Monday Poster Session
Category: Colon
P2464 - Unusual Case of Solitary Colonic Ganglioneuroma in a Patient with Neurofibromatosis Type 1
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Gabriella Mohring, BS (she/her/hers)
Geisinger Commonwealth School of Medicine
Scranton, PA
Presenting Author(s)
Gabriella Mohring, BS1, Mahdi Taye, MD1, Danial Nadeem, MD2, Sara Waqar, MD3, John Boger, MD2
1Geisinger Commonwealth School of Medicine, Scranton, PA; 2Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 3Geisinger Health System, Danville, PA
Introduction: Neuroblastic tumors originate from neural crest cells and are classified into neuroblastomas, ganglioneuroblastomas, and ganglioneuromas. These span a clinical spectrum from malignant to benign, with a median age of presentation of approximately 7 years. They typically occur in the posterior mediastinum, retroperitoneum, adrenal glands, and neck, but may arise anywhere along the peripheral sympathetic nervous system. We present a rare case of a solitary colonic ganglioneuroma identified during diagnostic workup for symptomatic diverticulosis in an adult with neurofibromatosis type 1 (NF1).
Case Description/
Methods: A 51-year-old male with sarcoidosis and NF1 presented with subacute diarrhea, weight loss, nausea, vomiting, and left lower quadrant pain. Contrast-enhanced computed tomography (CT) revealed diffuse colonic diverticulosis but no mass or inflammation. Colonoscopy showed a 7 mm sessile polyp in the transverse colon and a 25 mm soft, compressible sigmoid lesion with a positive “pillow sign.” Biopsies revealed Schwann cell proliferation and fibroadipose tissue, with strong S100 positivity.
