Monday Poster Session
Category: Colon
P2550 - CVID-Associated Colitis Presenting as Chronic Diarrhea and Mimicking IBD
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sophia Pimpinelli, MD
Robert Wood Johnson Medical School, Rutgers University
New Brunswick, NJ
Presenting Author(s)
Sophia Pimpinelli, MD1, Mansi Sheth, DO2, Anish V. Patel, MD1
1Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ; 2Jefferson Torresdale Hospital, Bridgewater, NJ
Introduction: Common variable immunodeficiency (CVID) is a primary immunodeficiency characterized by low serum levels of immunoglobulins, leading to increased susceptibility to infections. Gastrointestinal (GI) manifestations are common in CVID, with diarrhea being the primary symptom of GI involvement. Although distinct entities, CVID-associated colitis (CAC) can present with clinical and endoscopic features that mimic Inflammatory Bowel Disease (IBD), posing a diagnostic challenge.
Case Description/
Methods: A 34-year-old male with CVID on biweekly immune globulin therapy presented with rectal bleeding. He reports five months of watery bowel movements (up to five daily), intermittent hematochezia (1-2 times a week) and tenesmus. Laboratory studies showed: white blood cell count of 1.23, hemoglobin 6.9 and potassium 2.9. Stool studies were negative for infectious etiology (culture, ova & parasites, Giardia). He underwent a colonoscopy that showed diffuse mucosal erythema, friability, exudates and altered vascularity (Figure 1) with small, scattered erosions, most prominent in the rectum. Biopsies revealed mild to moderate active colitis, absent plasma cells and without crypt distortion or granulomas. Staining for cytomegalovirus was negative. Fecal calprotectin was 2,450 mcg/g. The patient was begun on Mesalamine therapy (combination 4.8gm oral and 1gm rectal once daily). Three months later, the patient reported clinical improvement: 1–2 non-bloody stools daily and minimal rectal discomfort.
Discussion: We report a case of CAC presenting as chronic diarrhea and mimicking IBD. This case highlights the overlap in presentation and management considerations between CAC and IBD. In CVID, infectious diarrhea is common, but 10–12% develop non-infectious entero-colopathy resembling IBD. An astute pathologist is essential in aiding diagnosis. Histologically, CAC may show absent plasma cells, CD8+ T-cell–predominant infiltrates, goblet cell loss, apoptosis, villous blunting with or