Monday Poster Session
Category: Esophagus
P2794 - Impact of Esophageal Dysmotility on Pulmonary Function Decline in Interstitial Lung Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Tarek Jaber, DO
Medical College of Wisconsin
Milwaukee, WI
Presenting Author(s)
Tarek Jaber, DO1, Thomas Kolman, MS2, Mark Barash, MD2, Francis Edeani, MD2, Mei Ling, MD2, Patrick Sanvanson, MD2, Mark Kern, MD2, Reza Shaker, MD2, Gokulakrishnan Balasubramanian, MD2
1Medical College of Wisconsin, Burr Ridge, IL; 2Medical College of Wisconsin, Milwaukee, WI
Introduction: Esophageal dysmotility has been implicated in the development of micro aspiration and progressive lung injury in patients with interstitial lung disease (ILD). While esophageal dysmotility is well characterized in connective tissue disease (CTD), its role in non-CTD ILD is largely unknown. In this study, we evaluate the impact of esophageal dysmotility in symptomatic ILD patients—those with CTD and non-CTD ILD who underwent esophageal manometry and compared their pulmonary function outcomes to asymptomatic ILD patients.
Methods: This retrospective cohort study included three groups of adult ILD patients evaluated at a single academic center between January 1, 2015, and May 30, 2024. Group 1 included asymptomatic non-CTD ILD patients (no esophageal symptoms); Group 2 included symptomatic CTD-ILD patients and Group 3 included symptomatic non-CTD ILD patients, both of whom underwent clinically indicated esophageal manometry. Data on demographics, pulmonary function, esophageal pH, and manometry parameters (only for Group 2 and 3) was collected. Patients with achalasia or hypercontractile esophagus were excluded. All the parameters between the groups were compared by using ANOVA and p-value < 0.05 was considered significant.
Results: Of the 153 ILD patients (70 asymptomatic non-CTD ILD patients, 26 symptomatic CTD-ILD patients, and 57 symptomatic non-CTD ILD patients), asymptomatic non-CTD ILD patients were significantly older at diagnosis compared to other groups (p < .001). Symptomatic ILD patients (Groups 2 and 3) experienced greater mean total FVC decline (11.7% and 14.0%, respectively) compared to the asymptomatic group (7.9%, p = .028), as well