Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2711 - Efficacy and Safety of Enhanced Endoscopic Sleeve Gastroplasty With Argon Plasma Coagulation vs Endoscopic Sleeve Gastroplasty Alone: A Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alan Gabriel Ortega Macias, MD (he/him/his)
University of New Mexico
Albuquerque, NM
Presenting Author(s)
Alan Gabriel. Ortega Macias, MD1, Udita Gupta, MD2, Pooja Viswanath, DO1, Gicel Jacklin. Aguilar, DO3, Adham Obeidat, MD4, Gulshan Parasher, MD, FACG1, Abu Baker Sheikh, MD2
1University of New Mexico, Albuquerque, NM; 2University of New Mexico Health Sciences Center, Albuquerque, NM; 3University of New Mexico Hospital, Albuquerque, NM; 4Presbyterian Health care, Albuquerque, NM
Introduction: Endoscopic Sleeve Gastroplasty (ESG), is a novel technique that reduces the gastric size reservoir using a full-thickness endoscopic suturing device. Its impact on weight loss has been significantly higher than lifestyle changes alone. There is a direct correlation between the integrity of the ESG and the achieved percentage of total body weight loss (%TBWL). Although, argon plasma coagulation (APC) is primarily used for the management of hemostasis by applying non-contact mucosal thermal ablation; its application before ESG could enhance wound healing and subsequent fibrosis, reducing suture dehiscence.
Methods: Following the PRISMA guidelines, a systematic review and meta-analysis were performed to determine the impact of APC prior to ESG for weight loss. Primary outcomes were %TBWL at 6 and 12 months. Gray literature was included due to technique novelty. Data was analyzed using R version 4.2.2. The risk of bias was assessed by the Rob-2 and Robins-I tool. The quality of evidence was graded using the GRADE and Newcastle-Ottawa guidelines.
