Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2709 - Dual Treatment Approach to Obesity and End-Stage Organ Disease: Outcomes of Concomitant Bariatric Surgery and Solid Organ Transplantation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Kanisha Bahierathan, BS (she/her/hers)
Case Western Reserve University School of Medicine
Cleveland, OH
Presenting Author(s)
Award: ACG Presidential Poster Award
Kanisha Bahierathan, BS1, Leandro Sierra, MD2, Akash Khurana, MD3, Arjun Chatterjee, MD3, Roma Patel, MD3, Stephen Firkins, MD3, Roberto Simons-Linares, MD3
1Case Western Reserve University School of Medicine, Cleveland, OH; 2Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 3Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, OH
Introduction: Obesity is a potential barrier to organ transplantation, often rendering patients ineligible due to perioperative risk and poorer outcomes. While bariatric surgery can improve transplant eligibility by addressing obesity-related comorbidities, concerns regarding infection and surgical complications limit its implementation. Current literature focuses on bariatric surgery before or after transplantation, leaving the impact of simultaneous procedures underexplored. This study evaluates the safety and therapeutic benefit of concomitant bariatric and organ transplant surgery.
Methods: We retrospectively analyzed 215,000 patients who underwent bariatric surgery (2005-2025) using the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database. 64 patients underwent concomitant transplant and bariatric surgery and were propensity score-matched to 64 controls who had bariatric surgery alone, based on age, sex, race, ASA class, and key preoperative comorbidities (GERD, hypertension, hyperlipidemia, and diabetes). Our primary outcome was a composite measure of key perioperative events, including reoperation, any surgical or procedural reintervention, and hospital readmission within 30 days postoperatively. The secondary outcome assessed longitudinal trends in weight and BMI following surgery.
Results: Sixty-four patients (88% female; mean age 48.8 years; BMI 46.6 kg/m²) underwent transplant, who were matched to 64 controls who did not (72.3% female; mean age 51.6 years; BMI 45.7 kg/m²). No significant differences in the composite 30-day outcome of readmission, reoperation, or reintervention between the two groups (12.5% vs. 7.8%, p = 0.67) were found. Transplant patients had a significantly longer length of stay (5.4 vs. 1.4 days, p = 0.01), ASA Class (p < 0.001), and pre-op dialysis status (9.4% vs. 0%, p = 0.01); however, there were no significant differences in weight loss outcomes at 30 days, including BMI (3.84 vs. 2.29 kg/m², p = 0.12) and body weight (3.15 vs. 5.59 lbs, p = 0.42).
Discussion: Our findings suggest that concomitant organ transplantation and bariatric surgery is a viable approach, with consistent weight loss outcomes and no significant increase in short-term postoperative complications compared to bariatric surgery alone. This dual strategy offers a unique opportunity to address both end-stage organ disease and obesity in a single operative course, expanding access to organ transplant eligibility.
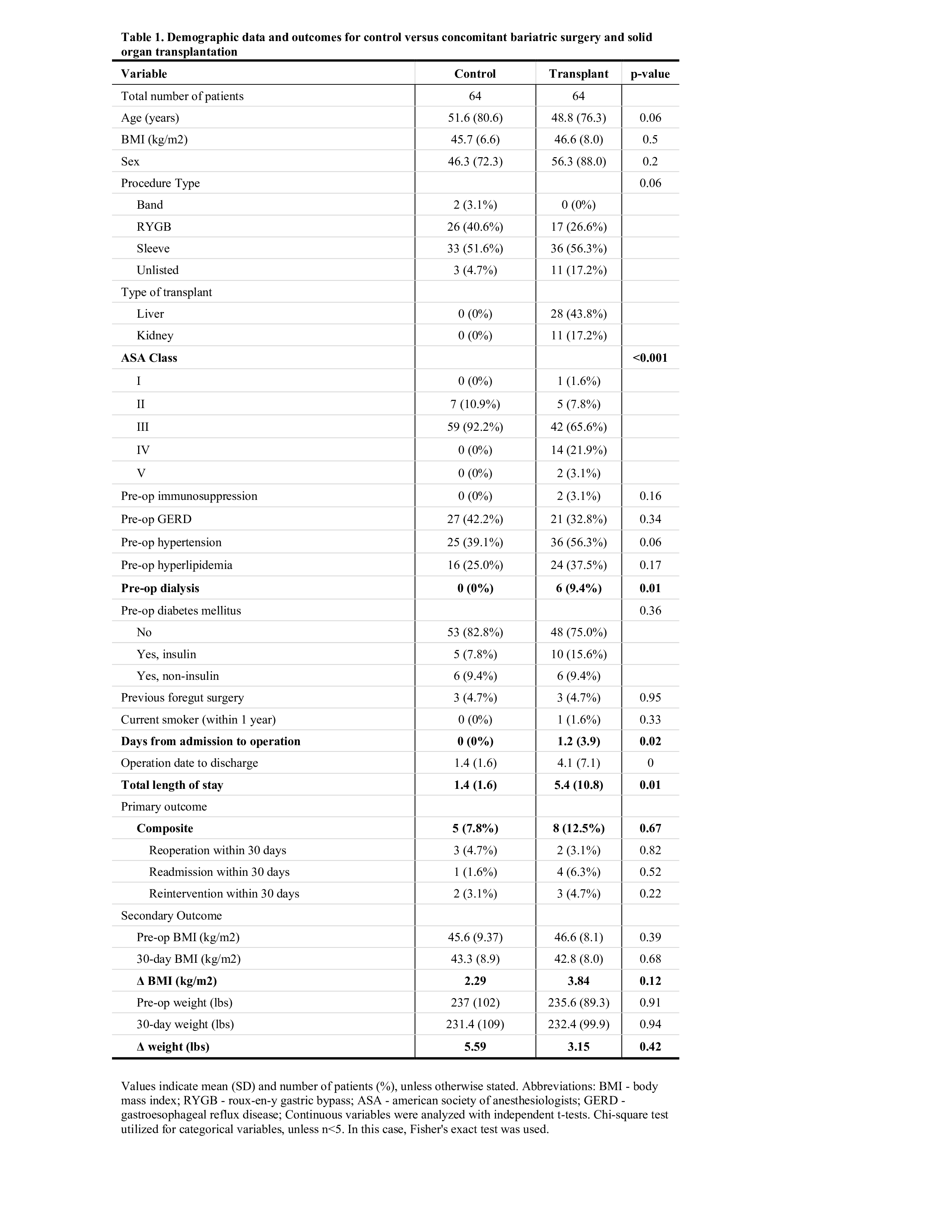
