Monday Poster Session
Category: Esophagus
P2795 - Ineffective Esophageal Motility and Lung Function Decline in Non-Connective Tissue Disease Interstitial Lung Disease: A Retrospective Cohort Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Tarek Jaber, DO
Medical College of Wisconsin
Milwaukee, WI
Presenting Author(s)
Tarek Jaber, DO1, Thomas Kolman, MS2, Mark Barash, MD2, Francis Edeani, MD2, Mei Ling, MD2, Patrick Sanvanson, MD2, Mark Kern, MD2, Reza Shaker, MD2, Gokulakrishnan Balasubramanian, MD2
1Medical College of Wisconsin, Burr Ridge, IL; 2Medical College of Wisconsin, Milwaukee, WI
Introduction: Esophageal dysmotility has been implicated in the development of microaspiration in patients with Interstitial lung disease (ILD). Although esophageal dysmotility has been studied in patients with connective tissue disorders, there is a paucity of data evaluating it in ILD patients without connective tissue disorders. This study aims to evaluate the impact of esophageal dysmotility in patients with ILD without connective tissue disorders on pulmonary outcomes.
Methods: This is a retrospective study of adult patients at a single academic institution diagnosed with non-connective tissue disease (non-CTD) ILD who underwent esophageal manometry testing between January 1, 2015, and May 30, 2024. Patients with achalasia, nutcracker esophagus, and CTD were excluded. Data from the electronic medical record included demographic information, pulmonary function test (PFT) results, esophageal pH testing results, and esophageal manometry information. Mann-Whitney U testing was used to compare numerical variables with a p-value< 0.05 being considered significant.
Results: Of 57 patients included, 21 (36.8%) were found to have ineffective esophageal motility (IEM). Compared to non-IEM patients, those with IEM demonstrated significantly greater total decline in diffusing capacity for carbon monoxide (DLCO) (24.86% vs. 12.10%, p < 0.03). Total forced vital capacity (FVC) decline was non-significantly higher in the IEM group compared that to non-IEM group (14.63% vs. 11.94%, p = 0.18). The IEM group also demonstrated significantly higher mean SECI than the non-IEM group (270.78 mmHg vs 154.65 mmHg, p-value = 0.024). LES pressure mean was lower in IEM patients (18.73 vs. 22.76 mmHg, p = 0.079), while other esophageal parameters including UES pressure, LES IRP, and EGJ CI showed no significant differences. However, mortality rates were comparable between groups (29.3% vs. 30.0%, p = 0.943).
Discussion: Ineffective esophageal motility is more prevalent in ILD patients without CTD than once realized. Presence of poor esophageal function in this population might have potential implication on worse pulmonary outcomes.
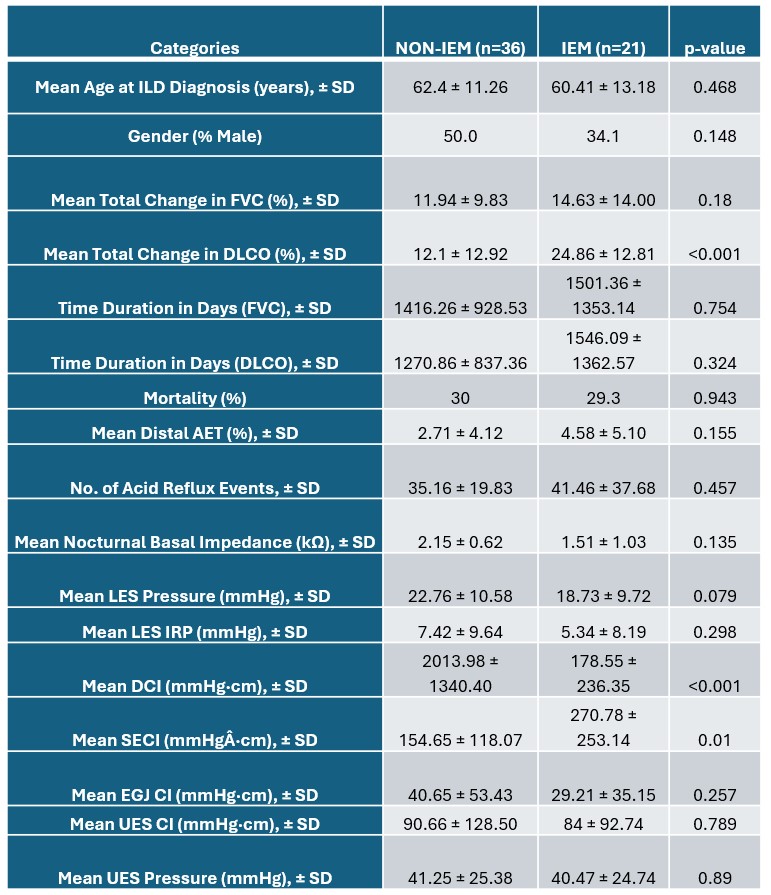
Figure: Patients with non-CTD ILD and ineffective esophageal motility (IEM) demonstrated significantly greater DLCO decline compared to those without IEM, while age, FVC decline, and mortality rates were similar between groups.

