Monday Poster Session
Category: Colon
P2535 - Blinded by Distension: A Large Mesenteric Abscess Masquerading as Sigmoid Volvulus

Shefali Mody, MBBS (she/her/hers)
SUNY Upstate Medical University Hospital
Syracuse, NY
Presenting Author(s)
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2SUNY Upstate Medical University, Syracuse, NY
Introduction:
Accurate differentiation between similarly presenting abdominal pathologies such as sigmoid volvulus, intra-abdominal abscess, and other abdominal masses is critical, as misdiagnosis can delay definitive management and increase morbidity. We present the case of a large mesenteric abscess initially misdiagnosed as sigmoid volvulus, highlighting the diagnostic challenges in differentiating sigmoid volvulus from other causes of large bowel obstruction, especially when clinical and radiologic features overlap.
Case Description/
Methods:
A 69-year-old man presented with chronic, progressively worsening abdominal pain, distension, fatigue, recent 70-lb weight loss, and nausea for months. He had no history of constipation or obstipation. Abdominal examination revealed distension and diffuse tenderness without peritoneal signs. Initial CT abdomen/pelvis with contrast showed a markedly dilated sigmoid colon (8.8 cm) consistent with sigmoid volvulus. GI was consulted and colonoscopic decompression with rectal tube placement to distal transverse colon was performed. Post-procedure exam showed minimal improvement. Three days later, due to persistent symptoms, repeat CT was done. Despite the rectal tube reaching the transverse colon, there was no change in size of the presumed “sigmoid colon". It was then reinterpreted as a large extraluminal mesenteric abscess, likely from an intra-mesenteric perforation with abscess formation. IR-guided percutaneous drainage was performed, retrieving purulent fluid. Repeat CT confirmed near-resolution of the abscess. The patient continues outpatient surgical follow-up with plans for CT abdomen/pelvis with rectal contrast to locate the colonic perforation. If persistent extravasation is found, surgical resection will be required.
