Monday Poster Session
Category: Colon
P2463 - The Road Less Traveled: Rectal Metastasis of Prostate Adenocarcinoma

Karim Al Annan, MD (he/him/his)
University of Connecticut Health Center
Hartford, CT
Presenting Author(s)
1University of Connecticut Health Center, Hartford, CT; 2University of Connecticut Health, Farmington, CT; 3University of Connecticut Health Center, Farmington, CT; 4Hospital of Central Connecticut, New Britian, CT
Introduction:
Prostate cancer is one of the most common malignancies in men. Its often indolent course can lead to delayed clinical presentations, frequently accompanied by metastatic spread to regional lymph nodes, bone, and liver. We report a rare case of rectal metastasis from prostate cancer.
Case Description/
Methods:
A 75-year-old male with a history of Gleason 8 prostate cancer status post radical prostatectomy with bilateral pelvic lymph node dissection 10 years prior presented with subacute left lower quadrant abdominal pain and unintentional weight loss of 28 pounds over two months. Otherwise, he was clinically and hemodynamically stable, with an unremarkable initial laboratory workup. Contrast-enhanced CT of the abdomen and pelvis showed a 7.4 × 5.6 × 4.8 cm heterogeneous rectal mass invading the mesorectal fascia and bladder, with retroperitoneal lymphadenopathy (Fig. 1).
Colonoscopy was performed, revealing a 4 cm submucosal, non-obstructing rectal mass located 8 cm from the anal verge, which was biopsied (Fig. 1). Histopathology demonstrated poorly differentiated metastatic adenocarcinoma of prostatic origin, confirmed by positive NKX3.1 immunostaining (Fig. 2). Notably, PSA levels were elevated at 10.86 ng/ml. The patient was referred to oncology for staging and initiation of androgen-deprivation therapy along with chemotherapy.
Discussion:
Prostate cancer poses diagnostic challenges due to its slow-growing nature and limitations in lab testing, including PSA levels. This often results in patients presenting with metastatic disease, with symptoms varying depending on the site of spread. Our patient endorsed nonspecific symptoms of weight loss and abdominal pain, initially suggesting colorectal cancer as the source of his rectal mass based on imaging and endoscopic appearance. However, histopathologic evaluation confirmed metastatic prostate adenocarcinoma. This diagnostic pitfall underscores the importance of considering prior malignancies in the differential diagnosis of new gastrointestinal lesions. Proposed mechanisms for this presentation include shared lymphatic pathways and disruption of Denonvilliers’ fascia from prior surgical intervention, facilitating local invasion of the rectal wall. Recognizing such metastatic presentations is crucial, as management differs significantly from that of primary colorectal cancer and typically involves systemic therapy rather than surgical resection.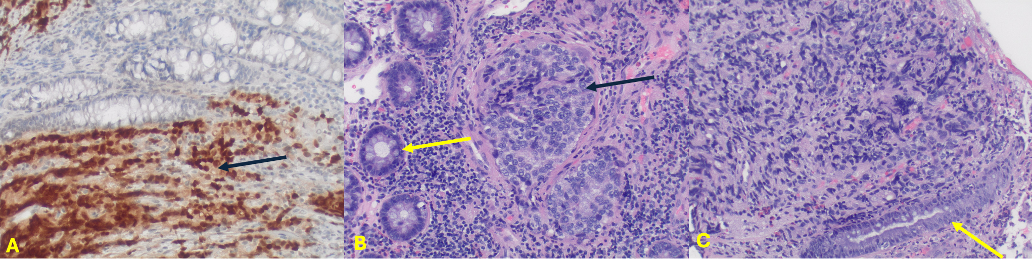
Figure: Figure 1. Colonoscopy images (A&B) highlighting rectal mass (yellow arrows) and contrast-enhanced CT images in coronal (C) and axial (D) views of rectal mass (black arrows).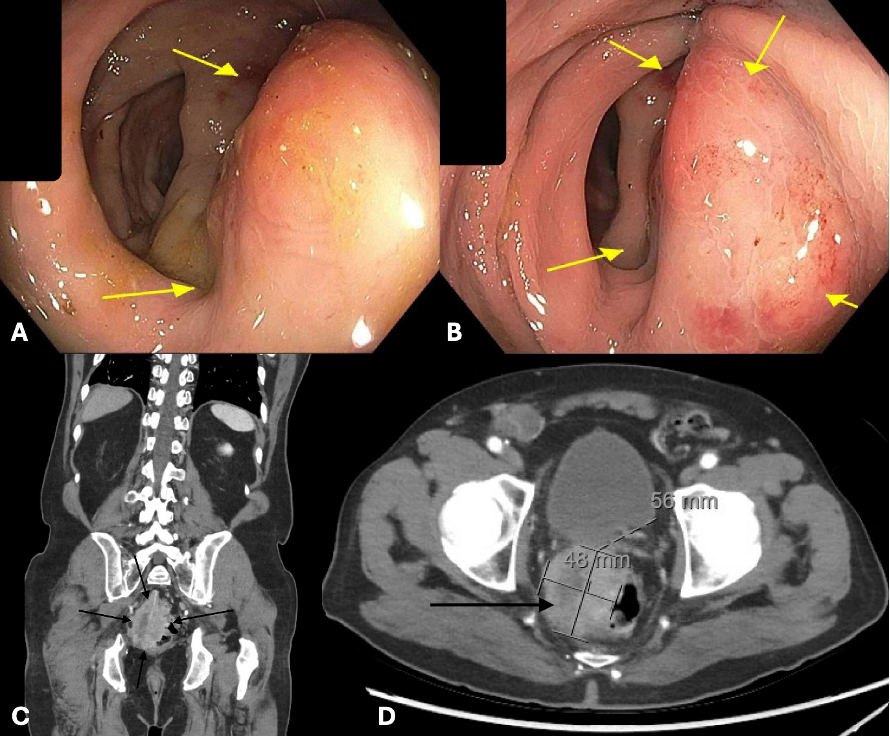
Figure: Figure 2. Histopathologic and immunohistochemical evaluation of rectal mass biopsy demonstrating metastatic prostatic adenocarcinoma.
(A) Immunohistochemistry for NKX3.1 showing strong nuclear positivity (dark-brown staining) in malignant cells infiltrating rectal tissue, confirming prostatic origin (black arrow). Magnification: 40x.
(B&C) H&E stain revealing poorly differentiated cells with solid nests, exhibiting cellular atypia with a high nuclear-to-cytoplasmic ratio and absence of gland formation (black arrow). Overlying normal colonic glands and crypts are noted (yellow arrows). Magnification: (B) 40x, (C) 20x.
Disclosures:
Karim Al Annan indicated no relevant financial relationships.
Rachael Hagen indicated no relevant financial relationships.
Minh-Thu Nguyen indicated no relevant financial relationships.
Alexander Potashinsky indicated no relevant financial relationships.
Karim Al Annan, MD1, Rachael Hagen, DO2, Minh-Thu Nguyen, MD3, Alexander Potashinsky, MD4. P2463 - The Road Less Traveled: Rectal Metastasis of Prostate Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