Figure: Spearman correlation reveals a significant inverse association between distal esophageal contractile vigor (DCI) and DLCO decline in ILD patients (ρ = –0.397, p = 0.03).
Disclosures:
Tarek Jaber indicated no relevant financial relationships.
Thomas Kolman indicated no relevant financial relationships.
Mark Barash indicated no relevant financial relationships.
Francis Edeani indicated no relevant financial relationships.
Mei Ling indicated no relevant financial relationships.
Patrick Sanvanson indicated no relevant financial relationships.
Mark Kern indicated no relevant financial relationships.
Reza Shaker indicated no relevant financial relationships.
Gokulakrishnan Balasubramanian indicated no relevant financial relationships.
Tarek Jaber, DO1, Thomas Kolman, MS2, Mark Barash, MD2, Francis Edeani, MD2, Mei Ling, MD2, Patrick Sanvanson, MD2, Mark Kern, MD2, Reza Shaker, MD2, Gokulakrishnan Balasubramanian, MD2. P2795 - Ineffective Esophageal Motility and Lung Function Decline in Non-Connective Tissue Disease Interstitial Lung Disease: A Retrospective Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Medical College of Wisconsin, Burr Ridge, IL; 2Medical College of Wisconsin, Milwaukee, WI
Introduction: Esophageal dysmotility has been implicated in the development of microaspiration in patients with Interstitial lung disease (ILD). Although esophageal dysmotility has been studied in patients with connective tissue disorders, there is a paucity of data evaluating it in ILD patients without connective tissue disorders. This study aims to evaluate the impact of esophageal dysmotility in patients with ILD without connective tissue disorders on pulmonary outcomes.
Methods: This is a retrospective study of adult patients at a single academic institution diagnosed with non-connective tissue disease (non-CTD) ILD who underwent esophageal manometry testing between January 1, 2015, and May 30, 2024. Patients with achalasia, nutcracker esophagus, and CTD were excluded. Data from the electronic medical record included demographic information, pulmonary function test (PFT) results, esophageal pH testing results, and esophageal manometry information. Mann-Whitney U testing was used to compare numerical variables with a p-value< 0.05 being considered significant.
Results: Of 57 patients included, 21 (36.8%) were found to have ineffective esophageal motility (IEM). Compared to non-IEM patients, those with IEM demonstrated significantly greater total decline in diffusing capacity for carbon monoxide (DLCO) (24.86% vs. 12.10%, p < 0.03). Total forced vital capacity (FVC) decline was non-significantly higher in the IEM group compared that to non-IEM group (14.63% vs. 11.94%, p = 0.18). The IEM group also demonstrated significantly higher mean SECI than the non-IEM group (270.78 mmHg vs 154.65 mmHg, p-value = 0.024). LES pressure mean was lower in IEM patients (18.73 vs. 22.76 mmHg, p = 0.079), while other esophageal parameters including UES pressure, LES IRP, and EGJ CI showed no significant differences. However, mortality rates were comparable between groups (29.3% vs. 30.0%, p = 0.943).
