Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2697 - GLP-1 Receptor Agonist Utilization: A National Analysis of Access Disparities in US Adults
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Tasnin Khan, DO (she/her/hers)
Lenox Hill Hospital, Northwell Health
New York, NY
Presenting Author(s)
Tasnin Khan, DO, Abdallah Beano, MD
Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: GLP-1 receptor agonists have transformed obesity therapeutics with expanding application beyond diabetes management, including NAFLD and potential benefits to groups facing increased obesity risk such as IBD patients treated with corticosteroids. With broader FDA approvals for obesity management, it is essential to examine utilization patterns across diverse patient populations to ensure equitable access. This study explores GLP-1 use patterns in U.S. adults with diabetes and/or obesity to identify potential access barriers and demographic differences.
Methods: We conducted a cross-sectional analysis of U.S. adults ≥18 years with diabetes and/or obesity (BMI≥30) using National Health and Nutrition Examination Survey (NHANES) 2017–March 2020 data (n=4,362). Prescription files identified GLP-1 users. Primary outcomes were utilization rates across demographic and clinical factors (age, gender, race/ethnicity, income, education, BMI). Statistical analysis was performed using chi-square tests (p< 0.05). One GLP-1 user without obesity or diabetes was excluded.
Results: GLP-1 use was 1.5% in those with diabetes and/or obesity (67/4,362). Significant differences existed by clinical sub-group: lowest in obesity-only group (2/2,939, 0.1%) versus diabetes-only (17/674, 2.5%) and diabetes with obesity (48/749, 6.4%, p< 0.001). Age was significant, with lower use in 18-39 years (1/1,170, 0.1%), versus ages 40-59 (34/1,514, 2.2%) and age ≥60 (32/1,624, 2.0%, p< 0.001). Class II/III Obesity had higher use than Class I group (33/1,783, 1.9% vs. 17/1,854, 0.9% respectively, p=0.008). Use across race/ethnicity varied from 0.7% (Asian) to 1.8% (Black/White) but remained non-significant (p=0.493). Income, education, and gender showed no significant associations.
Discussion: Our analysis reveals critically low GLP-1 utilization (1.5%) with a 64-fold difference between diabetes with obesity patients (6.4%) versus obesity-only patients (0.1%), consistent with diabetes-centered prescribing patterns when obesity approvals were limited. The virtual absence of use in young adults (0.1%) was striking, representing a gap in prevention opportunities in a population with rising obesity prevalence. Although racial disparities were non-significant, the small sample size of GLP-1 users may mask access barriers rather than reflecting true equity. Future research should employ larger datasets and claims analyses, particularly among complex patient populations such as IBD patients with corticosteroid-related obesity risks.