Results: Two observational and one randomized clinical trial described the total weight loss at 6 and 12 months of ESG + APC vs ESG, totaling 231 patients. Meta-analysis test for overall effect showed no statistically significant difference between groups (SMD = 0.70; 95% CI = [-0.90; 2.30]; p = 0.20; Fig. 1, and SMD = 0.77; 95% CI = [-0.57; 2.11]; p = 0.13; Fig. 2, respectively). Similarly, there was no statistically significant difference in terms of rate of adverse events between groups (RR = 0.39; 95% CI = [0.13; 1.16]; p = 0.07; Fig. 3). The risk of bias was moderate with moderate quality of evidence amongst the included studies.
Discussion: Our updated systematic review and meta-analysis demonstrated an absence of statistically significant difference in %TBWL loss at 6 to 12 months between ESG+APC compared to ESG alone. Further randomized studies are needed to confirm these findings.
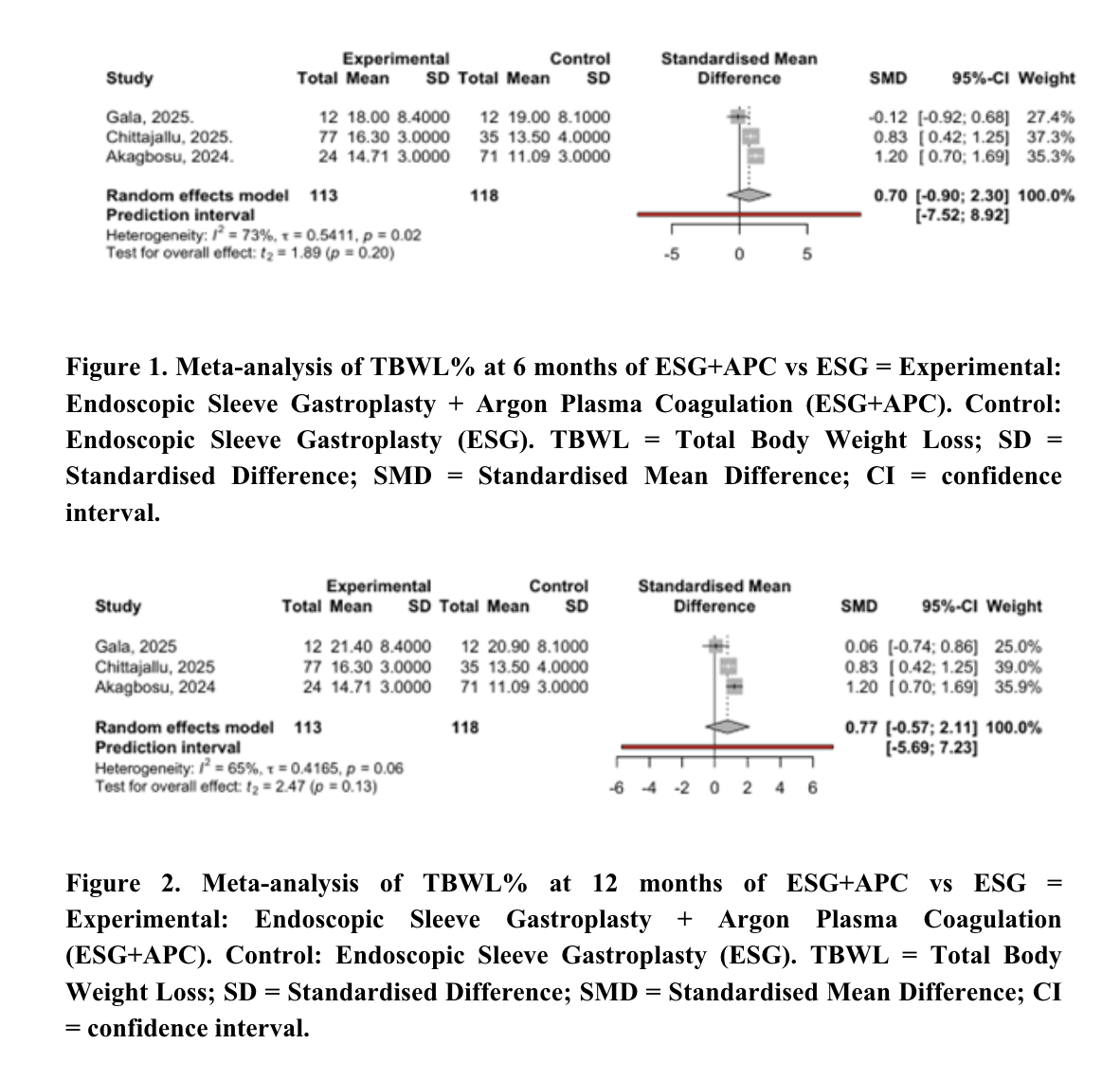
Figure: Figure 1 & 2. Meta-analysis of TBWL% at 6 -12 months of ESG+APC vs ESG = Experimental: Endoscopic Sleeve Gastroplasty + Argon Plasma Coagulation (ESG+APC). Control: Endoscopic Sleeve Gastroplasty (ESG). TBWL = Total Body Weight Loss; SD = Standardised Difference; SMD = Standardised Mean Difference; CI = confidence interval.
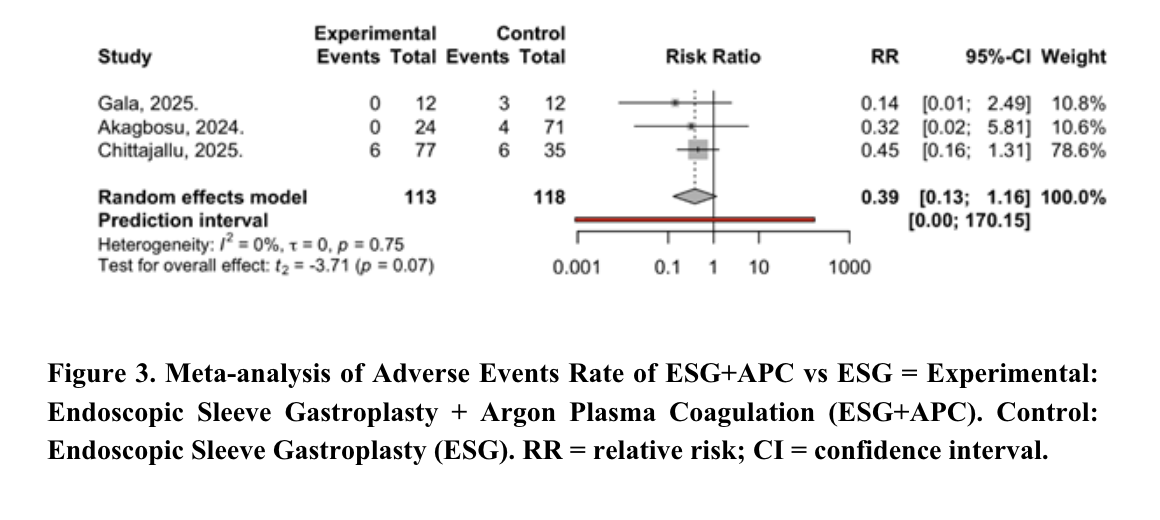
Figure: Figure 3. Meta-analysis of Adverse Events Rate of ESG+APC vs ESG = Experimental: Endoscopic Sleeve Gastroplasty + Argon Plasma Coagulation (ESG+APC). Control: Endoscopic Sleeve Gastroplasty (ESG). RR = relative risk; CI = confidence interval.