Discussion:
The ASGE recommends endoscopic decompression as first-line therapy in stable patients with presumed sigmoid volvulus but stresses reassessment when clinical improvement is lacking or atypical features arise. Absence of proportionate colonic dilation on endoscopy should prompt reassessment. In patients lacking classic risk factors like constipation, especially with chronic symptoms and weight loss, alternative or coexisting diagnoses should be considered. This case highlights the importance of a broad differential diagnosis, careful imaging interpretation, and multidisciplinary management in atypical presentations. Misinterpretation or cognitive bias may lead to inappropriate interventions or delayed recognition of alternate pathologies.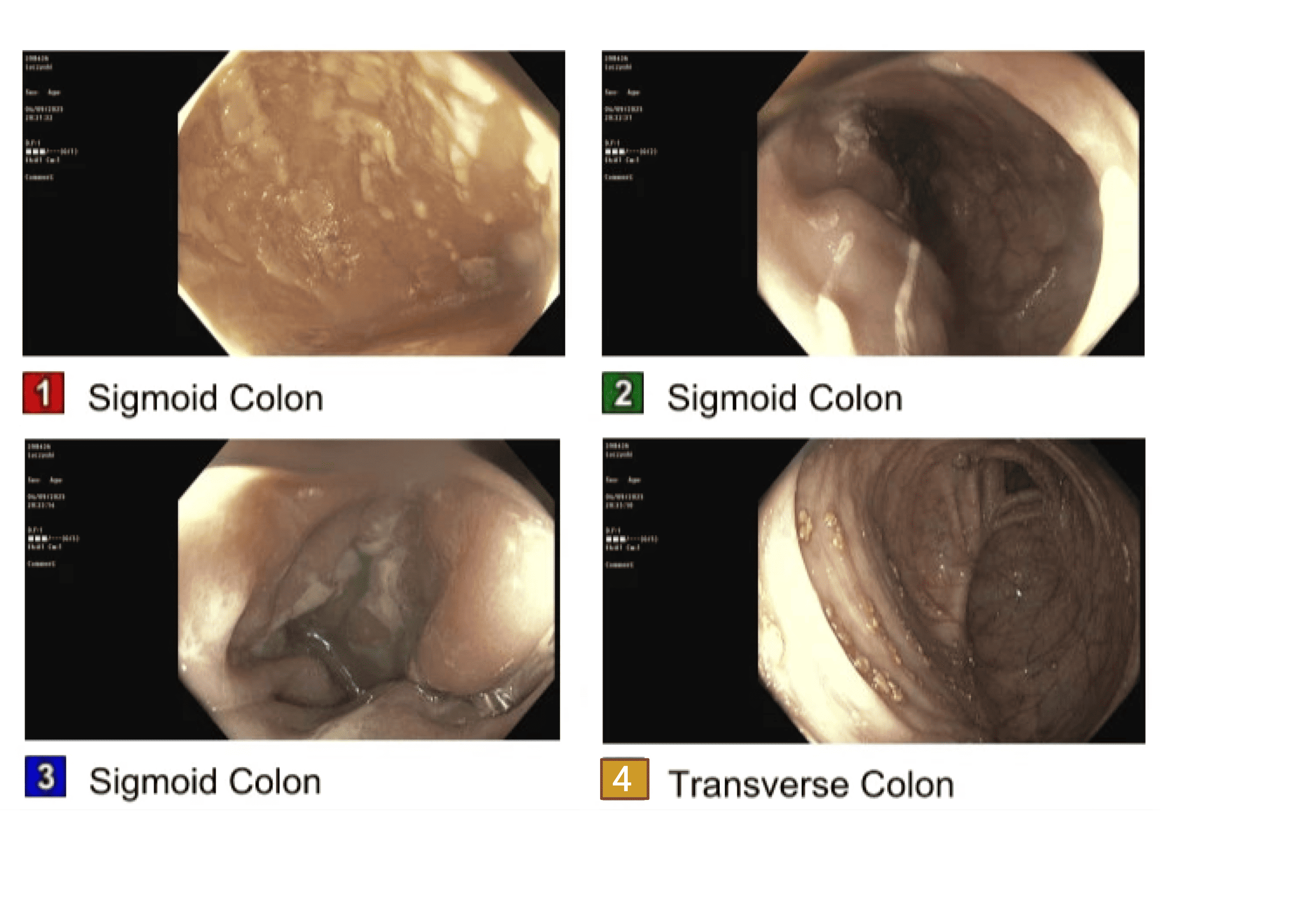
Figure: CT Abdomen/Pelvis (coronal and axial sections) scans showing suspected sigmoid volvulus with large air-fluid level before (left) and after (right) rectal tube insertion (red arrow) showing persistently dilated suspected sigmoid volvulus after rectal tube insertion.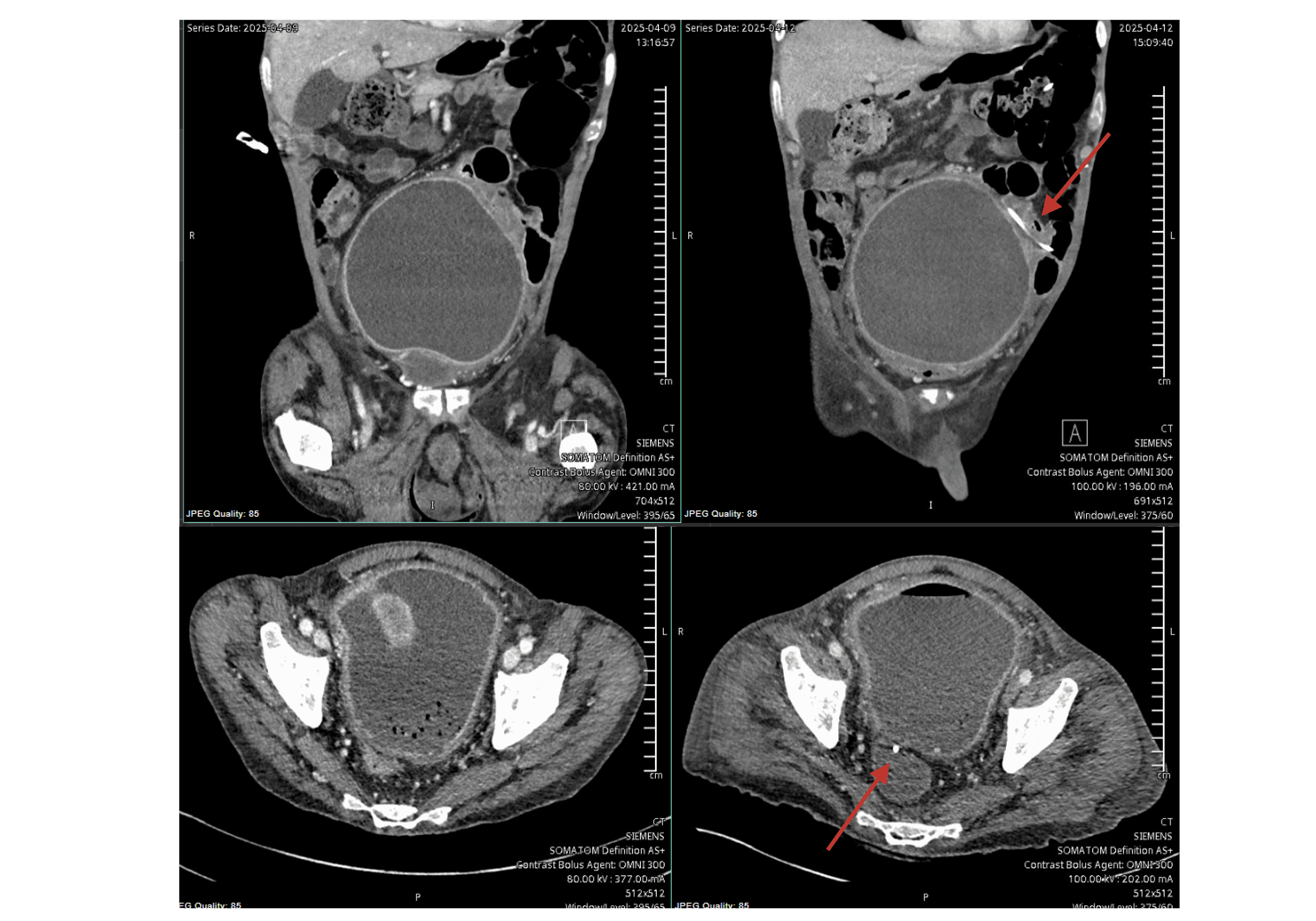
Figure: Endoscopic images showing absence of distension of sigmoid colon during attempted colonoscopic decompression of suspected sigmoid volvulus
Disclosures:
Shefali Mody indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Dayana Nasr indicated no relevant financial relationships.
Karan Sachdeva indicated no relevant financial relationships.
Bishnu Sapkota indicated no relevant financial relationships.
Shefali Mody, MBBS1, Avleen Kaur, MD2, Dayana Nasr, MD1, Karan Sachdeva, MBBS, MPH1, Bishnu Sapkota, MD, FACG2. P2535 - Blinded by Distension: A Large Mesenteric Abscess Masquerading as Sigmoid Volvulus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