as greater DLCO decline (24.8% and 16.3% vs. 8.9%, p < .001). Among those who underwent manometry (Groups 2 and 3), ineffective esophageal motility (IEM) was significantly more prevalent in the CTD group (83.3%) than in the non-CTD group (36.8%, p < .001). Additionally, Group 3 patients had higher DCI values (1348.6 vs. 458.7 mmHg·cm, p = .005), while Group 2 had higher SECI values (332.0 vs. 163.5 mmHg·cm, p < .001).
Discussion: Symptomatic ILD patients (with and without CTD) had a high prevalence of esophageal dysmotility and were associated with greater decline in pulmonary function outcomes. Future prospective studies are needed to further delineate the pathophysiologic mechanisms of esophageal dysmotility.
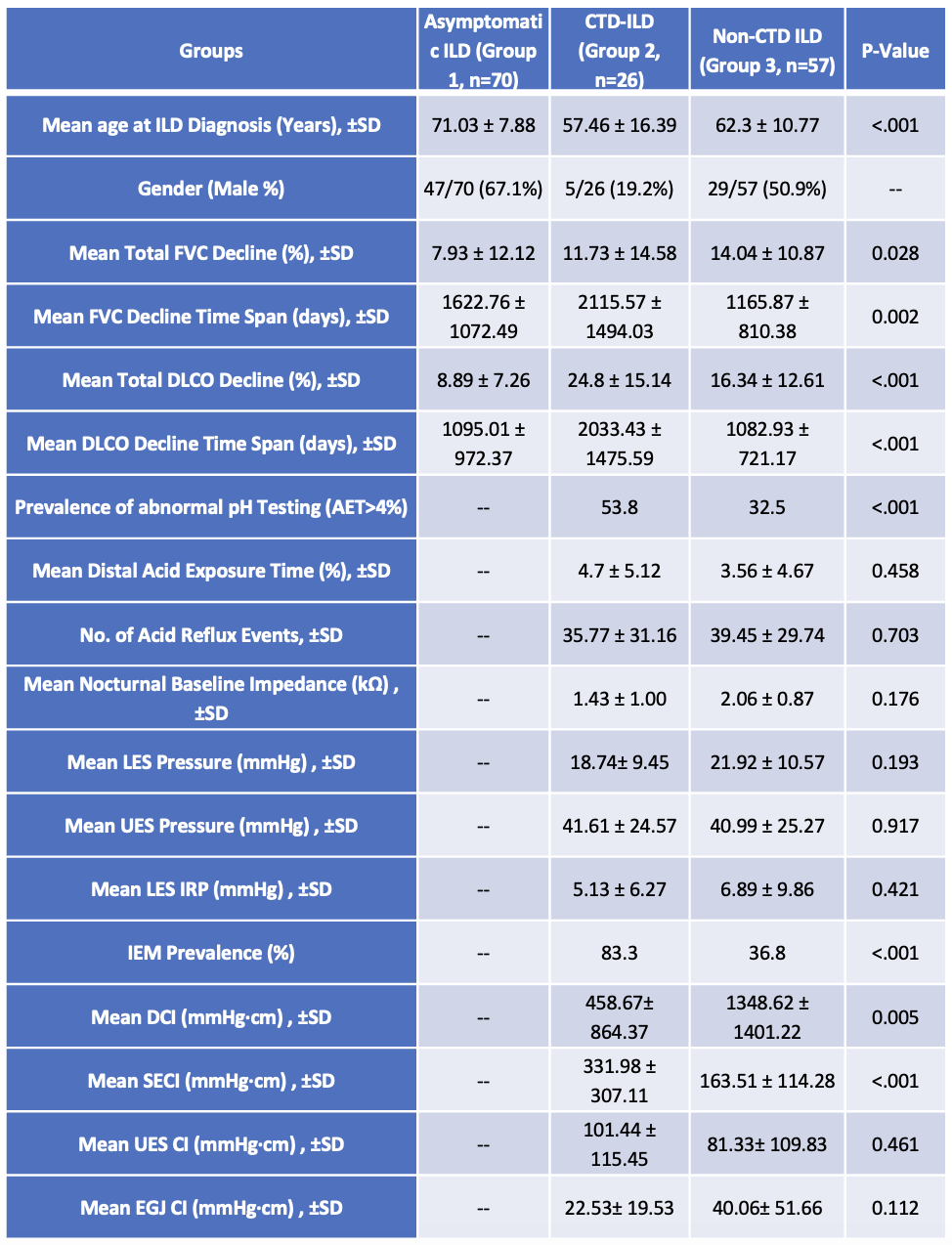
Figure: Table: Esophageal and Pulmonary Characteristics by ILD Group
Mean ± SD values and proportions are shown for key pulmonary, reflux, and esophageal function measures across patients with asymptomatic non-CTD ILD (Group 1), symptomatic CTD-ILD (Group 2), and symptomatic non-CTD ILD (Group 3).
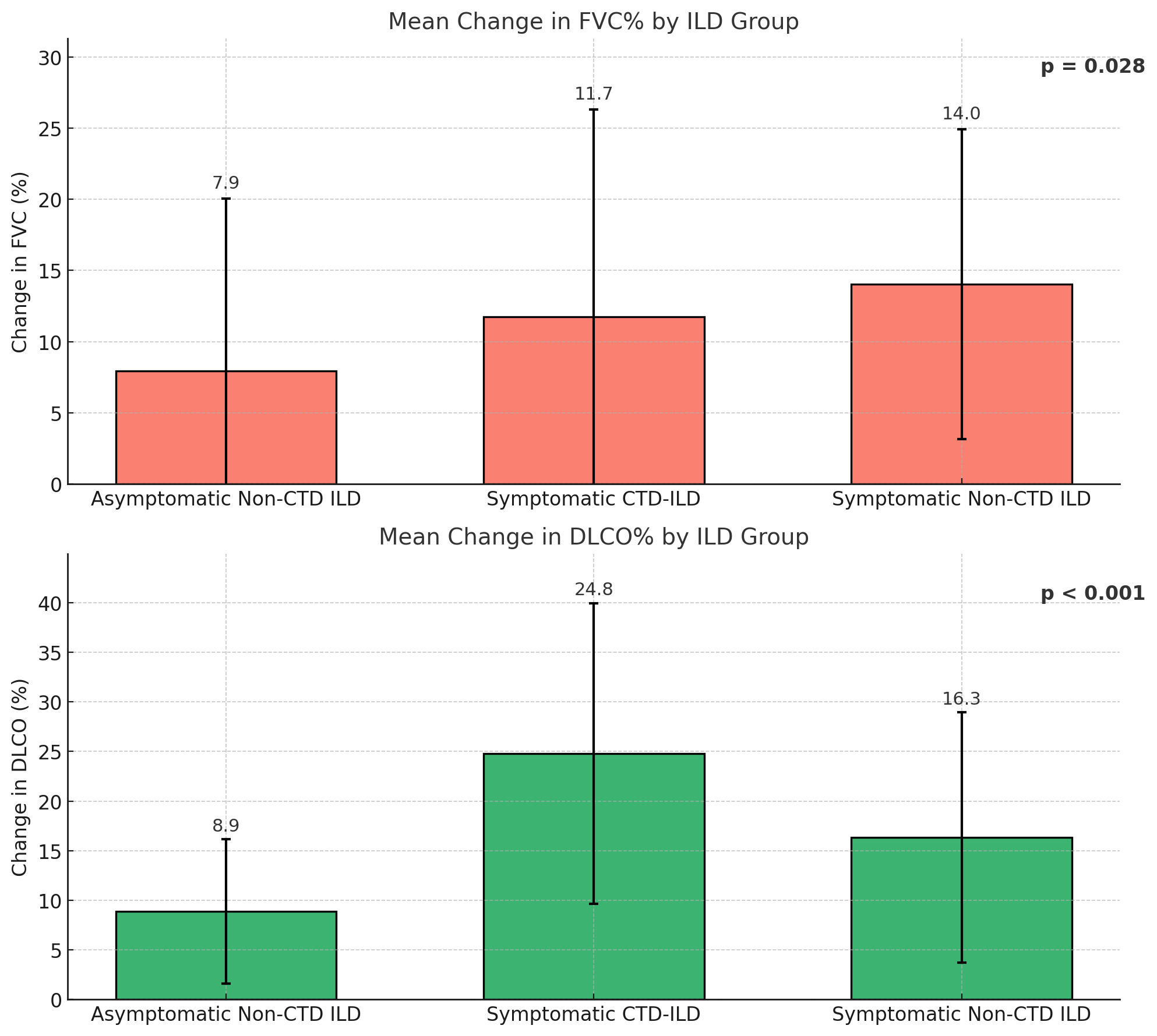
Figure: Figure: Mean Change in FVC% and DLCO%
Bars represent mean total change % ± standard deviation in FVC and DLCO among patients with asymptomatic non-CTD ILD, symptomatic CTD-ILD, and symptomatic non-CTD ILD. P-values reflect overall group differences.
Disclosures:
Tarek Jaber indicated no relevant financial relationships.
Thomas Kolman indicated no relevant financial relationships.
Mark Barash indicated no relevant financial relationships.
Francis Edeani indicated no relevant financial relationships.
Mei Ling indicated no relevant financial relationships.
Patrick Sanvanson indicated no relevant financial relationships.
Mark Kern indicated no relevant financial relationships.
Reza Shaker indicated no relevant financial relationships.
Gokulakrishnan Balasubramanian indicated no relevant financial relationships.
Tarek Jaber, DO1, Thomas Kolman, MS2, Mark Barash, MD2, Francis Edeani, MD2, Mei Ling, MD2, Patrick Sanvanson, MD2, Mark Kern, MD2, Reza Shaker, MD2, Gokulakrishnan Balasubramanian, MD2. P2794 - Impact of Esophageal Dysmotility on Pulmonary Function Decline in Interstitial Lung Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Medical College of Wisconsin, Burr Ridge, IL; 2Medical College of Wisconsin, Milwaukee, WI