Given the lesion’s size and submucosal appearance, resection was pursued, and the patient underwent laparoscopic sigmoidectomy. Pathology confirmed a 1.9 × 1.7 cm exophytic, polypoid, benign spindle cell lesion with ganglion cells involving mucosa through superficial muscularis propria, consistent with ganglioneuroma. Immunohistochemistry showed S100-positive neural fibers and actin- and desmin-positive smooth muscle bundles. CD34 and CD117 were negative; MIB-1 index < 1%. Follow-up colonoscopies at 1, 5, and 8 years revealed no recurrence of disease.
Discussion: Colonic ganglioneuromas are rare benign tumors, often identified incidentally during endoscopic evaluation. While diffuse forms may be syndromic, solitary lesions are typically sporadic. However, isolated lesions can occur in patients with NF1, making syndromic association uncertain and reinforcing the need for individualized evaluation. The “pillow sign,” commonly associated with lipomas, highlights the need for histologic confirmation. In this case, the absence of recurrence over eight years suggests routine surveillance may not be necessary after complete excision of isolated, nonsyndromic lesions.
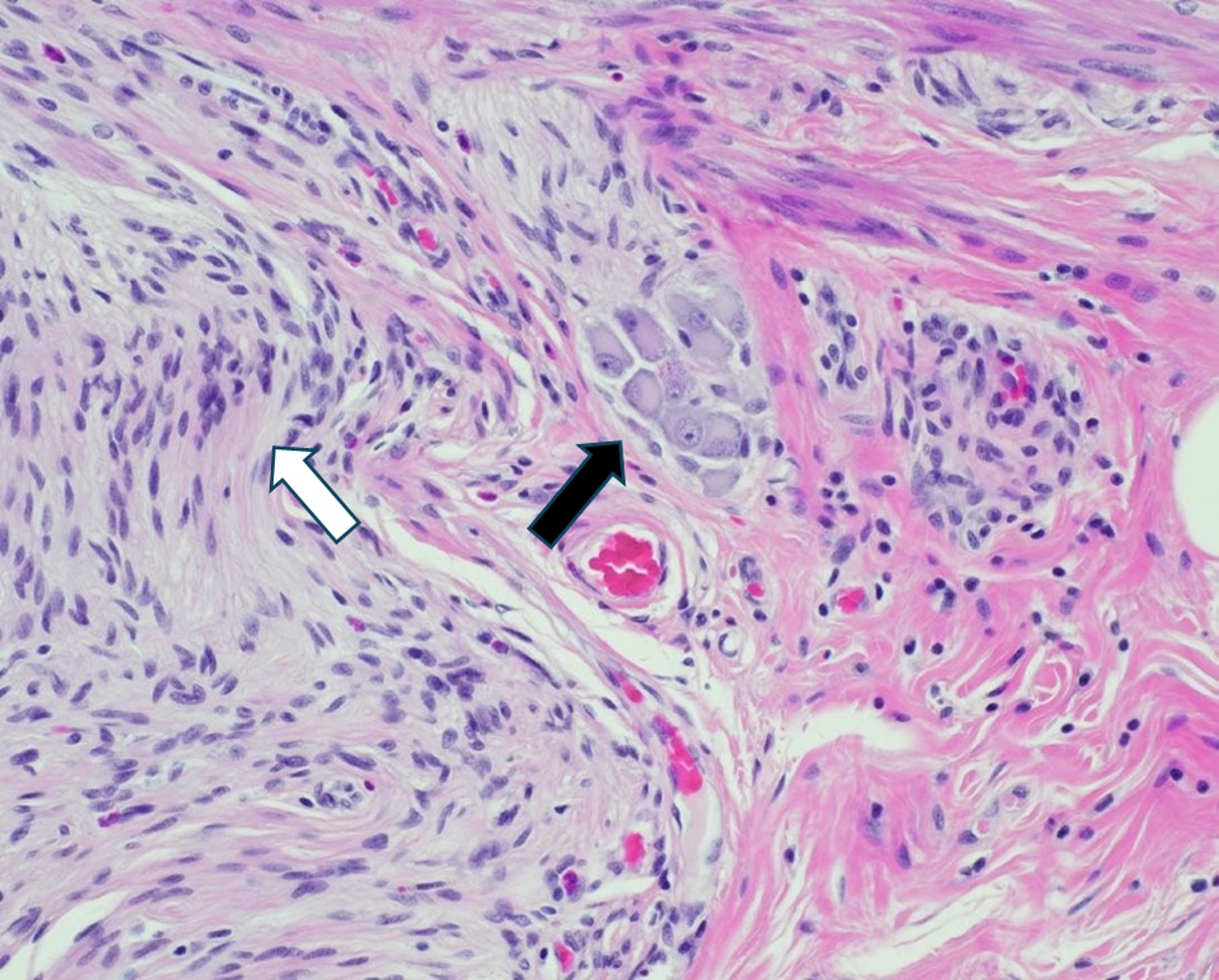
Figure: Figure 1: H&E stain showing a small cluster of mature ganglion cells centrally (black arrow), surrounded by a proliferation of bland spindle-shaped Schwann cells with wavy nuclei and a characteristic whorled pattern, consistent with ganglioneuroma (white arrow).
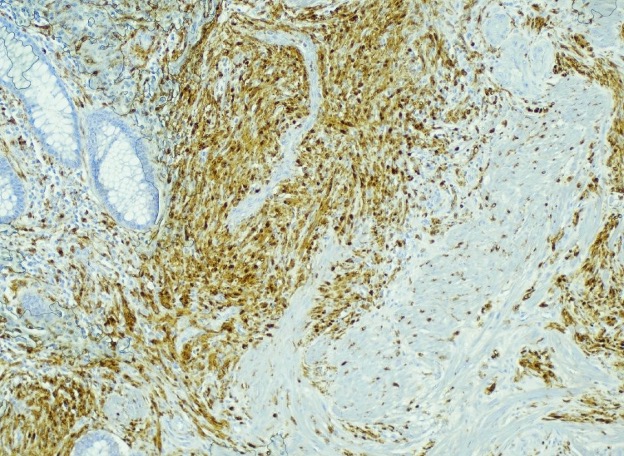
Figure: Figure 2: Immunohistochemical staining for S100 shows diffuse strong positivity in spindle cells, indicating neural crest origin and consistent with Schwannian differentiation.
Disclosures:
Gabriella Mohring indicated no relevant financial relationships.
Mahdi Taye indicated no relevant financial relationships.
Danial Nadeem indicated no relevant financial relationships.
Sara Waqar indicated no relevant financial relationships.
John Boger indicated no relevant financial relationships.
