Monday Poster Session
Category: Esophagus
P2798 - Evaluating Racial and Gender Differences in Barrett’s Esophagus Patients Undergoing Endoscopic Eradication Therapy at an Urban Tertiary Care Center
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- EL
Elizabeth Li, MD (she/her/hers)
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Elizabeth Li, MD1, Benjamin Mauri, MD2, Aditi Simlote, MD3, Abraham Ifrah, MD2, Samyuktha Manikandan, MD2, John Ebeid, MD, MS1, Aanini Dwivedi, MD1, Pranay Adavelly, MD2, Shir Levanon, MD2, Neena Mohan, MD2
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA; 3Temple University Health, Philadelphia, PA
Introduction: Endoscopic eradication therapy (EET), which includes radiofrequency ablation (RFA), cryotherapy, and endoscopic mucosal resection (EMR), is the cornerstone in treatment of dysplastic Barrett’s esophagus (BE) and early esophageal adenocarcinoma (EAC). The effect of race and gender on the outcomes of EET has not been well studied. We aimed to examine differences in demographics, dysplasia status, segment length, and endoscopic therapies in Barrett’s esophagus patients.
Methods: We conducted a retrospective review of 1415 patients diagnosed with BE between January 1, 2013 and December 31, 2022 at our institution that serves a population of 46.1% African American, 29.8% Hispanic, 17.8% Caucasian, 4.1% Asian, and 2.3% other races. There were 234 individuals treated with EET. Data collected included dysplasia classification on index endoscopy as low-grade (LGD), high-grade (HGD), indefinite for dysplasia (IND), and EAC; segment length categorized as short (< 3 cm) or long (>3 cm); and treatment modality (RFA, cryotherapy, EMR, or multiple). Descriptive statistics summarized patient characteristics and treatment trends. Chi-square analysis was performed to assess associations between demographic variables (race, gender) and treatment.
Results: Among patients who underwent EET, the most common dysplasia classification was HGD (22.6%), followed by LGD (21.8%), IND (9.8%) and EAC (7.7%). Of note, 38% of patients who eventually underwent EET had an index EGD showing non-dysplastic Barrett’s esophagus (NDBE). Long segment BE was more prevalent (50.8%) compared to short segment (37.8%) and non-recorded length (11.5%). The most common treatment modality was RFA alone (48.3%), followed by RFA + cryotherapy (18.4%), cryotherapy alone (13.2%), RFA + EMR (6.8%), RFA + cryotherapy + EMR (5.1%), cryotherapy + EMR (4.3%), and EMR alone (3.8%). There was no statistically significant association between dysplasia grade and gender (p=0.21) or race (p=0.71). Furthermore, no significant difference was found in EET type based on gender (p = 0.868) or race (p = 0.959).
Discussion: Our study demonstrates that dysplasia classification rates and EET modality did not differ significantly across gender or racial groups. RFA alone remains the most frequently used EET modality but is also used in addition to cryotherapy or EMR as needed. Further analysis is being performed to assess number of treatments done to achieve complete eradication of intestinal metaplasia (CEIM) and CEIM rates in gender and racial groups.