Figure: Values indicate mean (SD) and number of patients (%), unless otherwise stated. Abbreviations: BMI - body mass index; RYGB - roux-en-y gastric bypass; ASA - american society of anesthesiologists; GERD - gastroesophageal reflux disease; Continuous variables were analyzed with independent t-tests. Chi-square test utilized for categorical variables, unless n <5. In this case, Fisher's exact test was used.
Disclosures:
Kanisha Bahierathan indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Akash Khurana indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Roma Patel indicated no relevant financial relationships.
Stephen Firkins indicated no relevant financial relationships.
Roberto Simons-Linares indicated no relevant financial relationships.
Kanisha Bahierathan, BS1, Leandro Sierra, MD2, Akash Khurana, MD3, Arjun Chatterjee, MD3, Roma Patel, MD3, Stephen Firkins, MD3, Roberto Simons-Linares, MD3. P2709 - Dual Treatment Approach to Obesity and End-Stage Organ Disease: Outcomes of Concomitant Bariatric Surgery and Solid Organ Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Kanisha Bahierathan, BS1, Leandro Sierra, MD2, Akash Khurana, MD3, Arjun Chatterjee, MD3, Roma Patel, MD3, Stephen Firkins, MD3, Roberto Simons-Linares, MD3
1Case Western Reserve University School of Medicine, Cleveland, OH; 2Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 3Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, OH
Introduction: Obesity is a potential barrier to organ transplantation, often rendering patients ineligible due to perioperative risk and poorer outcomes. While bariatric surgery can improve transplant eligibility by addressing obesity-related comorbidities, concerns regarding infection and surgical complications limit its implementation. Current literature focuses on bariatric surgery before or after transplantation, leaving the impact of simultaneous procedures underexplored. This study evaluates the safety and therapeutic benefit of concomitant bariatric and organ transplant surgery.
Methods: We retrospectively analyzed 215,000 patients who underwent bariatric surgery (2005-2025) using the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database. 64 patients underwent concomitant transplant and bariatric surgery and were propensity score-matched to 64 controls who had bariatric surgery alone, based on age, sex, race, ASA class, and key preoperative comorbidities (GERD, hypertension, hyperlipidemia, and diabetes). Our primary outcome was a composite measure of key perioperative events, including reoperation, any surgical or procedural reintervention, and hospital readmission within 30 days postoperatively. The secondary outcome assessed longitudinal trends in weight and BMI following surgery.
Results: Sixty-four patients (88% female; mean age 48.8 years; BMI 46.6 kg/m²) underwent transplant, who were matched to 64 controls who did not (72.3% female; mean age 51.6 years; BMI 45.7 kg/m²). No significant differences in the composite 30-day outcome of readmission, reoperation, or reintervention between the two groups (12.5% vs. 7.8%, p = 0.67) were found. Transplant patients had a significantly longer length of stay (5.4 vs. 1.4 days, p = 0.01), ASA Class (p < 0.001), and pre-op dialysis status (9.4% vs. 0%, p = 0.01); however, there were no significant differences in weight loss outcomes at 30 days, including BMI (3.84 vs. 2.29 kg/m², p = 0.12) and body weight (3.15 vs. 5.59 lbs, p = 0.42).