Gabriella Mohring, BS1, Mahdi Taye, MD1, Danial Nadeem, MD2, Sara Waqar, MD3, John Boger, MD2. P2464 - Unusual Case of Solitary Colonic Ganglioneuroma in a Patient with Neurofibromatosis Type 1, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Commonwealth School of Medicine, Scranton, PA; 2Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 3Geisinger Health System, Danville, PA
Introduction: Neuroblastic tumors originate from neural crest cells and are classified into neuroblastomas, ganglioneuroblastomas, and ganglioneuromas. These span a clinical spectrum from malignant to benign, with a median age of presentation of approximately 7 years. They typically occur in the posterior mediastinum, retroperitoneum, adrenal glands, and neck, but may arise anywhere along the peripheral sympathetic nervous system. We present a rare case of a solitary colonic ganglioneuroma identified during diagnostic workup for symptomatic diverticulosis in an adult with neurofibromatosis type 1 (NF1).
Case Description/
Methods: A 51-year-old male with sarcoidosis and NF1 presented with subacute diarrhea, weight loss, nausea, vomiting, and left lower quadrant pain. Contrast-enhanced computed tomography (CT) revealed diffuse colonic diverticulosis but no mass or inflammation. Colonoscopy showed a 7 mm sessile polyp in the transverse colon and a 25 mm soft, compressible sigmoid lesion with a positive “pillow sign.” Biopsies revealed Schwann cell proliferation and fibroadipose tissue, with strong S100 positivity.
Given the lesion’s size and submucosal appearance, resection was pursued, and the patient underwent laparoscopic sigmoidectomy. Pathology confirmed a 1.9 × 1.7 cm exophytic, polypoid, benign spindle cell lesion with ganglion cells involving mucosa through superficial muscularis propria, consistent with ganglioneuroma. Immunohistochemistry showed S100-positive neural fibers and actin- and desmin-positive smooth muscle bundles. CD34 and CD117 were negative; MIB-1 index < 1%. Follow-up colonoscopies at 1, 5, and 8 years revealed no recurrence of disease.
