Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2699 - Body Weight and Stool Form Alter Diurnal Breath Gas Levels
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MB
Madeline Berschback, MD (she/her/hers)
Massachusetts General Hospital
Boston, MA
Presenting Author(s)
Award: ACG Presidential Poster Award
Madeline Berschback, MD1, Robert Burke, MSc2, Barry McBride, MSc2, Claire Shortt, PhD2, Aonghus Shortt, PhD2, Ciara Kernan, BSc2, Kyle Staller, MD, MPH1
1Massachusetts General Hospital, Boston, MA; 2FoodMarble, Dublin, Dublin, Ireland
Introduction: Breath gases such as hydrogen (H₂) and methane (CH₄), are direct markers of GI activity, reflecting microbial fermentation and transit dynamics. Previous studies have linked post-prandial gas measurements to GI symptoms, stool form, and body weight, likely through their shared influence on gut motility and microbiome composition. In this real-world study, non-fasting breath H2 and CH4 levels were analyzed alongside BMI and stool scores to explore their combined relationship with GI motility and underlying microbiome activity.
Methods: We studied 572 individuals (48±13.9 yrs, 75.9% Female) with varying BMI who logged symptoms while consuming their habitual diet for 1 week using an app-connected H2 and CH4 device (FoodMarble, Ireland). Subjects took hourly breath readings and recorded stool form (Bristol Stool Scale). A linear mixed-effects model (LMEM) was used to evaluate the relationship between BMI and stool with breath gases for the underweight and obese categories. We used the hourly breath gas levels as