Discussion: Ineffective esophageal motility is more prevalent in ILD patients without CTD than once realized. Presence of poor esophageal function in this population might have potential implication on worse pulmonary outcomes.
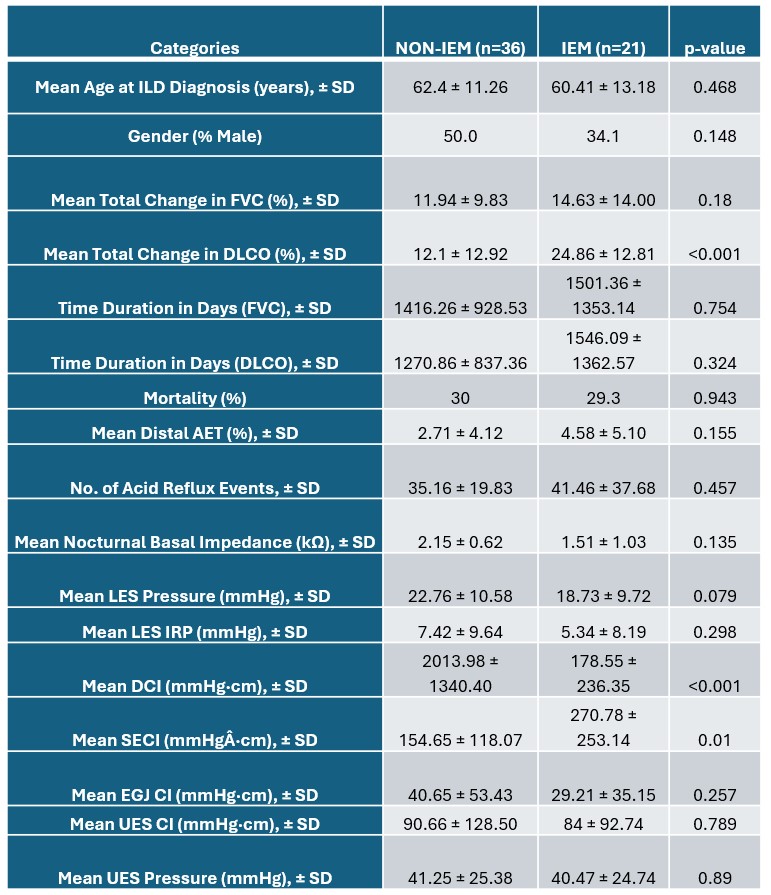
Figure: Patients with non-CTD ILD and ineffective esophageal motility (IEM) demonstrated significantly greater DLCO decline compared to those without IEM, while age, FVC decline, and mortality rates were similar between groups.

Figure: Spearman correlation reveals a significant inverse association between distal esophageal contractile vigor (DCI) and DLCO decline in ILD patients (ρ = –0.397, p = 0.03).
Disclosures:
Tarek Jaber indicated no relevant financial relationships.
Thomas Kolman indicated no relevant financial relationships.
Mark Barash indicated no relevant financial relationships.
Francis Edeani indicated no relevant financial relationships.
Mei Ling indicated no relevant financial relationships.
Patrick Sanvanson indicated no relevant financial relationships.
Mark Kern indicated no relevant financial relationships.
Reza Shaker indicated no relevant financial relationships.
Gokulakrishnan Balasubramanian indicated no relevant financial relationships.
Tarek Jaber, DO1, Thomas Kolman, MS2, Mark Barash, MD2, Francis Edeani, MD2, Mei Ling, MD2, Patrick Sanvanson, MD2, Mark Kern, MD2, Reza Shaker, MD2, Gokulakrishnan Balasubramanian, MD2. P2795 - Ineffective Esophageal Motility and Lung Function Decline in Non-Connective Tissue Disease Interstitial Lung Disease: A Retrospective Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