Discussion: Colonic ganglioneuromas are rare benign tumors, often identified incidentally during endoscopic evaluation. While diffuse forms may be syndromic, solitary lesions are typically sporadic. However, isolated lesions can occur in patients with NF1, making syndromic association uncertain and reinforcing the need for individualized evaluation. The “pillow sign,” commonly associated with lipomas, highlights the need for histologic confirmation. In this case, the absence of recurrence over eight years suggests routine surveillance may not be necessary after complete excision of isolated, nonsyndromic lesions.
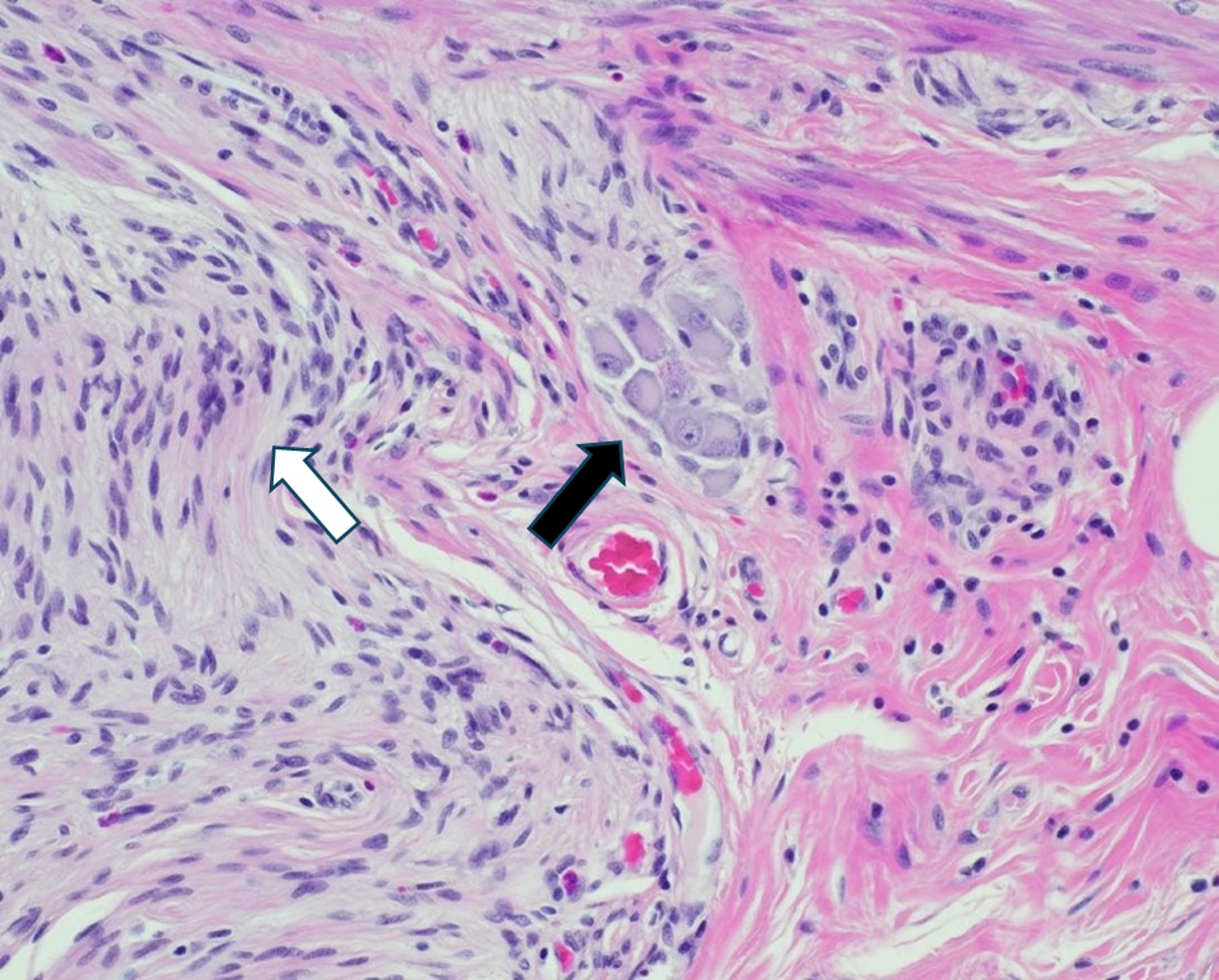
Figure: Figure 1: H&E stain showing a small cluster of mature ganglion cells centrally (black arrow), surrounded by a proliferation of bland spindle-shaped Schwann cells with wavy nuclei and a characteristic whorled pattern, consistent with ganglioneuroma (white arrow).
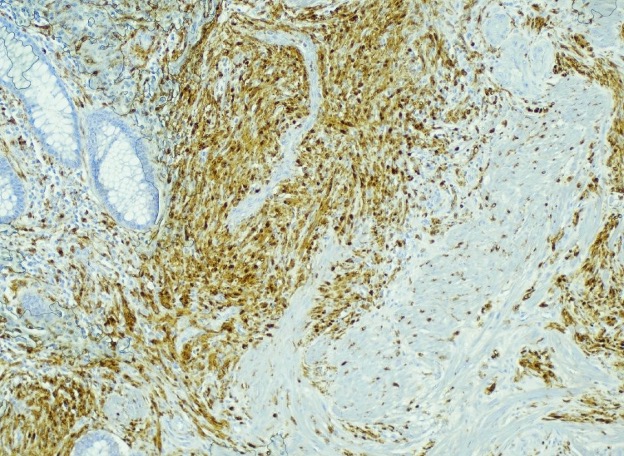
Figure: Figure 2: Immunohistochemical staining for S100 shows diffuse strong positivity in spindle cells, indicating neural crest origin and consistent with Schwannian differentiation.
Disclosures:
Gabriella Mohring indicated no relevant financial relationships.
Mahdi Taye indicated no relevant financial relationships.
Danial Nadeem indicated no relevant financial relationships.
Sara Waqar indicated no relevant financial relationships.
John Boger indicated no relevant financial relationships.
Gabriella Mohring, BS1, Mahdi Taye, MD1, Danial Nadeem, MD2, Sara Waqar, MD3, John Boger, MD2. P2464 - Unusual Case of Solitary Colonic Ganglioneuroma in a Patient with Neurofibromatosis Type 1, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