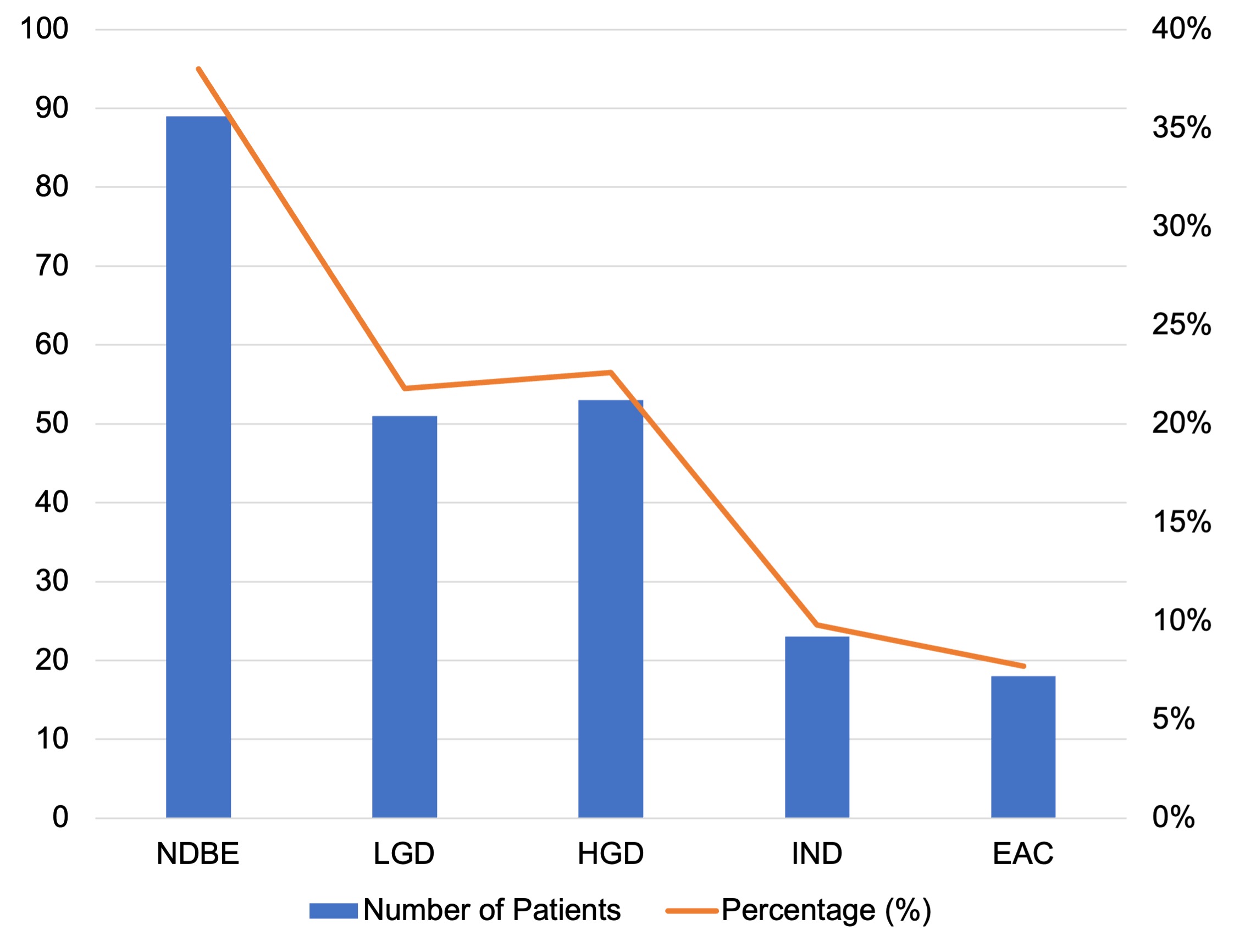
Figure: Dysplasia Classification on Index EGD
Disclosures:
Elizabeth Li indicated no relevant financial relationships.
Benjamin Mauri indicated no relevant financial relationships.
Aditi Simlote indicated no relevant financial relationships.
Abraham Ifrah indicated no relevant financial relationships.
Samyuktha Manikandan indicated no relevant financial relationships.
John Ebeid indicated no relevant financial relationships.
Aanini Dwivedi indicated no relevant financial relationships.
Pranay Adavelly indicated no relevant financial relationships.
Shir Levanon indicated no relevant financial relationships.
Neena Mohan: Cyted – Advisory Committee/Board Member.