the dependent variable and BMI, stool form and time as fixed effects. The underweight and obese groups were considered reference groups for the LMEM, and random intercepts were introduced to account for individual variability. Chi-squared tests were used to determine the similarity in stool composition of the groups.
Results: Underweight and obese groups had different proportions of constipated and diarrheal patients (χ²=7.94, p=0.047) with the underweight and obese groups having a higher proportion of constipated and diarrheal participants respectively. After adjusting for stool, there was a significant positive association between BMI and H2 (β=1.693, p=0.023). There was a negative association between BMI and CH4 levels, although this did not reach significance (β=-1.659, p=0.102). After accounting for BMI, the diarrheal cohort had a significant negative association with CH4 levels (β=-2.810, p=0.017).
Discussion: Obese participants had higher H2, beyond what would be explained by the higher proportions of diarrheal participants. Underweight participants had higher CH4 yet when adjusted for BSS, this association was no longer significant. However, the proportion of underweight participants was lower. Overall, incorporating both body weight and stool form in the interpretation of breath gas monitoring, has the potential for more personalized care and better predict response to treatment.
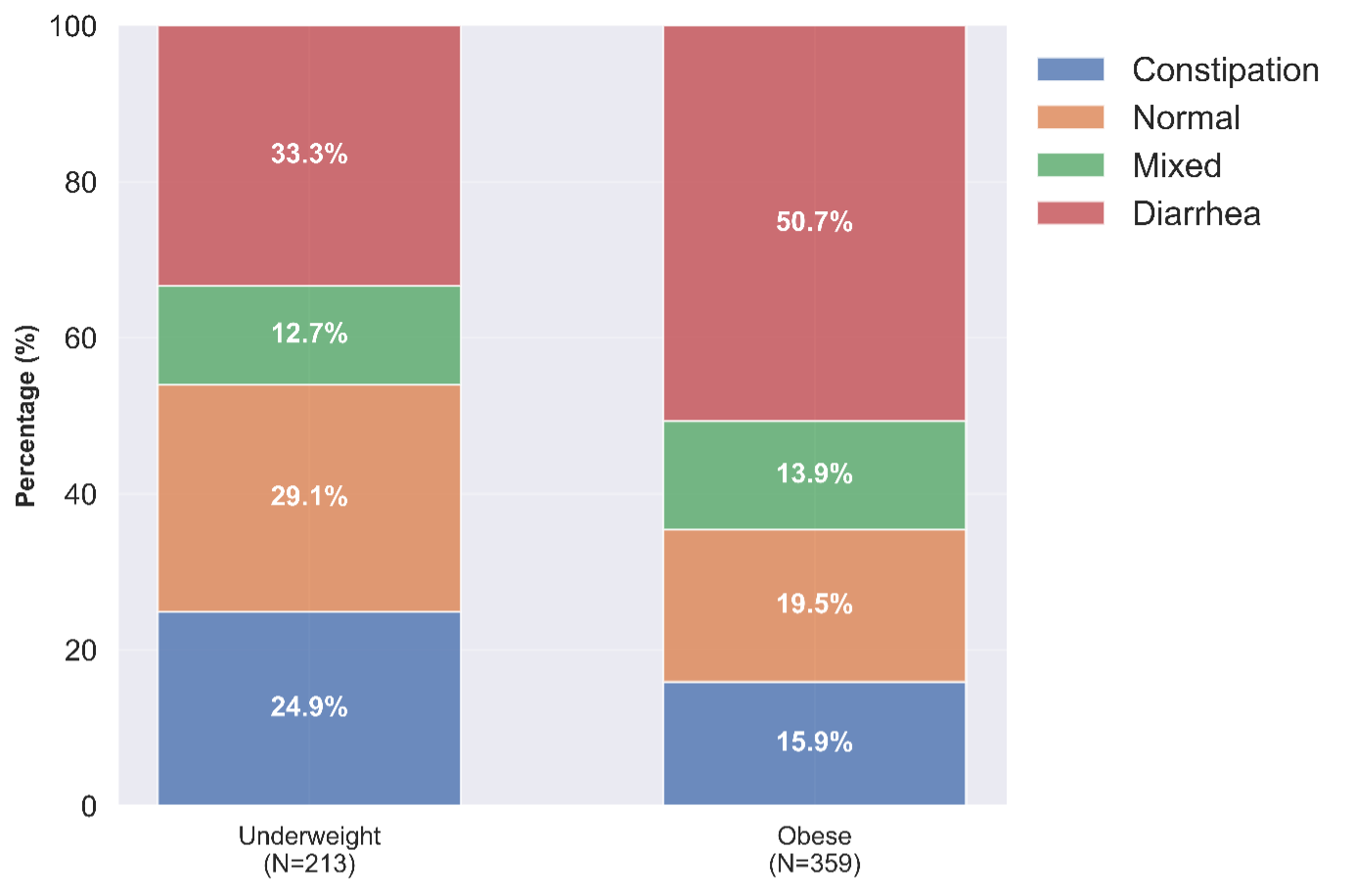
Figure: Non-fasted breath hydrogen (left) and breath methane (right) profiles for the underweight (blue) and obese (orange) groups.
