Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2708 - Geographic and Demographic Disparities in Obesity-Related Mortality for Acute Abdominal Emergencies: A US Perspective (1999-2020)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Azeem Khalid, MD (he/him/his)
Aiken Regional Medical Centers
Aiken, SC
Presenting Author(s)
Haneen Kamran, MBBS1, Juaquito Jorge, MD2, Sameen Tahira, MBBS1, Muhammad Umer, MBBS3, Umm e Aimen Minhas, MBBS1, Muhammad Ahsan Asif, MBBS4, Azeem Khalid, MD5
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2Private Practice/Independent Clinical Affiliate, USA, Chicago, IL; 3Sahiwal Medical College, Sahiwal, Punjab, Pakistan; 4Jinnah Hospital Lahore, Lahore, Punjab, Pakistan; 5Aiken Regional Medical Centers, Aiken, SC
Introduction: Obesity is increasingly recognized as a contributing factor in deaths from acute abdominal conditions such as obstruction, ischemia, and perforation. While these emergencies carry high mortality, national data on the role of obesity in such deaths remain limited. Prior studies focus on surgical cohorts, overlooking broader population trends. This study analyzes U.S. mortality records to assess temporal and demographic patterns in deaths where both obesity and acute abdominal emergencies were listed as contributing causes.
Methods: Mortality data were extracted from the CDC WONDER database (1999-2020), identifying deaths using ICD-10 codes for obesity (E66) and acute abdominal emergencies, including perforations, obstruction, acute ischemia, complicated diverticular disease, and ruptured abdominal aortic aneurysm. Age-adjusted mortality rates (AAMRs) per 1,000,000 population were calculated using the 2000 U.S. standard population. Joinpoint regression evaluated annual percent changes (APCs), with statistical significance defined as a 95% confidence interval (CI) excluding zero (P< 0.05). Following STROBE guidelines, demographic and geographic factors were analyzed for patients aged ≥18 years, accounting for the growing burden of obesity among younger adults.
Results: Between 1999 and 2020, 14,830 deaths were recorded (AAMR:2.16), with a significant overall rise in mortality (APC=3.42, CI:2.66-4.19). Females had a higher AAMR (2.28) compared to males (1.99), both genders showing a significant gradual rise in mortality till 2018 (APC=1.95 vs. 3.49), followed by a significant sharp increase 2018 onwards (APC=18.51, CI: 3.06-36.28 vs. 20.90, CI:6.16-37.70). Racial disparities were marked, American Indian/Alaska Natives had the highest AAMR (3.97), followed by non-Hispanic (NH) Blacks (2.75), NH Whites (2.19), and Hispanics (1.83); Asian/Pacific Islanders had the lowest (0.38) Regionally, the West reported the highest AAMR (2.58), while the Northeast had the lowest (1.76). At the state level, Vermont had the highest rate (5.94) and Virginia the lowest (1.03). Mortality was also higher in non-metro micropolitan areas (2.84) compared to large fringe metropolitan areas (1.67).
Discussion: The sharp recent rise in obesity-related mortality from acute abdominal emergencies, especially among rural and Indigenous populations, highlights the need for targeted health policy reforms addressing surgical access, perioperative care, and social determinants of health.