Introduction: Esophageal dysmotility has been implicated in the development of micro aspiration and progressive lung injury in patients with interstitial lung disease (ILD). While esophageal dysmotility is well characterized in connective tissue disease (CTD), its role in non-CTD ILD is largely unknown. In this study, we evaluate the impact of esophageal dysmotility in symptomatic ILD patients—those with CTD and non-CTD ILD who underwent esophageal manometry and compared their pulmonary function outcomes to asymptomatic ILD patients.
Methods: This retrospective cohort study included three groups of adult ILD patients evaluated at a single academic center between January 1, 2015, and May 30, 2024. Group 1 included asymptomatic non-CTD ILD patients (no esophageal symptoms); Group 2 included symptomatic CTD-ILD patients and Group 3 included symptomatic non-CTD ILD patients, both of whom underwent clinically indicated esophageal manometry. Data on demographics, pulmonary function, esophageal pH, and manometry parameters (only for Group 2 and 3) was collected. Patients with achalasia or hypercontractile esophagus were excluded. All the parameters between the groups were compared by using ANOVA and p-value < 0.05 was considered significant.
Results: Of the 153 ILD patients (70 asymptomatic non-CTD ILD patients, 26 symptomatic CTD-ILD patients, and 57 symptomatic non-CTD ILD patients), asymptomatic non-CTD ILD patients were significantly older at diagnosis compared to other groups (p < .001). Symptomatic ILD patients (Groups 2 and 3) experienced greater mean total FVC decline (11.7% and 14.0%, respectively) compared to the asymptomatic group (7.9%, p = .028), as well as greater DLCO decline (24.8% and 16.3% vs. 8.9%, p < .001). Among those who underwent manometry (Groups 2 and 3), ineffective esophageal motility (IEM) was significantly more prevalent in the CTD group (83.3%) than in the non-CTD group (36.8%, p < .001). Additionally, Group 3 patients had higher DCI values (1348.6 vs. 458.7 mmHg·cm, p = .005), while Group 2 had higher SECI values (332.0 vs. 163.5 mmHg·cm, p < .001).