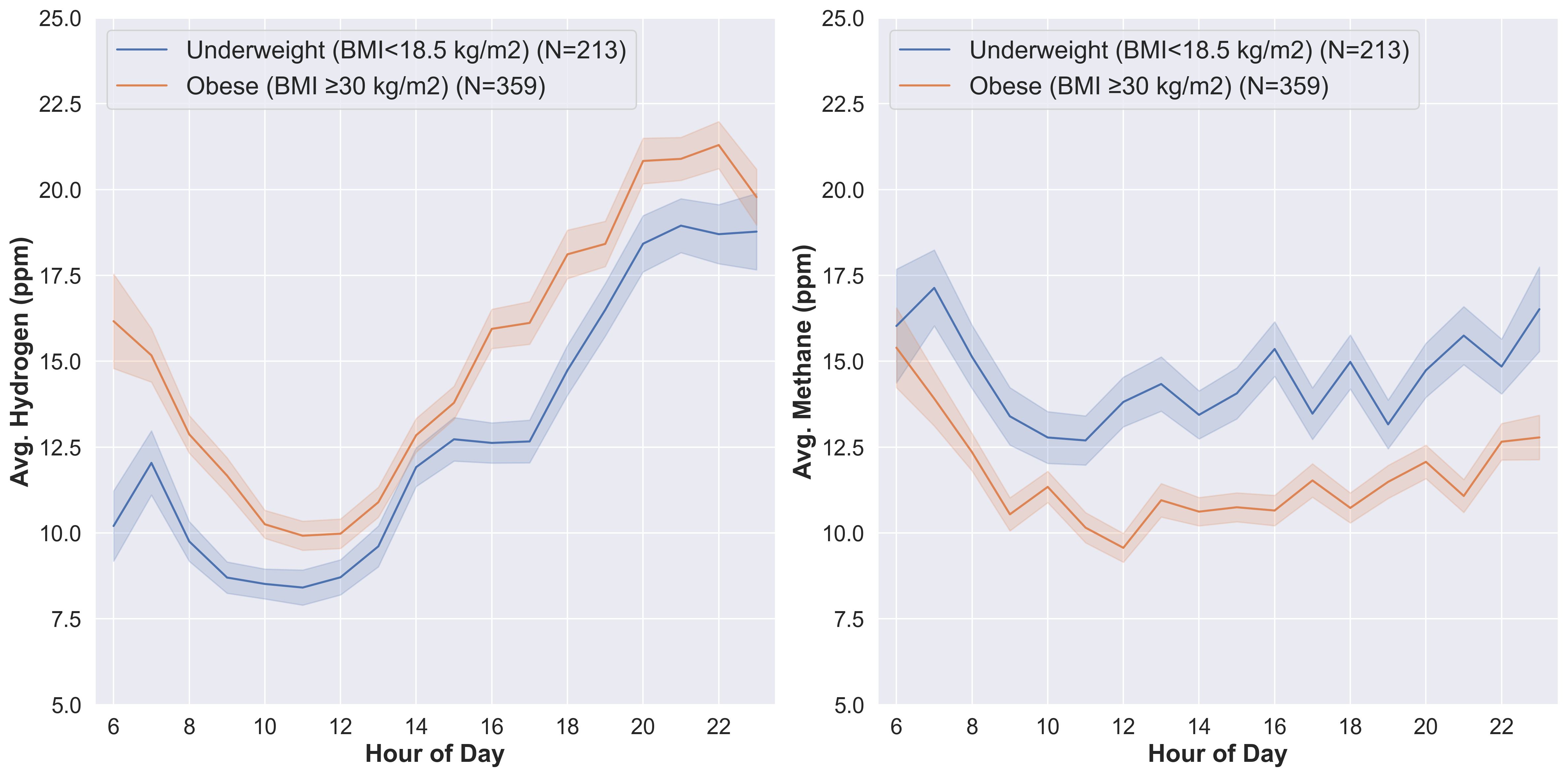
Figure: Relative percentage of BSS types within the underweight (left) and obese (right) BMI groups. Proportions of each BSS type are significantly different between the underweight and obese BMI groups.
Disclosures:
Madeline Berschback indicated no relevant financial relationships.
Robert Burke: FoodMarble Digestive Health – Employee.
Barry McBride: FoodMarble Digestive Health – Employee.
Claire Shortt: FoodMarble Digestive Health – Employee.
Aonghus Shortt: FoodMarble Digestive Health – Owner/Ownership Interest.
Ciara Kernan: FoodMarble Digestive Health – Employee.
Kyle Staller: Ardelyx – Grant/Research Support. Gemelli – Consultant. Laborie – Consultant. Mahana – Consultant. Salix – Consultant. Takeda – Expert witness.