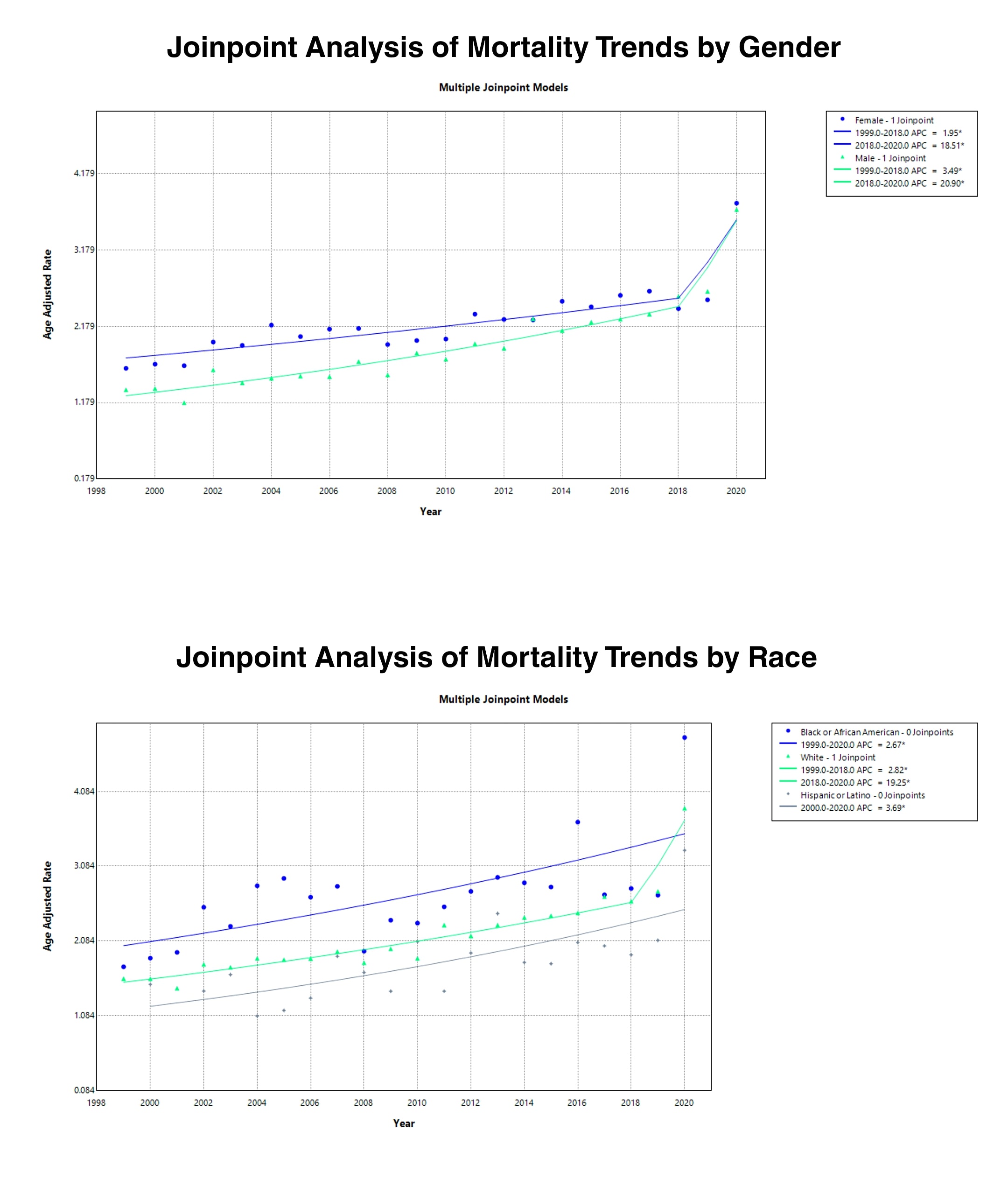
Figure: Figure 1: Central illustration of Geographic and Demographic Disparities in Obesity-Related Mortality for Acute Abdominal Emergencies in the U.S.
