Monday Poster Session
Category: Colorectal Cancer Prevention
P2614 - Implementation of a CRC Screening Protocol Among Incarcerated Adults: A Quality Improvement Initiative
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Naveena Luke, MD (she/her/hers)
NYU Grossman School of Medicine
Brooklyn, NY
Presenting Author(s)
Naveena Luke, MD1, Ashley Augustin, BA2, Firrah Saeed, MD2, Zachary Rosner, MD3, Renee Williams, MD, MHPE, FACG2
1NYU Grossman School of Medicine, Brooklyn, NY; 2NYU Grossman School of Medicine, New York, NY; 3NYU Langone Health, New York, NY
Introduction: Colorectal cancer (CRC) remains the second leading cause of cancer-related death in the U.S., yet screening rates among incarcerated populations are disproportionately low. Prior studies estimate that only about 30% of age-eligible inmates are up to date with CRC screening [1-2]. Given the logistical, financial, and structural barriers to colonoscopy in correctional settings, fecal immunochemical testing (FIT) represents a viable low-cost alternative. This study aimed to implement a risk-based screening protocol at a Prison Health Services (PHS) facility.
Methods: We designed a single-center, non-randomized, mixed-methods study using retrospective and prospective data collection to assess the impact of implementing a validated risk assessment and FIT protocol on PHS CRC screening rates.
Patients aged 45 - 75 years were identified and given a screening eligibility questionnaire by the primary care provider. High risk patients are offered colonoscopy, and average risk patients are offered FIT testing. Pre-intervention screening rates will be calculated using a retrospective chart review. Patients with a positive FIT are scheduled for follow-up colonoscopy within 60 days; one patient with positive FIT was released prior to colonoscopy. Demographics, screening outcomes, and follow-up rates are tracked and compared before and after implementation. Key metrics include baseline CRC screening rate, proportion of eligible patients receiving FIT post-implementation, proportion of patients with positive FIT results, and completion rate of diagnostic colonoscopy following positive FIT.
Results: Of the patients screened in the PHS clinic, 63% reported never having been screened for CRC. Only 37% endorsed prior screening. Additionally, 26% reported a family history of CRC or polyps, and 37% reported symptoms concerning for CRC, including rectal bleeding, altered bowel habits, or unexplained weight loss. Awareness of hereditary cancer syndromes and inflammatory bowel disease was limited, with many selecting “I don’t know” when queried about these conditions. These findings support the utility of a structured, tiered screening protocol in correctional settings to appropriately allocate FIT and colonoscopy resources.
Discussion: A risk-based CRC screening approach incorporating FIT is feasible and may improve screening uptake in correctional facilities. Early data highlight the potential for this strategy to reduce disparities and support stronger linkages between prisons and public health systems.
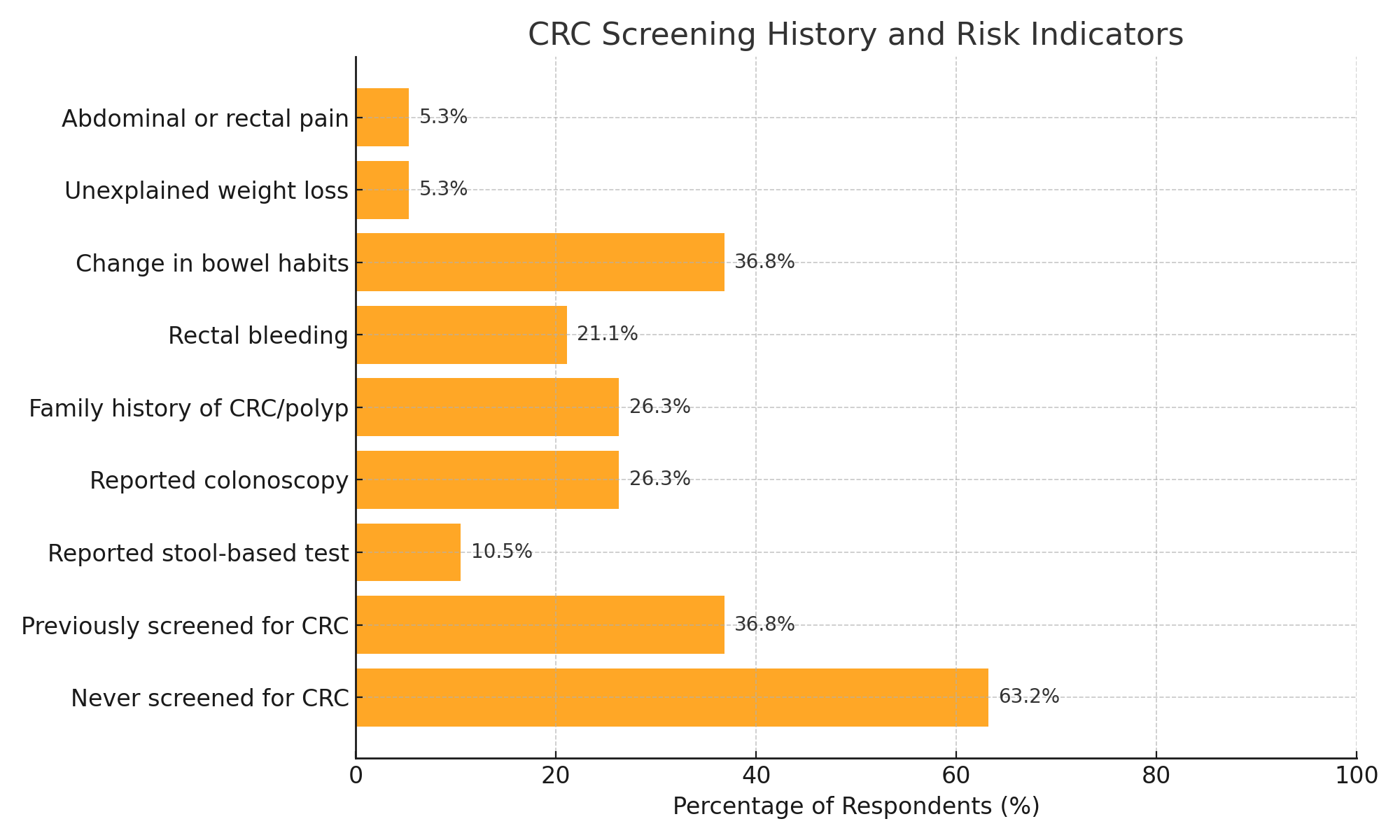
Figure: Figure: Preliminary responses from 19 incarcerated individuals highlight gaps in colorectal cancer (CRC) screening and key risk factors. While 63% reported never having been screened, 26% reported a family history of CRC or polyps, and over one-third endorsed symptoms such as rectal bleeding or bowel habit changes.