Madeline Berschback, MD1, Robert Burke, MSc2, Barry McBride, MSc2, Claire Shortt, PhD2, Aonghus Shortt, PhD2, Ciara Kernan, BSc2, Kyle Staller, MD, MPH1. P2699 - Body Weight and Stool Form Alter Diurnal Breath Gas Levels, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Madeline Berschback, MD1, Robert Burke, MSc2, Barry McBride, MSc2, Claire Shortt, PhD2, Aonghus Shortt, PhD2, Ciara Kernan, BSc2, Kyle Staller, MD, MPH1
1Massachusetts General Hospital, Boston, MA; 2FoodMarble, Dublin, Dublin, Ireland
Introduction: Breath gases such as hydrogen (H₂) and methane (CH₄), are direct markers of GI activity, reflecting microbial fermentation and transit dynamics. Previous studies have linked post-prandial gas measurements to GI symptoms, stool form, and body weight, likely through their shared influence on gut motility and microbiome composition. In this real-world study, non-fasting breath H2 and CH4 levels were analyzed alongside BMI and stool scores to explore their combined relationship with GI motility and underlying microbiome activity.
Methods: We studied 572 individuals (48±13.9 yrs, 75.9% Female) with varying BMI who logged symptoms while consuming their habitual diet for 1 week using an app-connected H2 and CH4 device (FoodMarble, Ireland). Subjects took hourly breath readings and recorded stool form (Bristol Stool Scale). A linear mixed-effects model (LMEM) was used