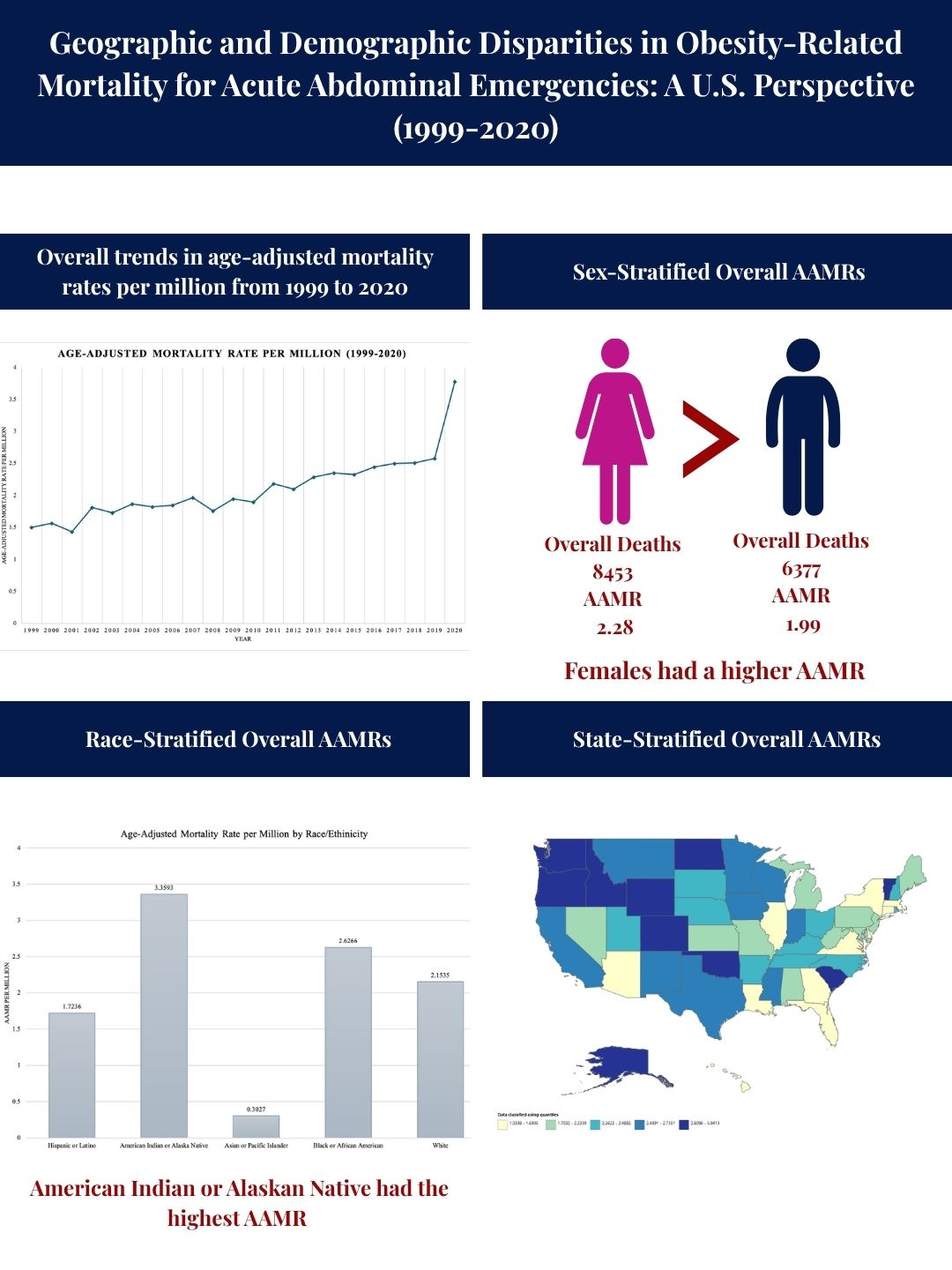
Figure: Figure 2: Joinpoint Regression Analysis for Obesity-Related Mortality for Acute Abdominal Emergencies in the U.S.
Disclosures:
Haneen Kamran indicated no relevant financial relationships.
Juaquito Jorge indicated no relevant financial relationships.
Sameen Tahira indicated no relevant financial relationships.
Muhammad Umer indicated no relevant financial relationships.
Umm e Aimen Minhas indicated no relevant financial relationships.
Muhammad Ahsan Asif indicated no relevant financial relationships.
Azeem Khalid indicated no relevant financial relationships.