Elizabeth Li, MD1, Benjamin Mauri, MD2, Aditi Simlote, MD3, Abraham Ifrah, MD2, Samyuktha Manikandan, MD2, John Ebeid, MD, MS1, Aanini Dwivedi, MD1, Pranay Adavelly, MD2, Shir Levanon, MD2, Neena Mohan, MD2. P2798 - Evaluating Racial and Gender Differences in Barrett’s Esophagus Patients Undergoing Endoscopic Eradication Therapy at an Urban Tertiary Care Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA; 3Temple University Health, Philadelphia, PA
Introduction: Endoscopic eradication therapy (EET), which includes radiofrequency ablation (RFA), cryotherapy, and endoscopic mucosal resection (EMR), is the cornerstone in treatment of dysplastic Barrett’s esophagus (BE) and early esophageal adenocarcinoma (EAC). The effect of race and gender on the outcomes of EET has not been well studied. We aimed to examine differences in demographics, dysplasia status, segment length, and endoscopic therapies in Barrett’s esophagus patients.
Methods: We conducted a retrospective review of 1415 patients diagnosed with BE between January 1, 2013 and December 31, 2022 at our institution that serves a population of 46.1% African American, 29.8% Hispanic, 17.8% Caucasian, 4.1% Asian, and 2.3% other races. There were 234 individuals treated with EET. Data collected included dysplasia classification on index endoscopy as low-grade (LGD), high-grade (HGD), indefinite for dysplasia (IND), and EAC; segment length categorized as short (< 3 cm) or long (>3 cm); and treatment modality (RFA, cryotherapy, EMR, or multiple). Descriptive statistics summarized patient characteristics and treatment trends. Chi-square analysis was performed to assess associations between demographic variables (race, gender) and treatment.
Results: Among patients who underwent EET, the most common dysplasia classification was HGD (22.6%), followed by LGD (21.8%), IND (9.8%) and EAC (7.7%). Of note, 38% of patients who eventually underwent EET had an index EGD showing non-dysplastic Barrett’s esophagus (NDBE). Long segment BE was more prevalent (50.8%) compared to short segment (37.8%) and non-recorded length (11.5%). The most common treatment modality was RFA alone (48.3%), followed by RFA + cryotherapy (18.4%), cryotherapy alone (13.2%), RFA + EMR (6.8%), RFA + cryotherapy + EMR (5.1%), cryotherapy + EMR (4.3%), and EMR alone (3.8%). There was no statistically significant association between dysplasia grade and gender (p=0.21) or race (p=0.71). Furthermore, no significant difference was found in EET type based on gender (p = 0.868) or race (p = 0.959).
Discussion: Our study demonstrates that dysplasia classification rates and EET modality did not differ significantly across gender or racial groups. RFA alone remains the most frequently used EET modality but is also used in addition to cryotherapy or EMR as needed. Further analysis is being performed to assess number of treatments done to achieve complete eradication of intestinal metaplasia (CEIM) and CEIM rates in gender and racial groups.