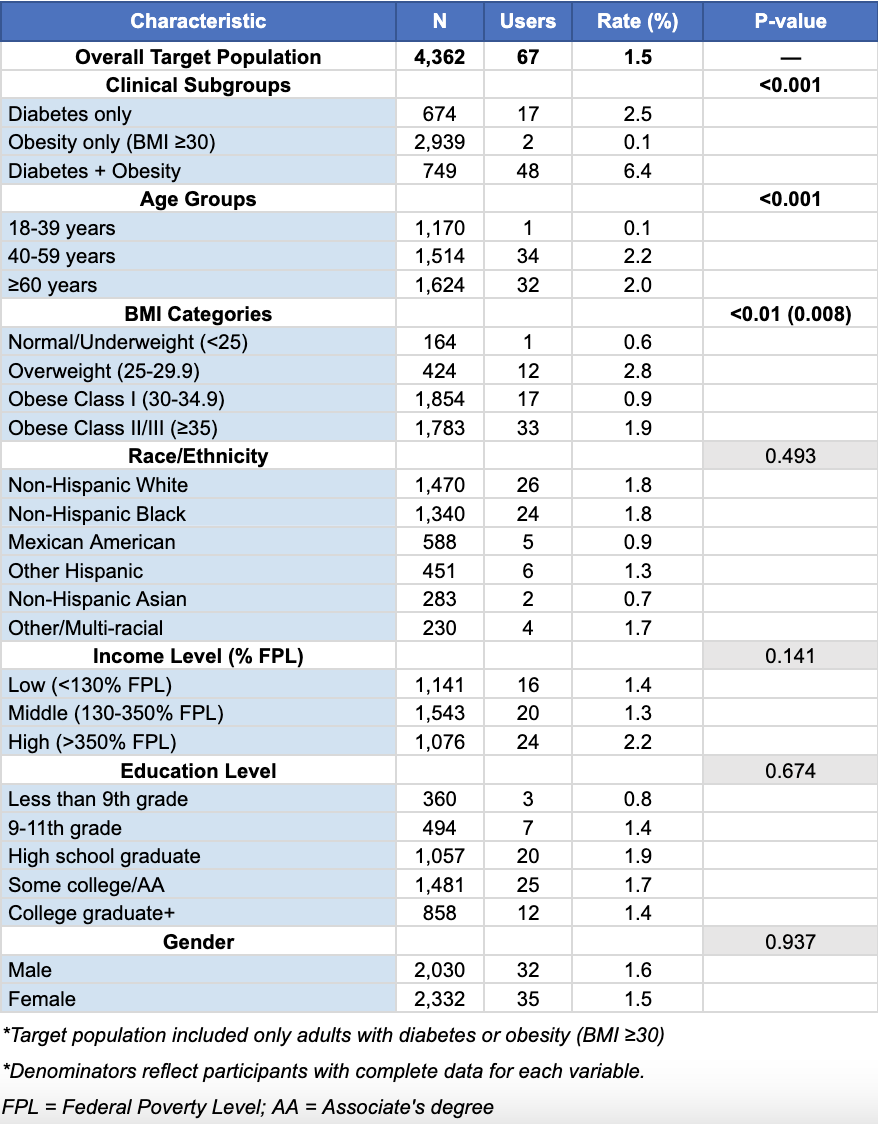
Figure: Table 1. GLP-1 Receptor Agonist Utilization Among Adults with Diabetes and/or Obesity, NHANES 2017-2020
Disclosures:
Tasnin Khan indicated no relevant financial relationships.
Abdallah Beano indicated no relevant financial relationships.
Tasnin Khan, DO, Abdallah Beano, MD. P2697 - GLP-1 Receptor Agonist Utilization: A National Analysis of Access Disparities in US Adults, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: GLP-1 receptor agonists have transformed obesity therapeutics with expanding application beyond diabetes management, including NAFLD and potential benefits to groups facing increased obesity risk such as IBD patients treated with corticosteroids. With broader FDA approvals for obesity management, it is essential to examine utilization patterns across diverse patient populations to ensure equitable access. This study explores GLP-1 use patterns in U.S. adults with diabetes and/or obesity to identify potential access barriers and demographic differences.
Methods: We conducted a cross-sectional analysis of U.S. adults ≥18 years with diabetes and/or obesity (BMI≥30) using National Health and Nutrition Examination Survey (NHANES) 2017–March 2020 data (n=4,362). Prescription files identified GLP-1 users. Primary outcomes were utilization rates across demographic and clinical factors (age, gender, race/ethnicity, income, education, BMI). Statistical analysis was performed using chi-square tests (p< 0.05). One GLP-1 user without obesity or diabetes was excluded.
Results: GLP-1 use was 1.5% in those with diabetes and/or obesity (67/4,362). Significant differences existed by clinical sub-group: lowest in obesity-only group (2/2,939, 0.1%) versus diabetes-only (17/674, 2.5%) and diabetes with obesity (48/749, 6.4%, p< 0.001). Age was significant, with lower use in 18-39 years (1/1,170, 0.1%), versus ages 40-59 (34/1,514, 2.2%) and age ≥60 (32/1,624, 2.0%, p< 0.001). Class II/III Obesity had higher use than Class I group (33/1,783, 1.9% vs. 17/1,854, 0.9% respectively, p=0.008). Use across race/ethnicity varied from 0.7% (Asian) to 1.8% (Black/White) but remained non-significant (p=0.493). Income, education, and gender showed no significant associations.