Disclosures:
Alan Ortega Macias indicated no relevant financial relationships.
Udita Gupta indicated no relevant financial relationships.
Pooja Viswanath indicated no relevant financial relationships.
Gicel Aguilar indicated no relevant financial relationships.
Adham Obeidat indicated no relevant financial relationships.
Gulshan Parasher indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Alan Gabriel. Ortega Macias, MD1, Udita Gupta, MD2, Pooja Viswanath, DO1, Gicel Jacklin. Aguilar, DO3, Adham Obeidat, MD4, Gulshan Parasher, MD, FACG1, Abu Baker Sheikh, MD2. P2711 - Efficacy and Safety of Enhanced Endoscopic Sleeve Gastroplasty With Argon Plasma Coagulation vs Endoscopic Sleeve Gastroplasty Alone: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico, Albuquerque, NM; 2University of New Mexico Health Sciences Center, Albuquerque, NM; 3University of New Mexico Hospital, Albuquerque, NM; 4Presbyterian Health care, Albuquerque, NM
Introduction: Endoscopic Sleeve Gastroplasty (ESG), is a novel technique that reduces the gastric size reservoir using a full-thickness endoscopic suturing device. Its impact on weight loss has been significantly higher than lifestyle changes alone. There is a direct correlation between the integrity of the ESG and the achieved percentage of total body weight loss (%TBWL). Although, argon plasma coagulation (APC) is primarily used for the management of hemostasis by applying non-contact mucosal thermal ablation; its application before ESG could enhance wound healing and subsequent fibrosis, reducing suture dehiscence.
Methods: Following the PRISMA guidelines, a systematic review and meta-analysis were performed to determine the impact of APC prior to ESG for weight loss. Primary outcomes were %TBWL at 6 and 12 months. Gray literature was included due to technique novelty. Data was analyzed using R version 4.2.2. The risk of bias was assessed by the Rob-2 and Robins-I tool. The quality of evidence was graded using the GRADE and Newcastle-Ottawa guidelines.
Results: Two observational and one randomized clinical trial described the total weight loss at 6 and 12 months of ESG + APC vs ESG, totaling 231 patients. Meta-analysis test for overall effect showed no statistically significant difference between groups (SMD = 0.70; 95% CI = [-0.90; 2.30]; p = 0.20; Fig. 1, and SMD = 0.77; 95% CI = [-0.57; 2.11]; p = 0.13; Fig. 2, respectively). Similarly, there was no statistically significant difference in terms of rate of adverse events between groups (RR = 0.39; 95% CI = [0.13; 1.16]; p = 0.07; Fig. 3). The risk of bias was moderate with moderate quality of evidence amongst the included studies.
Discussion: Our updated systematic review and meta-analysis demonstrated an absence of statistically significant difference in %TBWL loss at 6 to 12 months between ESG+APC compared to ESG alone. Further randomized studies are needed to confirm these findings.