Haneen Kamran, MBBS1, Juaquito Jorge, MD2, Sameen Tahira, MBBS1, Muhammad Umer, MBBS3, Umm e Aimen Minhas, MBBS1, Muhammad Ahsan Asif, MBBS4, Azeem Khalid, MD5. P2708 - Geographic and Demographic Disparities in Obesity-Related Mortality for Acute Abdominal Emergencies: A US Perspective (1999-2020), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2Private Practice/Independent Clinical Affiliate, USA, Chicago, IL; 3Sahiwal Medical College, Sahiwal, Punjab, Pakistan; 4Jinnah Hospital Lahore, Lahore, Punjab, Pakistan; 5Aiken Regional Medical Centers, Aiken, SC
Introduction: Obesity is increasingly recognized as a contributing factor in deaths from acute abdominal conditions such as obstruction, ischemia, and perforation. While these emergencies carry high mortality, national data on the role of obesity in such deaths remain limited. Prior studies focus on surgical cohorts, overlooking broader population trends. This study analyzes U.S. mortality records to assess temporal and demographic patterns in deaths where both obesity and acute abdominal emergencies were listed as contributing causes.
Methods: Mortality data were extracted from the CDC WONDER database (1999-2020), identifying deaths using ICD-10 codes for obesity (E66) and acute abdominal emergencies, including perforations, obstruction, acute ischemia, complicated diverticular disease, and ruptured abdominal aortic aneurysm. Age-adjusted mortality rates (AAMRs) per 1,000,000 population were calculated using the 2000 U.S. standard population. Joinpoint regression evaluated annual percent changes (APCs), with statistical significance defined as a 95% confidence interval (CI) excluding zero (P< 0.05). Following STROBE guidelines, demographic and geographic factors were analyzed for patients aged ≥18 years, accounting for the growing burden of obesity among younger adults.
Results: Between 1999 and 2020, 14,830 deaths were recorded (AAMR:2.16), with a significant overall rise in mortality (APC=3.42, CI:2.66-4.19). Females had a higher AAMR (2.28) compared to males (1.99), both genders showing a significant gradual rise in mortality till 2018 (APC=1.95 vs. 3.49), followed by a significant sharp increase 2018 onwards (APC=18.51, CI: 3.06-36.28 vs. 20.90, CI:6.16-37.70). Racial disparities were marked, American Indian/Alaska Natives had the highest AAMR (3.97), followed by non-Hispanic (NH) Blacks (2.75), NH Whites (2.19), and Hispanics (1.83); Asian/Pacific Islanders had the lowest (0.38) Regionally, the West reported the highest AAMR (2.58), while the Northeast had the lowest (1.76). At the state level, Vermont had the highest rate (5.94) and Virginia the lowest (1.03). Mortality was also higher in non-metro micropolitan areas (2.84) compared to large fringe metropolitan areas (1.67).
Discussion: The sharp recent rise in obesity-related mortality from acute abdominal emergencies, especially among rural and Indigenous populations, highlights the need for targeted health policy reforms addressing surgical access, perioperative care, and social determinants of health.
