Monday Poster Session
Category: Colon
P2459 - Is the Rising Incidence of Colorectal Neuroendocrine Tumors Masking Persistent Mortality Disparities?

Silpa Choday, MD (she/her/hers)
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
1Creighton University School of Medicine, Phoenix, AZ; 2Arizona Digestive Health, GI Alliance, Glendale, AZ
Introduction:
Colorectal neuroendocrine tumors (CRNETs) are a rare and increasingly recognized malignancy with variable outcomes. We aimed to characterize these trends using a large, population-based dataset to identify disparities in CRNET
Methods: We analyzed SEER 17-registry data (2000–2022) to calculate age-adjusted incidence and mortality rates for colorectal neuroendocrine tumors (CRNET). Trends were assessed using annual percentage changes (APCs) via log-linear and joinpoint regression, and adjusted rate ratios using multivariable Poisson regression. Analyses were conducted using SEER*Stat v8.4.4, Joinpoint v5.4.0, and STATA v18.
Results:
The overall age-adjusted incidence of CRNET was 1.3 per 100,000 population (95% CI: 1.3–1.3), with the highest rates observed among Non-Hispanic Black (NHB) individuals (2.2; 95% CI: 2.1–2.2), nearly twice that of Non-Hispanic Whites (NHW) (1.2; 95% CI: 1.2–1.1). Most tumors were localized at diagnosis across all groups. Age-adjusted mortality was low overall (0.4 in men, 0.3 in women), but NHB individuals exhibited the highest mortality (0.6; 95% CI: 0.6–0.7), over double that of NHW.
From 2000–2022, incidence rose significantly in nearly all demographic groups, with sharp increases observed in NHW males (APC = 19.1%, 2012–2015) and American Indian/Alaska Native (AI/AN) females (APC = 26.6%, 2012–2017). Localized-stage tumors drove most of the increase (APC = 5.89%; 95% CI: 4.10–7.45), with more modest gains in regional and distant stages.
Mortality rates also increased steadily (APC = 6.35% in men, 6.51% in women; p < 0.001). NHB and AI/ANs experienced the most rapid long-term mortality growth. Localized-stage mortality rose sharply (APC = 9.24%), while regional and distant-stage deaths showed minimal or non-significant change.
Incidence rate ratios (IRRs) confirmed a 19% increase per 5-year age increment (IRR = 1.19; p < 0.001), and a significantly higher burden among males and NHB individuals (IRR = 2.18). Mortality rose 33% per 5-year age increment (IRR = 1.33) and was highest among NHB (IRR = 2.50; p < 0.001). Rate ratios confirmed higher incidence and mortality with age, male sex, and NHB race.
Discussion:
CRNET incidence has risen across all racial/ethnic groups, with the fastest increases in Hispanics and non-Hispanic Asian/Pacific Islanders. NHB faces the highest mortality, especially from distant-stage disease. While localized-stage mortality has improved, distant-stage outcomes remain unchanged, underscoring growing disparities in diagnosis and care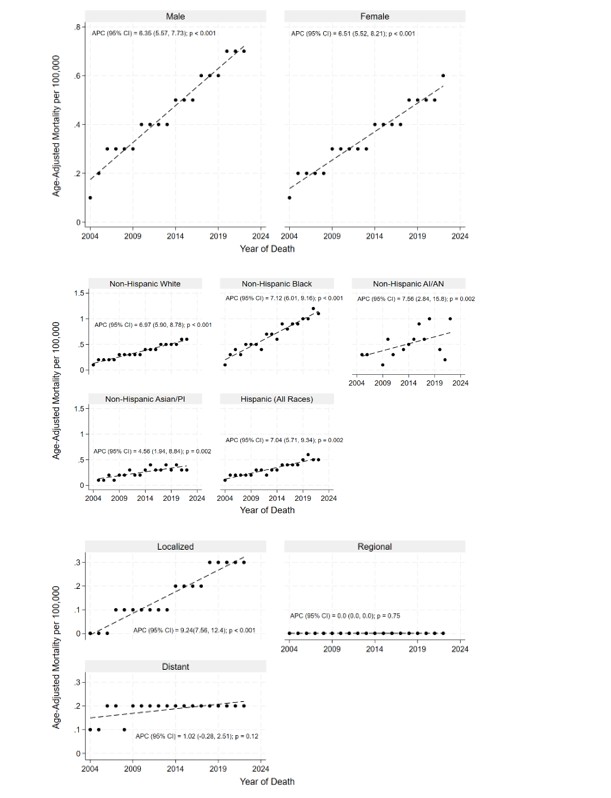
Figure: Table 1. Age-Adjusted Incidence Rates of CRNET by Sex, Race/Ethnicity and Stage at Diagnosis with further stratification by race/ethnicity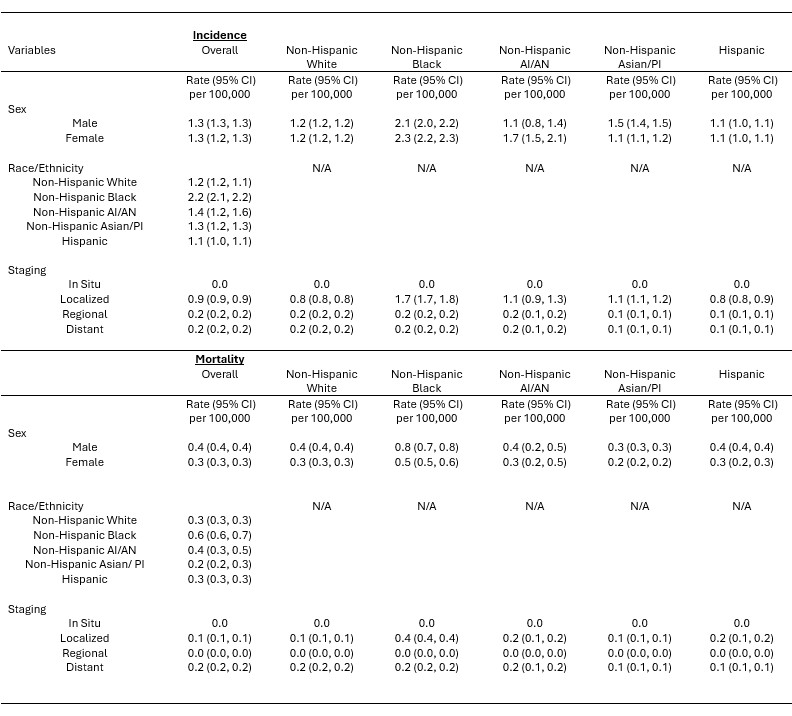
Figure: Figure 1. Annual Percent Change in Age-Adjusted Mortality Rates of CRNET by Sex, Race/Ethnicity and Stage at Diagnosis.
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Anthony Yeung indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Savio Reddymasu indicated no relevant financial relationships.
Silpa Choday, MD1, Anthony Yeung, MD1, Keng-Yu Chuang, MD2, Neil Vyas, MD1, Savio Reddymasu, MD1. P2459 - Is the Rising Incidence of Colorectal Neuroendocrine Tumors Masking Persistent Mortality Disparities?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
