Monday Poster Session
Category: Colorectal Cancer Prevention
P2607 - A Clinical Assessment: Counseling Families on Timing of Colorectal Cancer Screening
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Bertilia Tavarez, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Bertilia Tavarez, MD1, Hamzah Shariff, MD1, Breanne McDermott, BS2, Limi Jamma, MD1, Sonali Shah, MD1, Sanjna Shelukar, MD1, Akash Patel, DO1, Christopher Henry, MD1, Aaron Martin, MD1
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Colorectal cancer (CRC) is the second leading cause of cancer death in the US. CRC screening should start with a colonoscopy at age 40 or 10 years before youngest affected relative, whichever is earlier, for patients with CRC or advanced polyp (AP) in 1 first degree relative (FDR) at age < 60 years or CRC/AP in more than 2 FDR at any age. Limited data exists regarding clinical application of this guideline despite its utility in supporting early CRC screening in patients at higher risk. In this study, we aim to assess the level of integration of FDR counseling for CRC screening in patients diagnosed with CRC.
Methods: We conducted a retrospective chart review of electronic health records from an urban academic institution. Patients diagnosed with CRC or an AP from 1/01/2019 to 12/31/2024 were identified. CRC was defined as any colorectal adenocarcinoma and an AP was defined as an adenoma >10mm, any adenoma with a villous component or high-grade dysplasia, and serrated lesions >10mm. Patient demographics and disease characteristics were collected with special attention to CRC risk factors. The primary endpoint was documentation of informing FDR about early screening in patients with CRC or an AP.
Results: We identified 225 patients; 51.1% had an average age range of 50-69 yrs. Three patients had inflammatory bowel disease, 3 had Lynch Syndrome and 1 had Familial Adenomatous Polyposis. 50% had hypertension and 21% had diabetes mellitus; 3.5% had a history of prior pelvic radiation. Only 13 patients had documented counseling informing FDR when to undergo colonoscopy. Of these 13 patients, 8 were counseled by a genetics counselor, 2 by a colorectal surgeon, 2 by an oncologist, and 1 by a gastroenterologist (Figure 1). However, there was no documentation of whether FDR actually underwent early CRC screening.
Discussion: This study reveals that informing FDR of patients with CRC or an AP is rarely documented. Less than 6% of patients were advised of this practice, and of those, the majority were done by a genetic counselor; only 7% by gastroenterologists. There was also no documentation as to whether or not FDR actually underwent CRC screening at the recommended age per ACG guidelines. This study suggests limited counseling of FDR screening by gastroenterologists after CRC diagnosis. Further studies dedicated to increasing FDR screening should be pursued to increase early detection of CRC in this high-risk population.
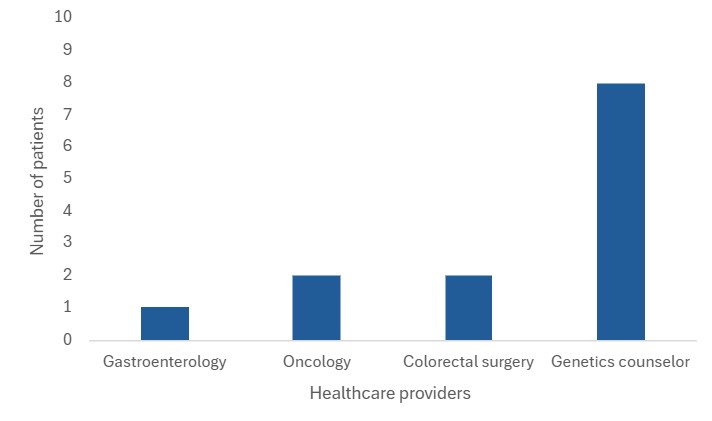
Figure: Figure 1. Number of healthcare providers documenting counseling patients when FDR should undergo CRC screening.
Disclosures:
Bertilia Tavarez indicated no relevant financial relationships.
Hamzah Shariff indicated no relevant financial relationships.
Breanne McDermott indicated no relevant financial relationships.
Limi Jamma indicated no relevant financial relationships.
Sonali Shah indicated no relevant financial relationships.
Sanjna Shelukar indicated no relevant financial relationships.
Akash Patel indicated no relevant financial relationships.
Christopher Henry indicated no relevant financial relationships.
Aaron Martin indicated no relevant financial relationships.