without crypt destruction. IBD typically features crypt distortion, abscesses, ulceration, and plasma cell–rich infiltrates. The absence of plasma cells favors CVID as with our patient. Immune globulin therapy itself may not be effective in treatment and mucosal healing. Although mesalamine is not traditionally effective in CVID-colitis, this patient showed a favorable response. Differentiating between CAC and IBD is crucial, as it influences treatment strategy and prognosis.
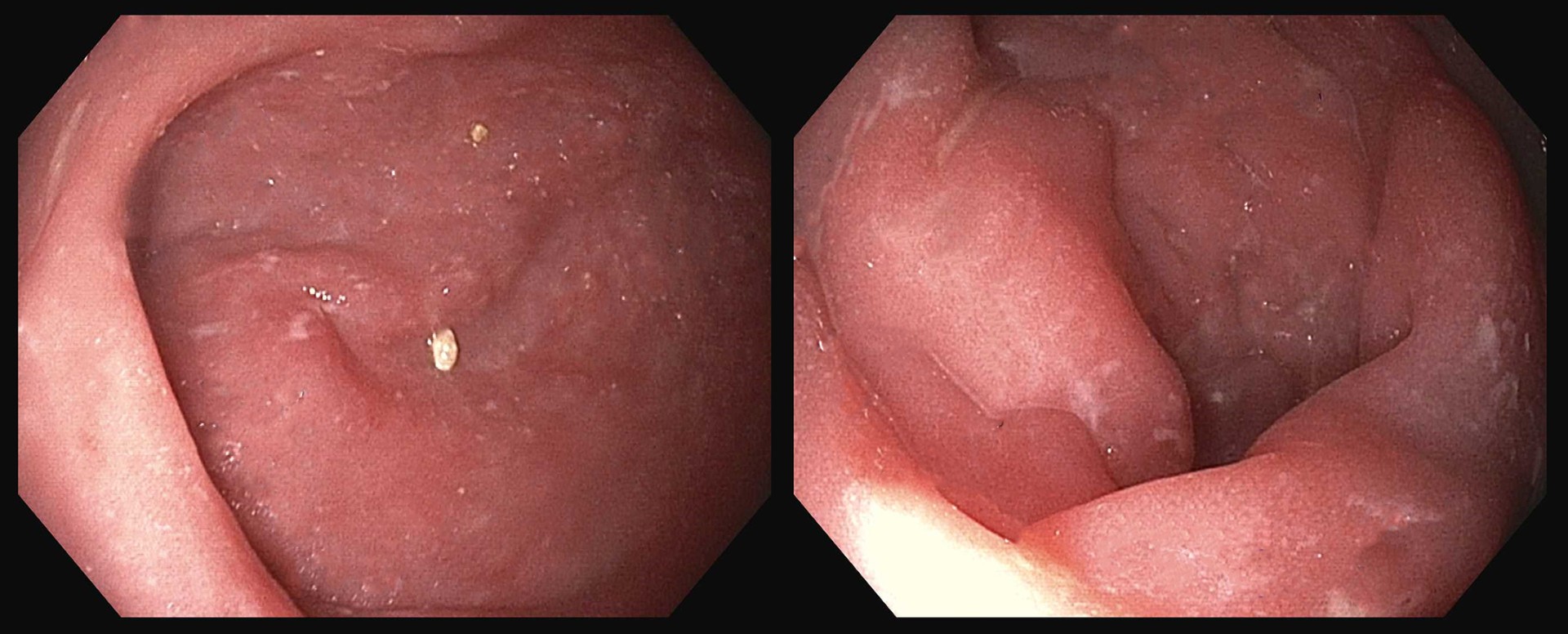
Figure: CVID colitis on colonoscopy
Disclosures:
Sophia Pimpinelli indicated no relevant financial relationships.
Mansi Sheth indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Sophia Pimpinelli, MD1, Mansi Sheth, DO2, Anish V. Patel, MD1. P2550 - CVID-Associated Colitis Presenting as Chronic Diarrhea and Mimicking IBD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ; 2Jefferson Torresdale Hospital, Bridgewater, NJ
Introduction: Common variable immunodeficiency (CVID) is a primary immunodeficiency characterized by low serum levels of immunoglobulins, leading to increased susceptibility to infections. Gastrointestinal (GI) manifestations are common in CVID, with diarrhea being the primary symptom of GI involvement. Although distinct entities, CVID-associated colitis (CAC) can present with clinical and endoscopic features that mimic Inflammatory Bowel Disease (IBD), posing a diagnostic challenge.
Case Description/
Methods: A 34-year-old male with CVID on biweekly immune globulin therapy presented with rectal bleeding. He reports five months of watery bowel movements (up to five daily), intermittent hematochezia (1-2 times a week) and tenesmus. Laboratory studies showed: white blood cell count of 1.23, hemoglobin 6.9 and potassium 2.9. Stool studies were negative for infectious etiology (culture, ova & parasites, Giardia). He underwent a colonoscopy that showed diffuse mucosal erythema, friability, exudates and altered vascularity (Figure 1) with small, scattered erosions, most prominent in the rectum. Biopsies revealed mild to moderate active colitis, absent plasma cells and without crypt distortion or granulomas. Staining for cytomegalovirus was negative. Fecal calprotectin was 2,450 mcg/g. The patient was begun on Mesalamine therapy (combination 4.8gm oral and 1gm rectal once daily). Three months later, the patient reported clinical improvement: 1–2 non-bloody stools daily and minimal rectal discomfort.