Disclosures:
Naveena Luke indicated no relevant financial relationships.
Ashley Augustin indicated no relevant financial relationships.
Firrah Saeed indicated no relevant financial relationships.
Zachary Rosner indicated no relevant financial relationships.
Renee Williams indicated no relevant financial relationships.
Naveena Luke, MD1, Ashley Augustin, BA2, Firrah Saeed, MD2, Zachary Rosner, MD3, Renee Williams, MD, MHPE, FACG2. P2614 - Implementation of a CRC Screening Protocol Among Incarcerated Adults: A Quality Improvement Initiative, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYU Grossman School of Medicine, Brooklyn, NY; 2NYU Grossman School of Medicine, New York, NY; 3NYU Langone Health, New York, NY
Introduction: Colorectal cancer (CRC) remains the second leading cause of cancer-related death in the U.S., yet screening rates among incarcerated populations are disproportionately low. Prior studies estimate that only about 30% of age-eligible inmates are up to date with CRC screening [1-2]. Given the logistical, financial, and structural barriers to colonoscopy in correctional settings, fecal immunochemical testing (FIT) represents a viable low-cost alternative. This study aimed to implement a risk-based screening protocol at a Prison Health Services (PHS) facility.
Methods: We designed a single-center, non-randomized, mixed-methods study using retrospective and prospective data collection to assess the impact of implementing a validated risk assessment and FIT protocol on PHS CRC screening rates.
Patients aged 45 - 75 years were identified and given a screening eligibility questionnaire by the primary care provider. High risk patients are offered colonoscopy, and average risk patients are offered FIT testing. Pre-intervention screening rates will be calculated using a retrospective chart review. Patients with a positive FIT are scheduled for follow-up colonoscopy within 60 days; one patient with positive FIT was released prior to colonoscopy. Demographics, screening outcomes, and follow-up rates are tracked and compared before and after implementation. Key metrics include baseline CRC screening rate, proportion of eligible patients receiving FIT post-implementation, proportion of patients with positive FIT results, and completion rate of diagnostic colonoscopy following positive FIT.
Results: Of the patients screened in the PHS clinic, 63% reported never having been screened for CRC. Only 37% endorsed prior screening. Additionally, 26% reported a family history of CRC or polyps, and 37% reported symptoms concerning for CRC, including rectal bleeding, altered bowel habits, or unexplained weight loss. Awareness of hereditary cancer syndromes and inflammatory bowel disease was limited, with many selecting “I don’t know” when queried about these conditions. These findings support the utility of a structured, tiered screening protocol in correctional settings to appropriately allocate FIT and colonoscopy resources.
Discussion: A risk-based CRC screening approach incorporating FIT is feasible and may improve screening uptake in correctional facilities. Early data highlight the potential for this strategy to reduce disparities and support stronger linkages between prisons and public health systems.