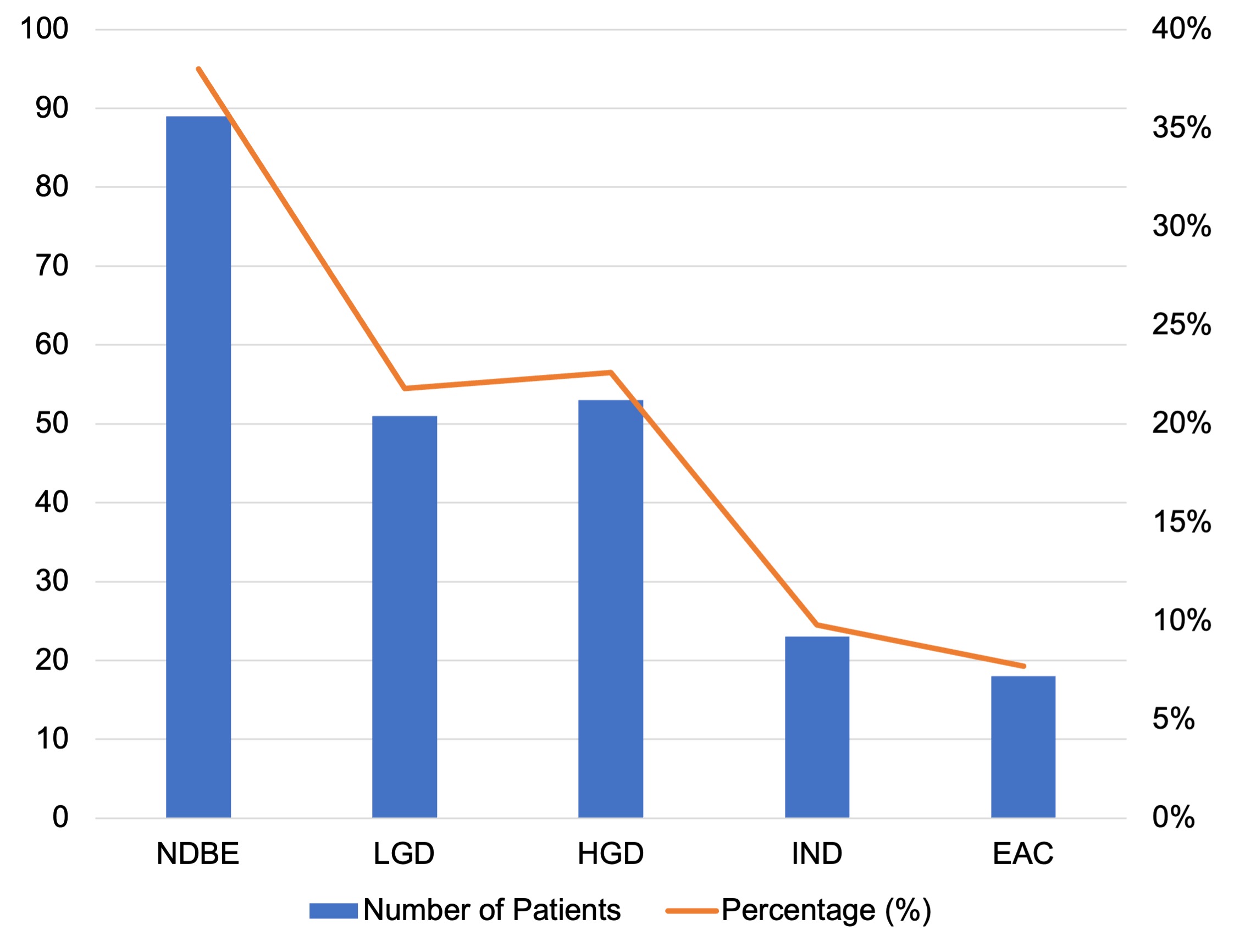
Figure: Dysplasia Classification on Index EGD
Disclosures:
Elizabeth Li indicated no relevant financial relationships.
Benjamin Mauri indicated no relevant financial relationships.
Aditi Simlote indicated no relevant financial relationships.
Abraham Ifrah indicated no relevant financial relationships.
Samyuktha Manikandan indicated no relevant financial relationships.
John Ebeid indicated no relevant financial relationships.
Aanini Dwivedi indicated no relevant financial relationships.
Pranay Adavelly indicated no relevant financial relationships.
Shir Levanon indicated no relevant financial relationships.
Neena Mohan: Cyted – Advisory Committee/Board Member.
Elizabeth Li, MD1, Benjamin Mauri, MD2, Aditi Simlote, MD3, Abraham Ifrah, MD2, Samyuktha Manikandan, MD2, John Ebeid, MD, MS1, Aanini Dwivedi, MD1, Pranay Adavelly, MD2, Shir Levanon, MD2, Neena Mohan, MD2. P2798 - Evaluating Racial and Gender Differences in Barrett’s Esophagus Patients Undergoing Endoscopic Eradication Therapy at an Urban Tertiary Care Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