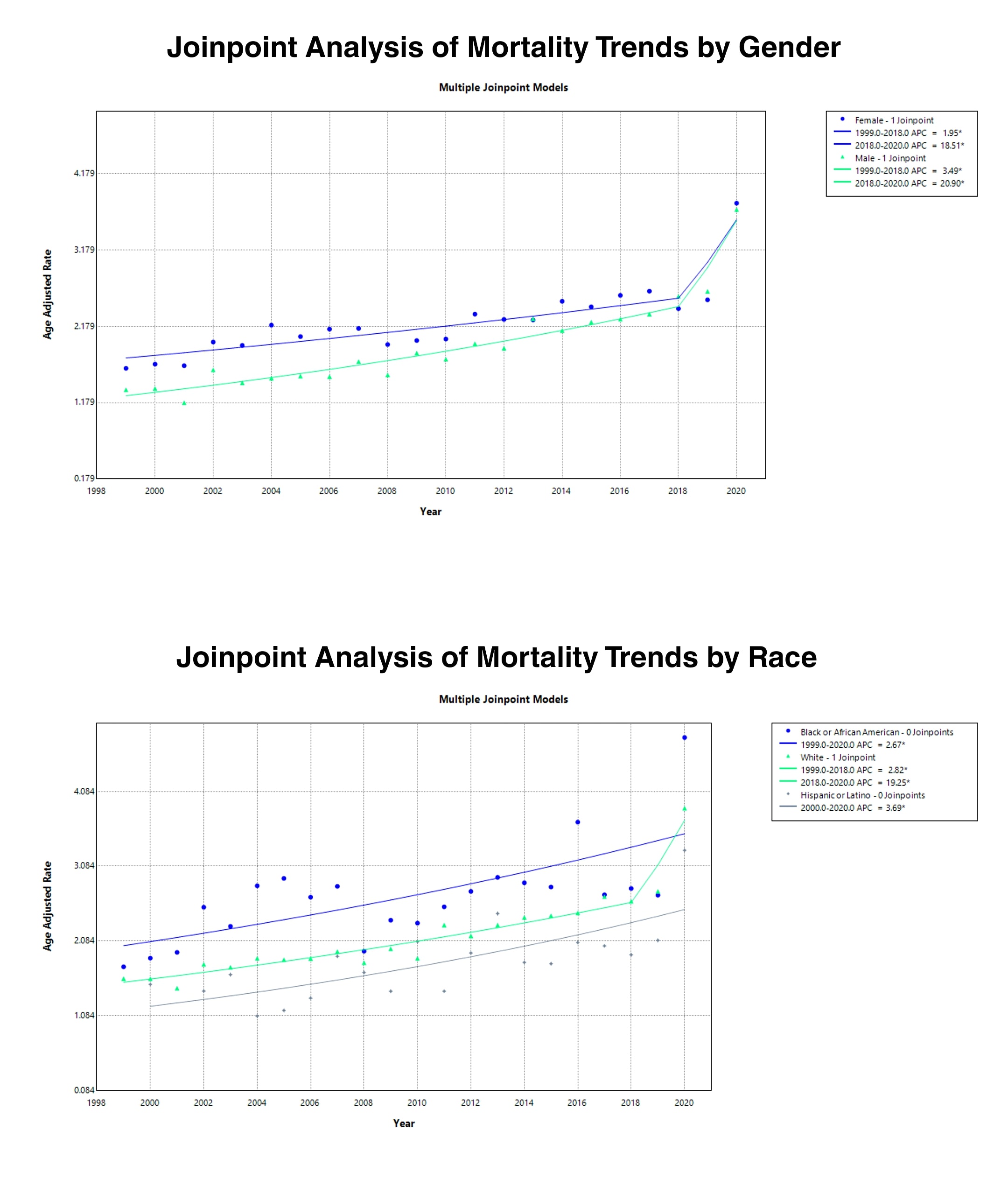
Figure: Figure 1: Central illustration of Geographic and Demographic Disparities in Obesity-Related Mortality for Acute Abdominal Emergencies in the U.S.
