Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2719 - Not Just a Weight Issue: The Hidden Threat of Superior Mesenteric Artery Syndrome With a Normal BMI
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Woo Suk Kim, DO (he/him/his)
Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai
Queens, NY
Presenting Author(s)
Woo Suk Kim, DO, Bibhuti Adhikari, MD, Sindhura Kolli, MD, Tasur Seen, MD, Genanew Bedanie, MD, Nirali Sheth, DO, Anastasia Novikov, MD
Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, Queens, NY
Introduction: Superior Mesenteric Artery (SMA) Syndrome is a potentially life-threatening condition caused by external compression of the third portion of the duodenum between the aorta and the SMA. Normally, an aortomesenteric angle of 40-65 degrees is maintained by a fat pad. When the angle narrows to < 25 degrees, the resulting duodenal compression between the two vessels produces abdominal pain, distention, early satiety, and bilious vomiting. SMA Syndrome is typically associated with a Body Mass Index (BMI) < 17, with elevated risk in intravenous drug use (IVDU), eating disorders, malignancy, and post-surgical weight loss. Treatment is often delayed due to the nonspecific symptoms, as SMA Syndrome is infrequently considered early in the differential diagnoses. To emphasize the need for early consideration of SMA Syndrome in high-risk populations, we present a case of SMA Syndrome with atypical symptoms in the context of IVDU.
Case Description/
Methods: A 28-year-old female with a history of IV heroin and fentanyl use presented with recurrent bilious vomiting. She had no abdominal pain or distention. Despite initial fluid resuscitation, the patient had persistent bilious vomiting and intolerance to oral intake. A Computed Tomography (CT) imaging revealed a severely distended stomach. An Esophagogastroduodenoscopy found the proximal duodenum to be dilated, with an acute stenosis in the third portion of the duodenum that appeared as a slit-like structure with a pulsatile duodenal wall, suggestive of external compression. The CT imaging was reassessed to confirm that the aortomesenteric angle was < 25 degrees, diagnostic of SMA Syndrome in addition to the endoscopic findings. Supportive measures were initiated with nasogastric decompression and nutritional supplementation, with subsequent resolution in her symptoms and advancement of her diet.
Discussion: While SMA Syndrome is classically associated with a BMI < 17, our patient with a normal BMI of 20 developed the condition due to a significant reduction in body fat percentage rather than total body weight. Her history of IVDU contributed to her atypical presentation limited to bilious vomiting without abdominal pain. The nonspecific nature of SMA Syndrome often delays diagnosis, as symptoms overlap with more common gastrointestinal conditions. This case suggests that BMI may underestimate risk in special populations, highlighting the role of body composition and clinical risk factors as additional markers in the diagnosis of SMA Syndrome.
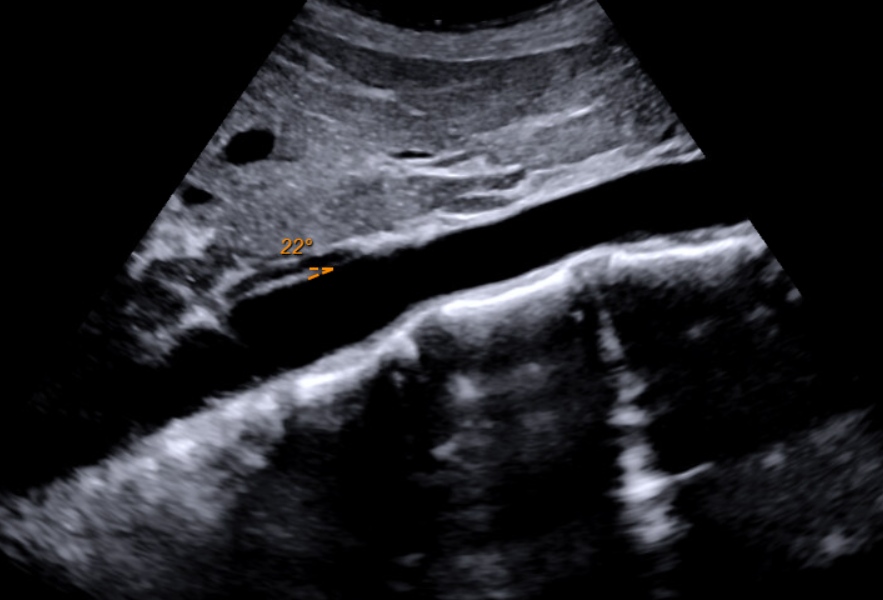
Figure: CT showing SMA branching off aorta and compressing duodenum

Figure: Aortic ultrasound showing narrow aortomesenteric angle due to loss of fat pad
Disclosures:
Woo Suk Kim indicated no relevant financial relationships.
Bibhuti Adhikari indicated no relevant financial relationships.
Sindhura Kolli indicated no relevant financial relationships.
Tasur Seen indicated no relevant financial relationships.
Genanew Bedanie indicated no relevant financial relationships.
Nirali Sheth indicated no relevant financial relationships.
Anastasia Novikov indicated no relevant financial relationships.