Bertilia Tavarez, MD1, Hamzah Shariff, MD1, Breanne McDermott, BS2, Limi Jamma, MD1, Sonali Shah, MD1, Sanjna Shelukar, MD1, Akash Patel, DO1, Christopher Henry, MD1, Aaron Martin, MD1. P2607 - A Clinical
Assessment: Counseling Families on Timing of Colorectal Cancer Screening, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Colorectal cancer (CRC) is the second leading cause of cancer death in the US. CRC screening should start with a colonoscopy at age 40 or 10 years before youngest affected relative, whichever is earlier, for patients with CRC or advanced polyp (AP) in 1 first degree relative (FDR) at age < 60 years or CRC/AP in more than 2 FDR at any age. Limited data exists regarding clinical application of this guideline despite its utility in supporting early CRC screening in patients at higher risk. In this study, we aim to assess the level of integration of FDR counseling for CRC screening in patients diagnosed with CRC.
Methods: We conducted a retrospective chart review of electronic health records from an urban academic institution. Patients diagnosed with CRC or an AP from 1/01/2019 to 12/31/2024 were identified. CRC was defined as any colorectal adenocarcinoma and an AP was defined as an adenoma >10mm, any adenoma with a villous component or high-grade dysplasia, and serrated lesions >10mm. Patient demographics and disease characteristics were collected with special attention to CRC risk factors. The primary endpoint was documentation of informing FDR about early screening in patients with CRC or an AP.
Results: We identified 225 patients; 51.1% had an average age range of 50-69 yrs. Three patients had inflammatory bowel disease, 3 had Lynch Syndrome and 1 had Familial Adenomatous Polyposis. 50% had hypertension and 21% had diabetes mellitus; 3.5% had a history of prior pelvic radiation. Only 13 patients had documented counseling informing FDR when to undergo colonoscopy. Of these 13 patients, 8 were counseled by a genetics counselor, 2 by a colorectal surgeon, 2 by an oncologist, and 1 by a gastroenterologist (Figure 1). However, there was no documentation of whether FDR actually underwent early CRC screening.
Discussion: This study reveals that informing FDR of patients with CRC or an AP is rarely documented. Less than 6% of patients were advised of this practice, and of those, the majority were done by a genetic counselor; only 7% by gastroenterologists. There was also no documentation as to whether or not FDR actually underwent CRC screening at the recommended age per ACG guidelines. This study suggests limited counseling of FDR screening by gastroenterologists after CRC diagnosis. Further studies dedicated to increasing FDR screening should be pursued to increase early detection of CRC in this high-risk population.
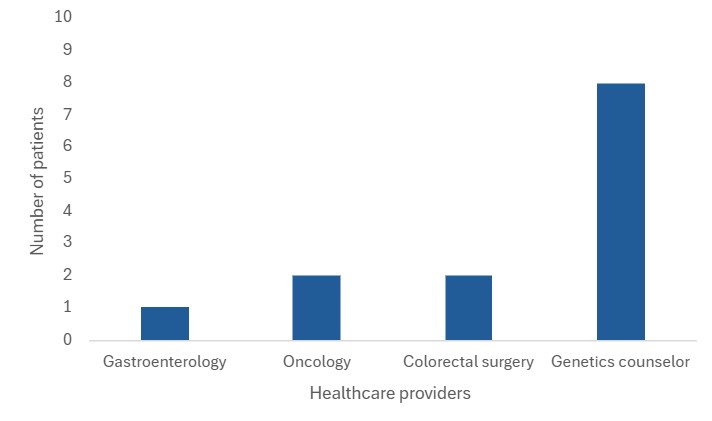
Figure: Figure 1. Number of healthcare providers documenting counseling patients when FDR should undergo CRC screening.
Disclosures:
Bertilia Tavarez indicated no relevant financial relationships.
Hamzah Shariff indicated no relevant financial relationships.
Breanne McDermott indicated no relevant financial relationships.
Limi Jamma indicated no relevant financial relationships.
Sonali Shah indicated no relevant financial relationships.
Sanjna Shelukar indicated no relevant financial relationships.
Akash Patel indicated no relevant financial relationships.
Christopher Henry indicated no relevant financial relationships.
Aaron Martin indicated no relevant financial relationships.
Bertilia Tavarez, MD1, Hamzah Shariff, MD1, Breanne McDermott, BS2, Limi Jamma, MD1, Sonali Shah, MD1, Sanjna Shelukar, MD1, Akash Patel, DO1, Christopher Henry, MD1, Aaron Martin, MD1. P2607 - A Clinical
Assessment: Counseling Families on Timing of Colorectal Cancer Screening, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