Discussion: We report a case of CAC presenting as chronic diarrhea and mimicking IBD. This case highlights the overlap in presentation and management considerations between CAC and IBD. In CVID, infectious diarrhea is common, but 10–12% develop non-infectious entero-colopathy resembling IBD. An astute pathologist is essential in aiding diagnosis. Histologically, CAC may show absent plasma cells, CD8+ T-cell–predominant infiltrates, goblet cell loss, apoptosis, villous blunting with or without crypt destruction. IBD typically features crypt distortion, abscesses, ulceration, and plasma cell–rich infiltrates. The absence of plasma cells favors CVID as with our patient. Immune globulin therapy itself may not be effective in treatment and mucosal healing. Although mesalamine is not traditionally effective in CVID-colitis, this patient showed a favorable response. Differentiating between CAC and IBD is crucial, as it influences treatment strategy and prognosis.
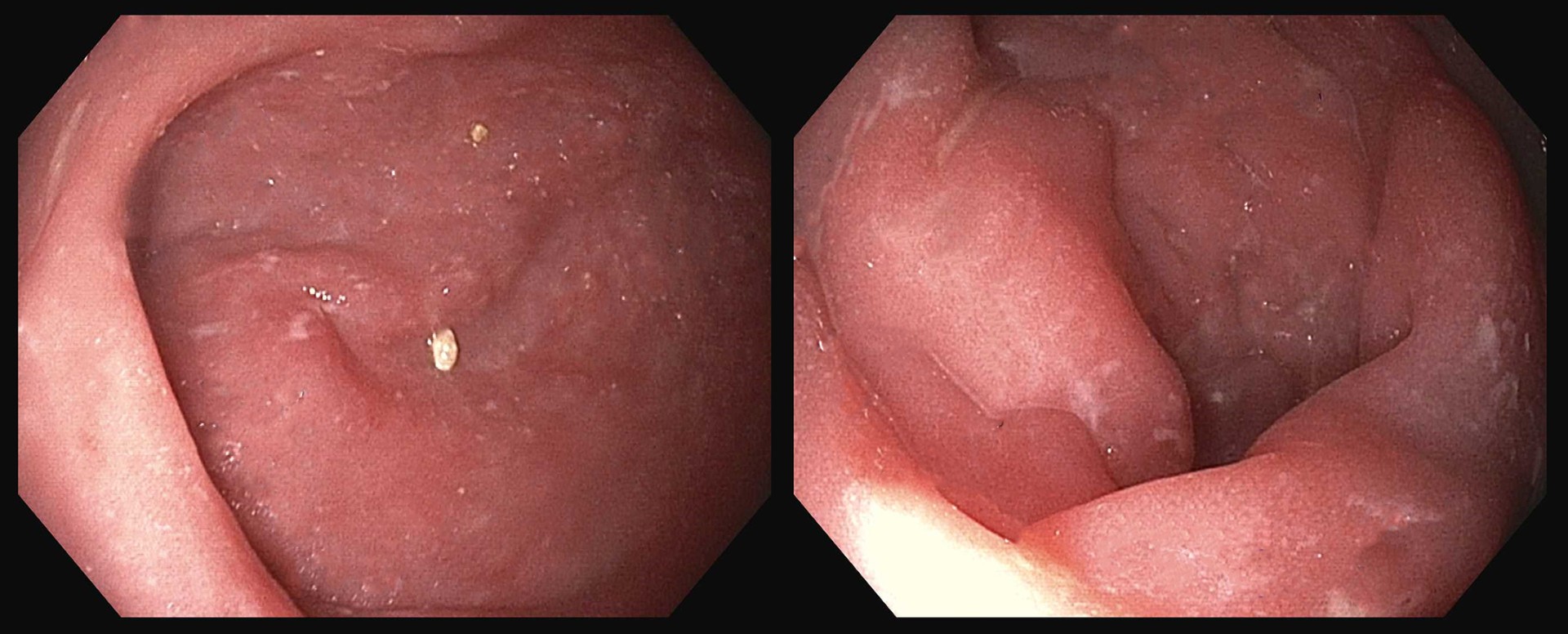
Figure: CVID colitis on colonoscopy
Disclosures:
Sophia Pimpinelli indicated no relevant financial relationships.
Mansi Sheth indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Sophia Pimpinelli, MD1, Mansi Sheth, DO2, Anish V. Patel, MD1. P2550 - CVID-Associated Colitis Presenting as Chronic Diarrhea and Mimicking IBD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