Discussion: Our findings suggest that concomitant organ transplantation and bariatric surgery is a viable approach, with consistent weight loss outcomes and no significant increase in short-term postoperative complications compared to bariatric surgery alone. This dual strategy offers a unique opportunity to address both end-stage organ disease and obesity in a single operative course, expanding access to organ transplant eligibility.
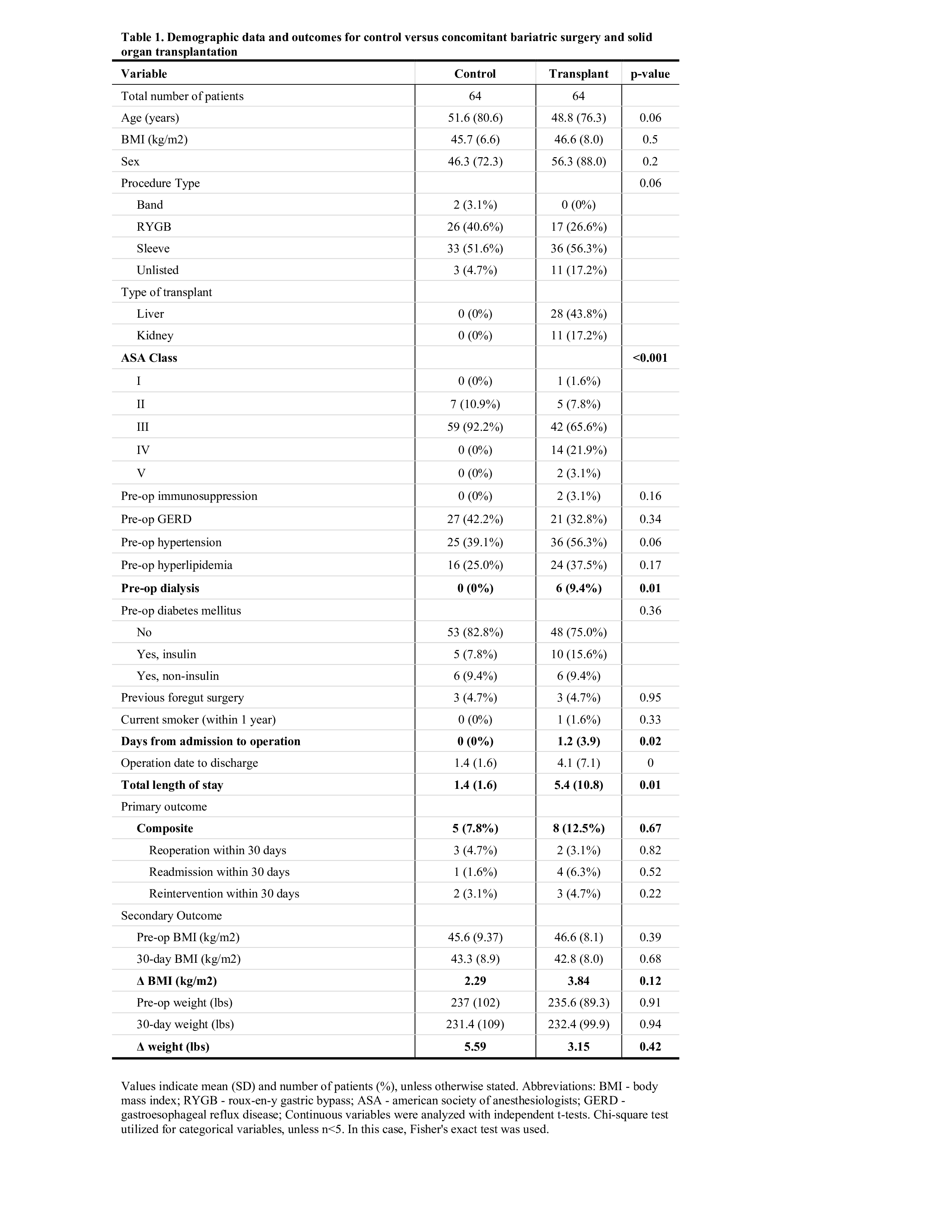
Figure: Values indicate mean (SD) and number of patients (%), unless otherwise stated. Abbreviations: BMI - body mass index; RYGB - roux-en-y gastric bypass; ASA - american society of anesthesiologists; GERD - gastroesophageal reflux disease; Continuous variables were analyzed with independent t-tests. Chi-square test utilized for categorical variables, unless n <5. In this case, Fisher's exact test was used.
Disclosures:
Kanisha Bahierathan indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Akash Khurana indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Roma Patel indicated no relevant financial relationships.
Stephen Firkins indicated no relevant financial relationships.
Roberto Simons-Linares indicated no relevant financial relationships.
Kanisha Bahierathan, BS1, Leandro Sierra, MD2, Akash Khurana, MD3, Arjun Chatterjee, MD3, Roma Patel, MD3, Stephen Firkins, MD3, Roberto Simons-Linares, MD3. P2709 - Dual Treatment Approach to Obesity and End-Stage Organ Disease: Outcomes of Concomitant Bariatric Surgery and Solid Organ Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


