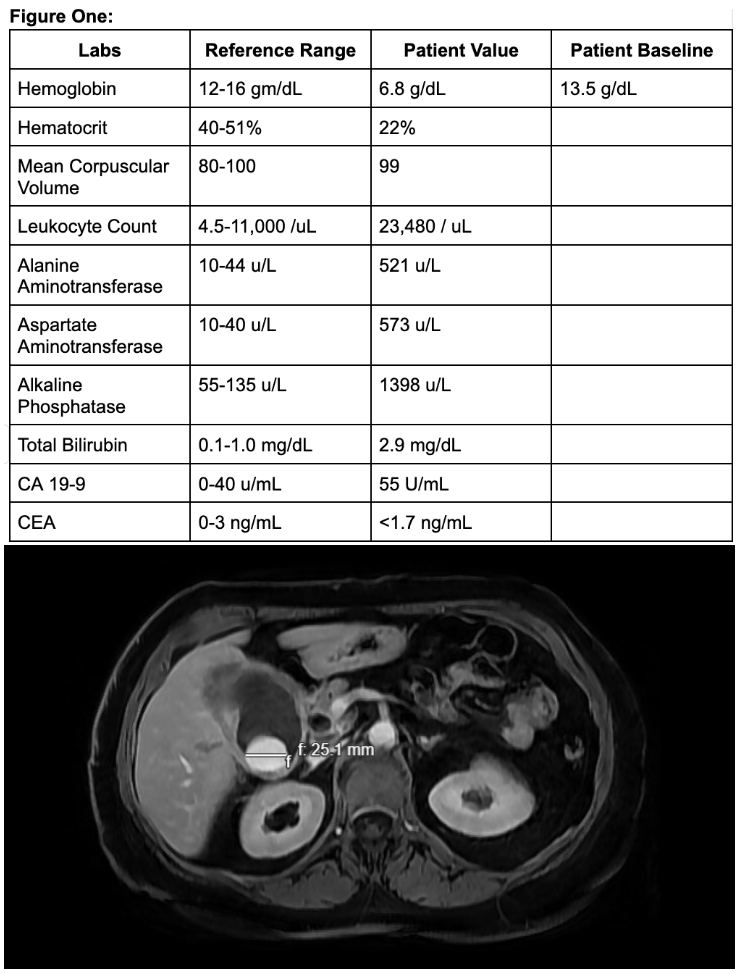
Figure: Left: bloot clot covering papilla. Right: polyp on the papilla with oozing seen into the second portion of duodenum.
Disclosures:
Erika Haviland indicated no relevant financial relationships.
Nikki Seraji indicated no relevant financial relationships.
Catherine Loehr indicated no relevant financial relationships.
Katherine Westbrook Cates indicated no relevant financial relationships.
Daniel Raines indicated no relevant financial relationships.
Erika Haviland, DO1, Nikki Seraji, MD1, Catherine Loehr, MD1, Katherine Westbrook Cates, DO2, Daniel Raines, MD, FACG1. P2338 - Hemobilia Presenting as Hematemesis in Acute Cholecystitis: A Rare Gastrointestinal Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