to evaluate the relationship between BMI and stool with breath gases for the underweight and obese categories. We used the hourly breath gas levels as the dependent variable and BMI, stool form and time as fixed effects. The underweight and obese groups were considered reference groups for the LMEM, and random intercepts were introduced to account for individual variability. Chi-squared tests were used to determine the similarity in stool composition of the groups.
Results: Underweight and obese groups had different proportions of constipated and diarrheal patients (χ²=7.94, p=0.047) with the underweight and obese groups having a higher proportion of constipated and diarrheal participants respectively. After adjusting for stool, there was a significant positive association between BMI and H2 (β=1.693, p=0.023). There was a negative association between BMI and CH4 levels, although this did not reach significance (β=-1.659, p=0.102). After accounting for BMI, the diarrheal cohort had a significant negative association with CH4 levels (β=-2.810, p=0.017).
Discussion: Obese participants had higher H2, beyond what would be explained by the higher proportions of diarrheal participants. Underweight participants had higher CH4 yet when adjusted for BSS, this association was no longer significant. However, the proportion of underweight participants was lower. Overall, incorporating both body weight and stool form in the interpretation of breath gas monitoring, has the potential for more personalized care and better predict response to treatment.
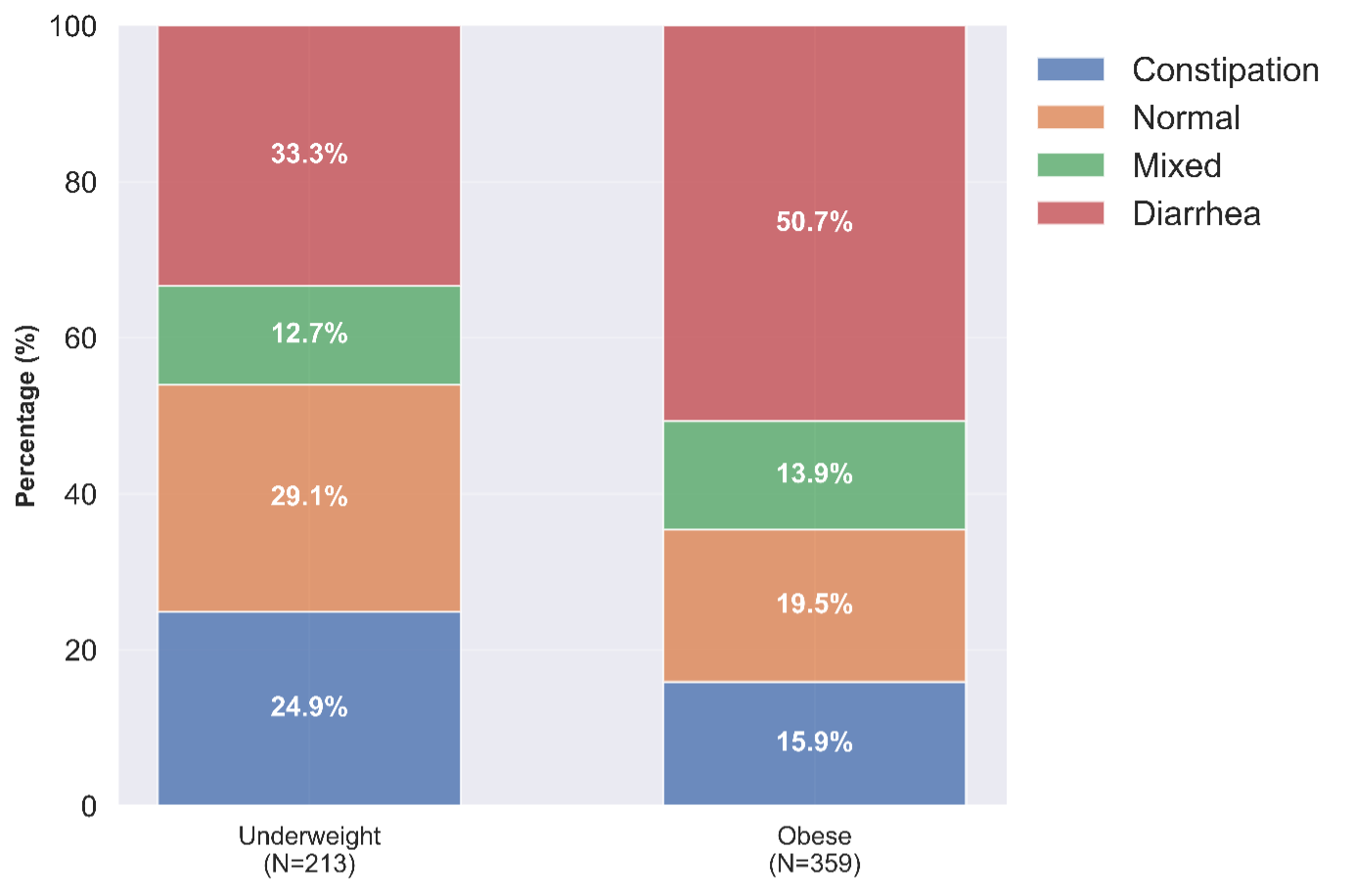
Figure: Non-fasted breath hydrogen (left) and breath methane (right) profiles for the underweight (blue) and obese (orange) groups.
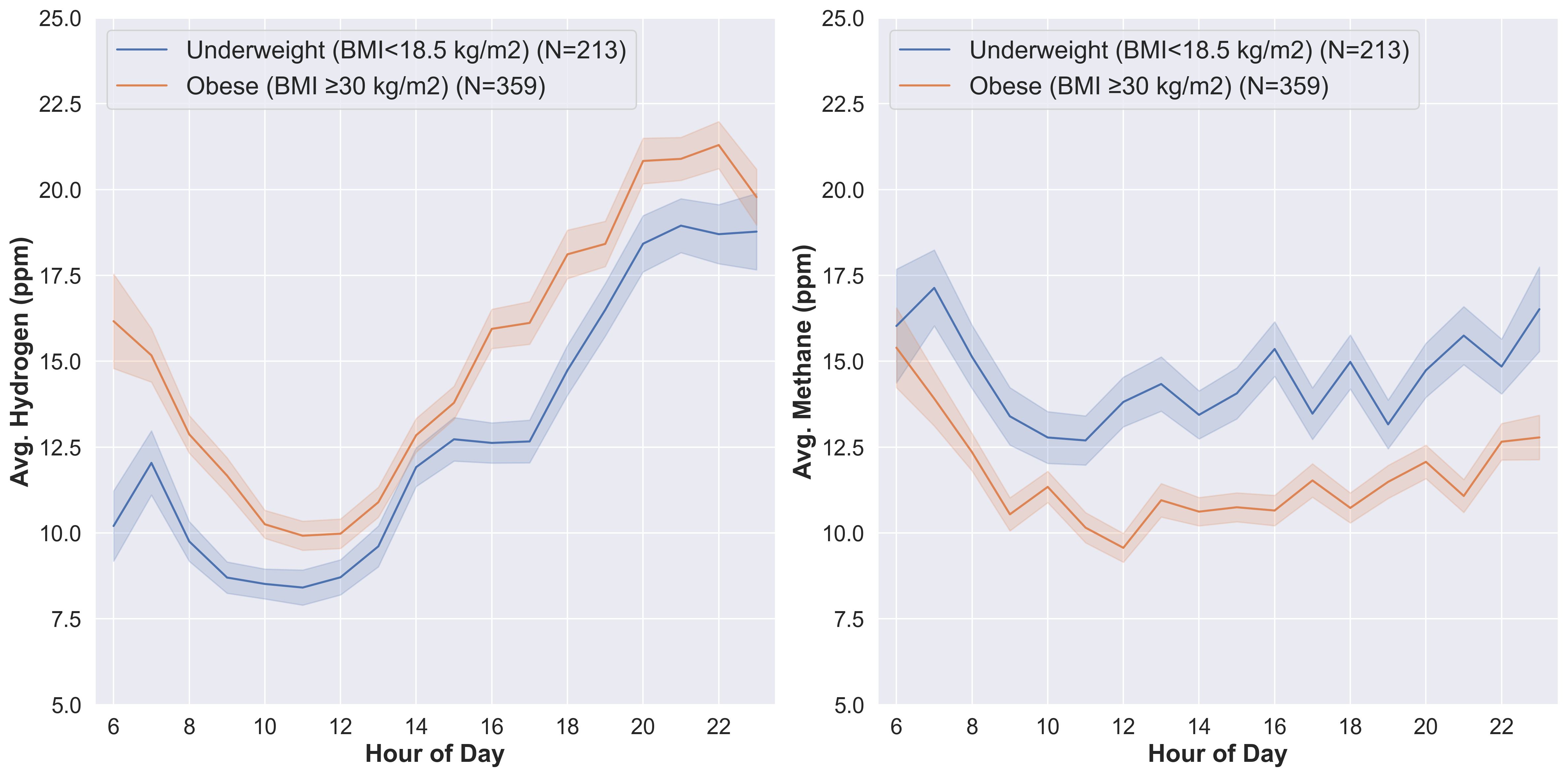
Figure: Relative percentage of BSS types within the underweight (left) and obese (right) BMI groups. Proportions of each BSS type are significantly different between the underweight and obese BMI groups.
Disclosures:
Madeline Berschback indicated no relevant financial relationships.
Robert Burke: FoodMarble Digestive Health – Employee.
Barry McBride: FoodMarble Digestive Health – Employee.
Claire Shortt: FoodMarble Digestive Health – Employee.
Aonghus Shortt: FoodMarble Digestive Health – Owner/Ownership Interest.
Ciara Kernan: FoodMarble Digestive Health – Employee.
Kyle Staller: Ardelyx – Grant/Research Support. Gemelli – Consultant. Laborie – Consultant. Mahana – Consultant. Salix – Consultant. Takeda – Expert witness.
Madeline Berschback, MD1, Robert Burke, MSc2, Barry McBride, MSc2, Claire Shortt, PhD2, Aonghus Shortt, PhD2, Ciara Kernan, BSc2, Kyle Staller, MD, MPH1. P2699 - Body Weight and Stool Form Alter Diurnal Breath Gas Levels, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