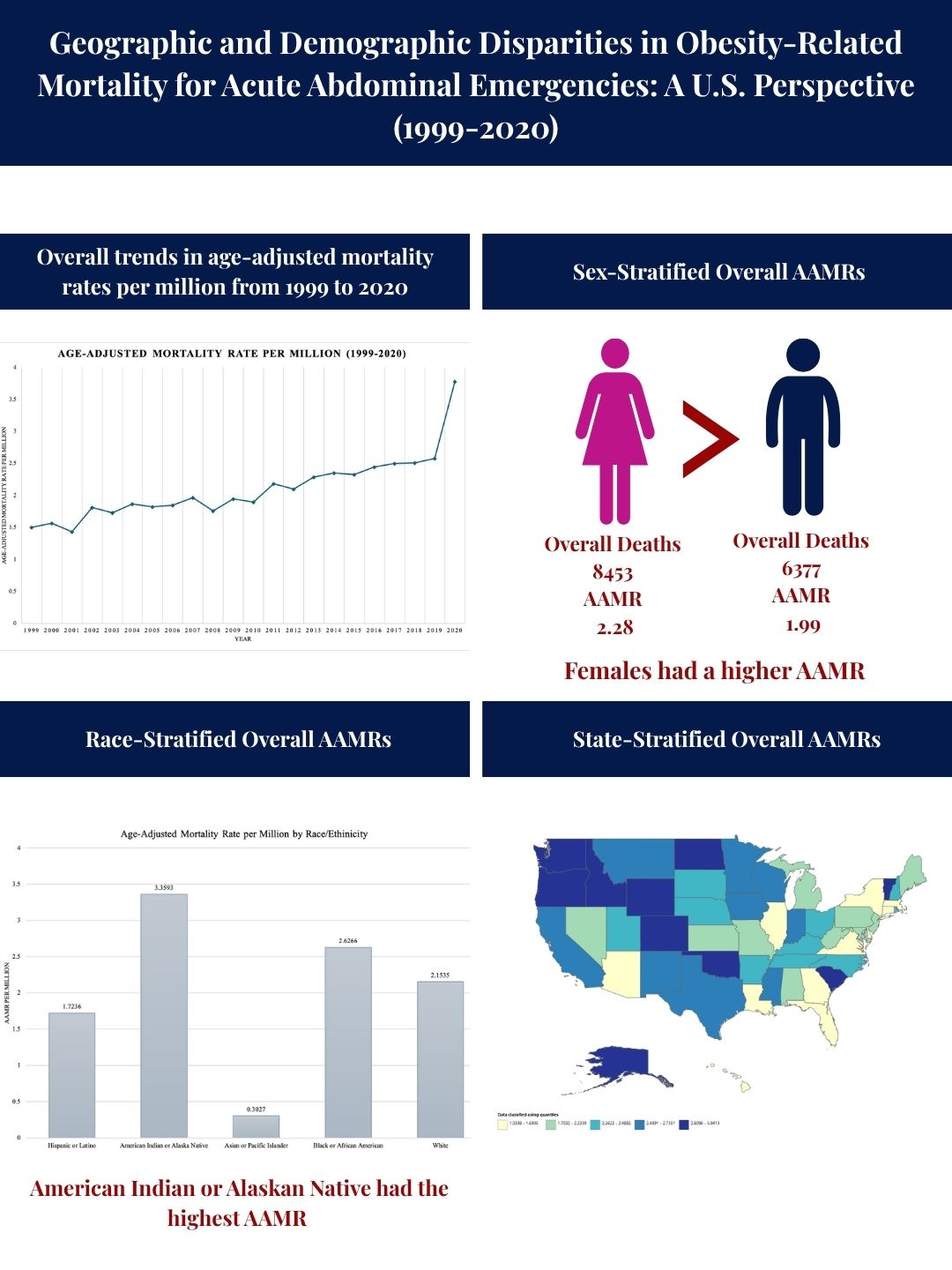
Figure: Figure 2: Joinpoint Regression Analysis for Obesity-Related Mortality for Acute Abdominal Emergencies in the U.S.
Disclosures:
Haneen Kamran indicated no relevant financial relationships.
Juaquito Jorge indicated no relevant financial relationships.
Sameen Tahira indicated no relevant financial relationships.
Muhammad Umer indicated no relevant financial relationships.
Umm e Aimen Minhas indicated no relevant financial relationships.
Muhammad Ahsan Asif indicated no relevant financial relationships.
Azeem Khalid indicated no relevant financial relationships.
Haneen Kamran, MBBS1, Juaquito Jorge, MD2, Sameen Tahira, MBBS1, Muhammad Umer, MBBS3, Umm e Aimen Minhas, MBBS1, Muhammad Ahsan Asif, MBBS4, Azeem Khalid, MD5. P2708 - Geographic and Demographic Disparities in Obesity-Related Mortality for Acute Abdominal Emergencies: A US Perspective (1999-2020), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