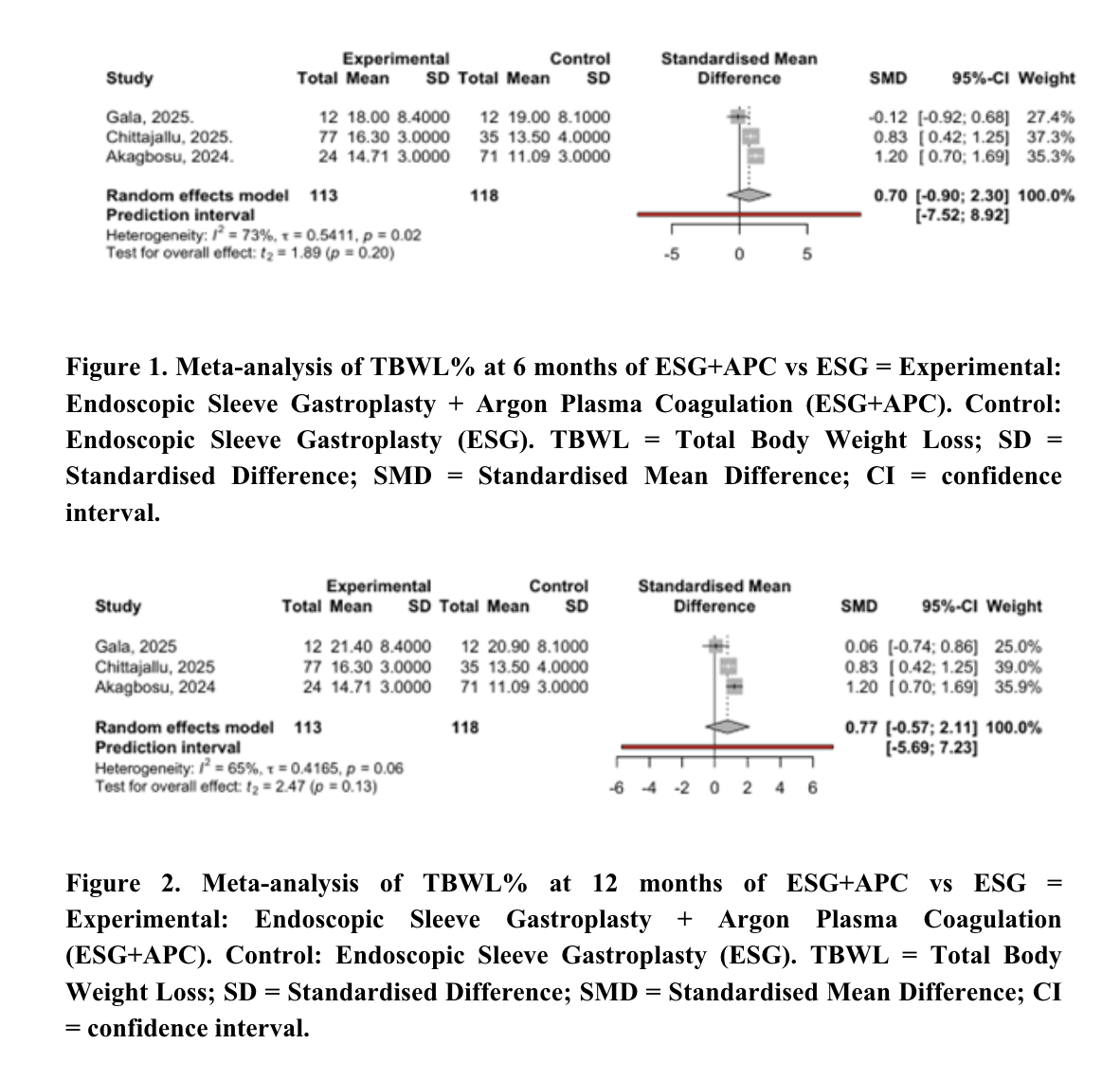
Figure: Figure 1 & 2. Meta-analysis of TBWL% at 6 -12 months of ESG+APC vs ESG = Experimental: Endoscopic Sleeve Gastroplasty + Argon Plasma Coagulation (ESG+APC). Control: Endoscopic Sleeve Gastroplasty (ESG). TBWL = Total Body Weight Loss; SD = Standardised Difference; SMD = Standardised Mean Difference; CI = confidence interval.
Figure: Figure 3. Meta-analysis of Adverse Events Rate of ESG+APC vs ESG = Experimental: Endoscopic Sleeve Gastroplasty + Argon Plasma Coagulation (ESG+APC). Control: Endoscopic Sleeve Gastroplasty (ESG). RR = relative risk; CI = confidence interval.
Disclosures:
Alan Ortega Macias indicated no relevant financial relationships.
Udita Gupta indicated no relevant financial relationships.
Pooja Viswanath indicated no relevant financial relationships.
Gicel Aguilar indicated no relevant financial relationships.
Adham Obeidat indicated no relevant financial relationships.
Gulshan Parasher indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Alan Gabriel. Ortega Macias, MD1, Udita Gupta, MD2, Pooja Viswanath, DO1, Gicel Jacklin. Aguilar, DO3, Adham Obeidat, MD4, Gulshan Parasher, MD, FACG1, Abu Baker Sheikh, MD2. P2711 - Efficacy and Safety of Enhanced Endoscopic Sleeve Gastroplasty With Argon Plasma Coagulation vs Endoscopic Sleeve Gastroplasty Alone: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