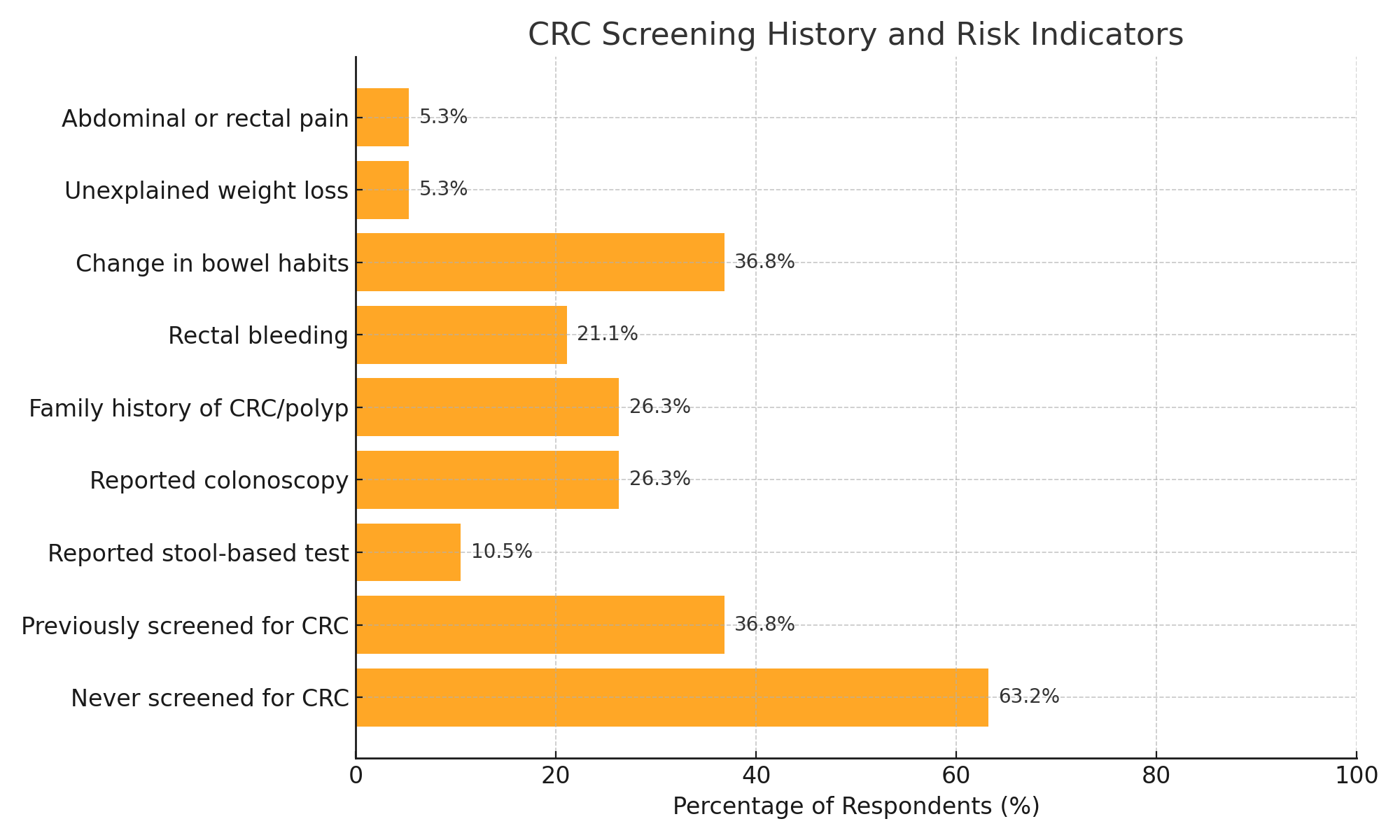
Figure: Figure: Preliminary responses from 19 incarcerated individuals highlight gaps in colorectal cancer (CRC) screening and key risk factors. While 63% reported never having been screened, 26% reported a family history of CRC or polyps, and over one-third endorsed symptoms such as rectal bleeding or bowel habit changes.
Disclosures:
Naveena Luke indicated no relevant financial relationships.
Ashley Augustin indicated no relevant financial relationships.
Firrah Saeed indicated no relevant financial relationships.
Zachary Rosner indicated no relevant financial relationships.
Renee Williams indicated no relevant financial relationships.
Naveena Luke, MD1, Ashley Augustin, BA2, Firrah Saeed, MD2, Zachary Rosner, MD3, Renee Williams, MD, MHPE, FACG2. P2614 - Implementation of a CRC Screening Protocol Among Incarcerated Adults: A Quality Improvement Initiative, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