Discussion: Our analysis reveals critically low GLP-1 utilization (1.5%) with a 64-fold difference between diabetes with obesity patients (6.4%) versus obesity-only patients (0.1%), consistent with diabetes-centered prescribing patterns when obesity approvals were limited. The virtual absence of use in young adults (0.1%) was striking, representing a gap in prevention opportunities in a population with rising obesity prevalence. Although racial disparities were non-significant, the small sample size of GLP-1 users may mask access barriers rather than reflecting true equity. Future research should employ larger datasets and claims analyses, particularly among complex patient populations such as IBD patients with corticosteroid-related obesity risks.
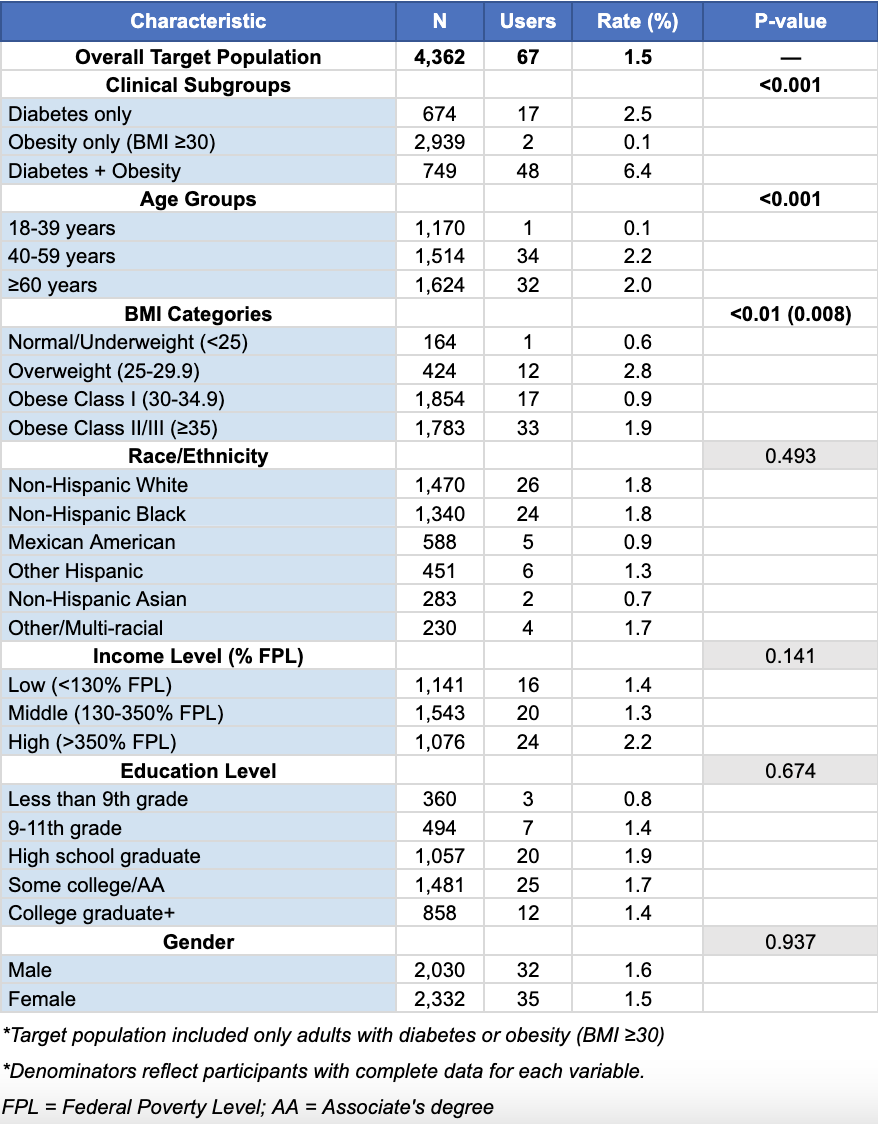
Figure: Table 1. GLP-1 Receptor Agonist Utilization Among Adults with Diabetes and/or Obesity, NHANES 2017-2020
Disclosures:
Tasnin Khan indicated no relevant financial relationships.
Abdallah Beano indicated no relevant financial relationships.
Tasnin Khan, DO, Abdallah Beano, MD. P2697 - GLP-1 Receptor Agonist Utilization: A National Analysis of Access Disparities in US Adults, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