Woo Suk Kim, DO, Bibhuti Adhikari, MD, Sindhura Kolli, MD, Tasur Seen, MD, Genanew Bedanie, MD, Nirali Sheth, DO, Anastasia Novikov, MD. P2719 - Not Just a Weight Issue: The Hidden Threat of Superior Mesenteric Artery Syndrome With a Normal BMI, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, Queens, NY
Introduction: Superior Mesenteric Artery (SMA) Syndrome is a potentially life-threatening condition caused by external compression of the third portion of the duodenum between the aorta and the SMA. Normally, an aortomesenteric angle of 40-65 degrees is maintained by a fat pad. When the angle narrows to < 25 degrees, the resulting duodenal compression between the two vessels produces abdominal pain, distention, early satiety, and bilious vomiting. SMA Syndrome is typically associated with a Body Mass Index (BMI) < 17, with elevated risk in intravenous drug use (IVDU), eating disorders, malignancy, and post-surgical weight loss. Treatment is often delayed due to the nonspecific symptoms, as SMA Syndrome is infrequently considered early in the differential diagnoses. To emphasize the need for early consideration of SMA Syndrome in high-risk populations, we present a case of SMA Syndrome with atypical symptoms in the context of IVDU.
Case Description/
Methods: A 28-year-old female with a history of IV heroin and fentanyl use presented with recurrent bilious vomiting. She had no abdominal pain or distention. Despite initial fluid resuscitation, the patient had persistent bilious vomiting and intolerance to oral intake. A Computed Tomography (CT) imaging revealed a severely distended stomach. An Esophagogastroduodenoscopy found the proximal duodenum to be dilated, with an acute stenosis in the third portion of the duodenum that appeared as a slit-like structure with a pulsatile duodenal wall, suggestive of external compression. The CT imaging was reassessed to confirm that the aortomesenteric angle was < 25 degrees, diagnostic of SMA Syndrome in addition to the endoscopic findings. Supportive measures were initiated with nasogastric decompression and nutritional supplementation, with subsequent resolution in her symptoms and advancement of her diet.
Discussion: While SMA Syndrome is classically associated with a BMI < 17, our patient with a normal BMI of 20 developed the condition due to a significant reduction in body fat percentage rather than total body weight. Her history of IVDU contributed to her atypical presentation limited to bilious vomiting without abdominal pain. The nonspecific nature of SMA Syndrome often delays diagnosis, as symptoms overlap with more common gastrointestinal conditions. This case suggests that BMI may underestimate risk in special populations, highlighting the role of body composition and clinical risk factors as additional markers in the diagnosis of SMA Syndrome.
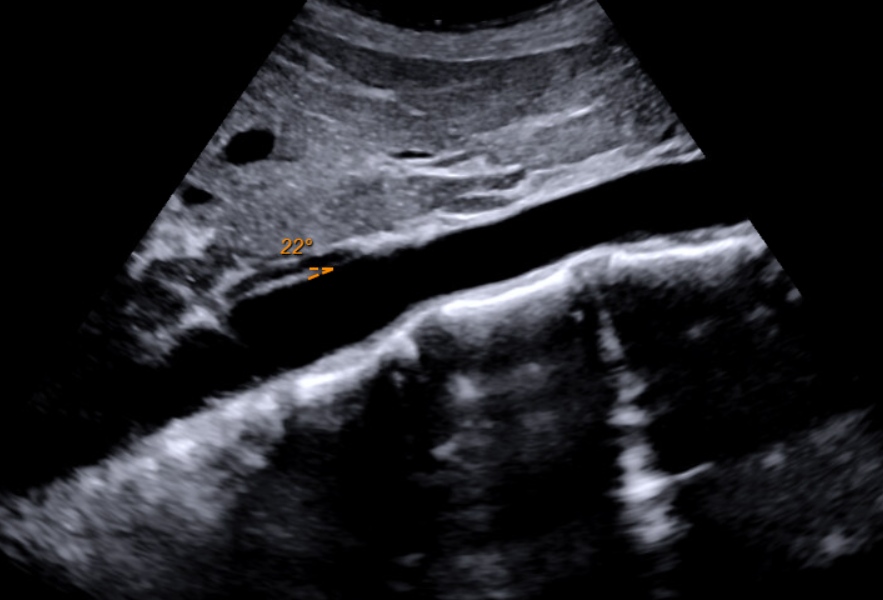
Figure: CT showing SMA branching off aorta and compressing duodenum

Figure: Aortic ultrasound showing narrow aortomesenteric angle due to loss of fat pad
Disclosures:
Woo Suk Kim indicated no relevant financial relationships.
Bibhuti Adhikari indicated no relevant financial relationships.
Sindhura Kolli indicated no relevant financial relationships.
Tasur Seen indicated no relevant financial relationships.
Genanew Bedanie indicated no relevant financial relationships.
Nirali Sheth indicated no relevant financial relationships.
Anastasia Novikov indicated no relevant financial relationships.
Woo Suk Kim, DO, Bibhuti Adhikari, MD, Sindhura Kolli, MD, Tasur Seen, MD, Genanew Bedanie, MD, Nirali Sheth, DO, Anastasia Novikov, MD. P2719 - Not Just a Weight Issue: The Hidden Threat of Superior Mesenteric Artery Syndrome With a Normal BMI, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