Discussion: Symptomatic ILD patients (with and without CTD) had a high prevalence of esophageal dysmotility and were associated with greater decline in pulmonary function outcomes. Future prospective studies are needed to further delineate the pathophysiologic mechanisms of esophageal dysmotility.
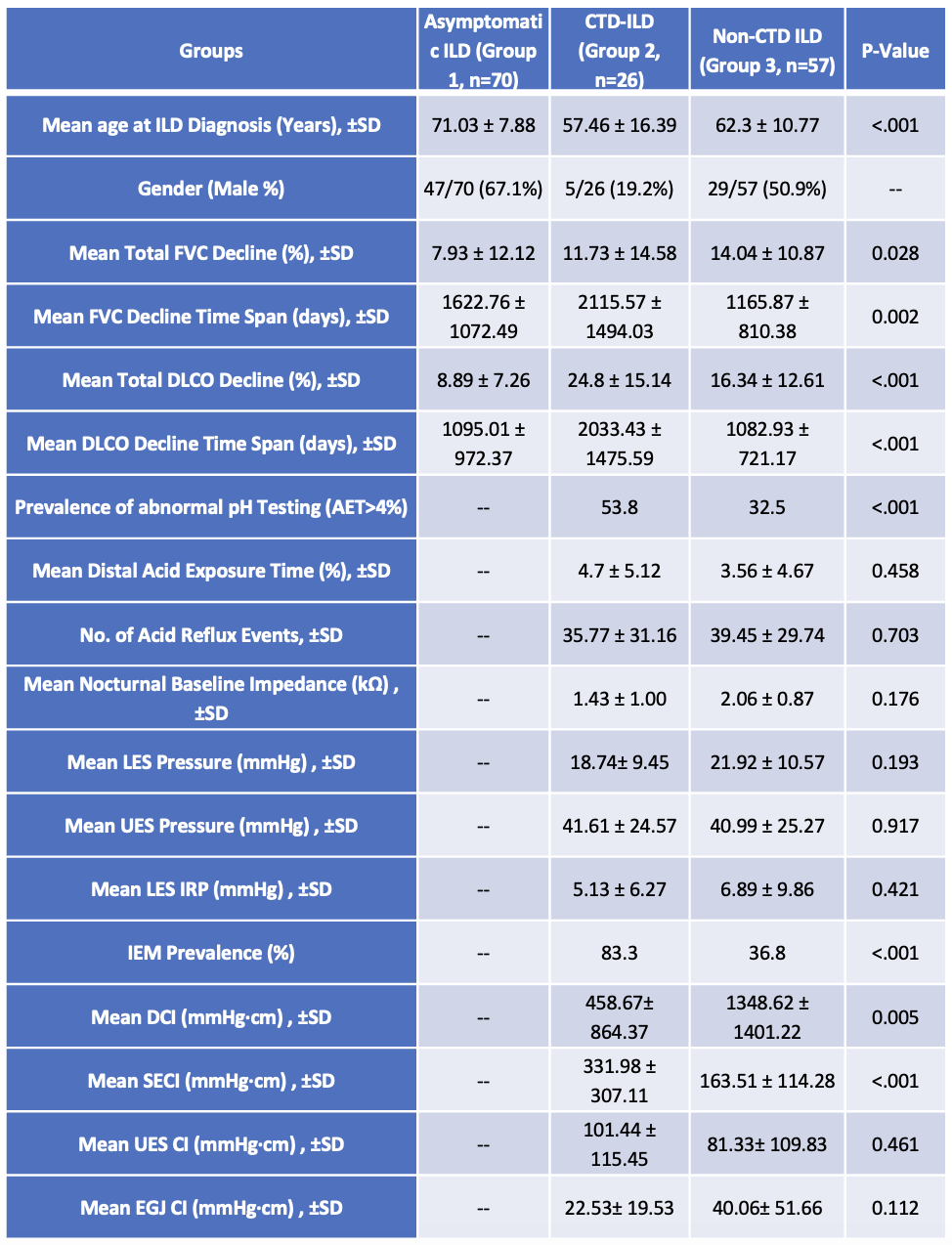
Figure: Table: Esophageal and Pulmonary Characteristics by ILD Group
Mean ± SD values and proportions are shown for key pulmonary, reflux, and esophageal function measures across patients with asymptomatic non-CTD ILD (Group 1), symptomatic CTD-ILD (Group 2), and symptomatic non-CTD ILD (Group 3).
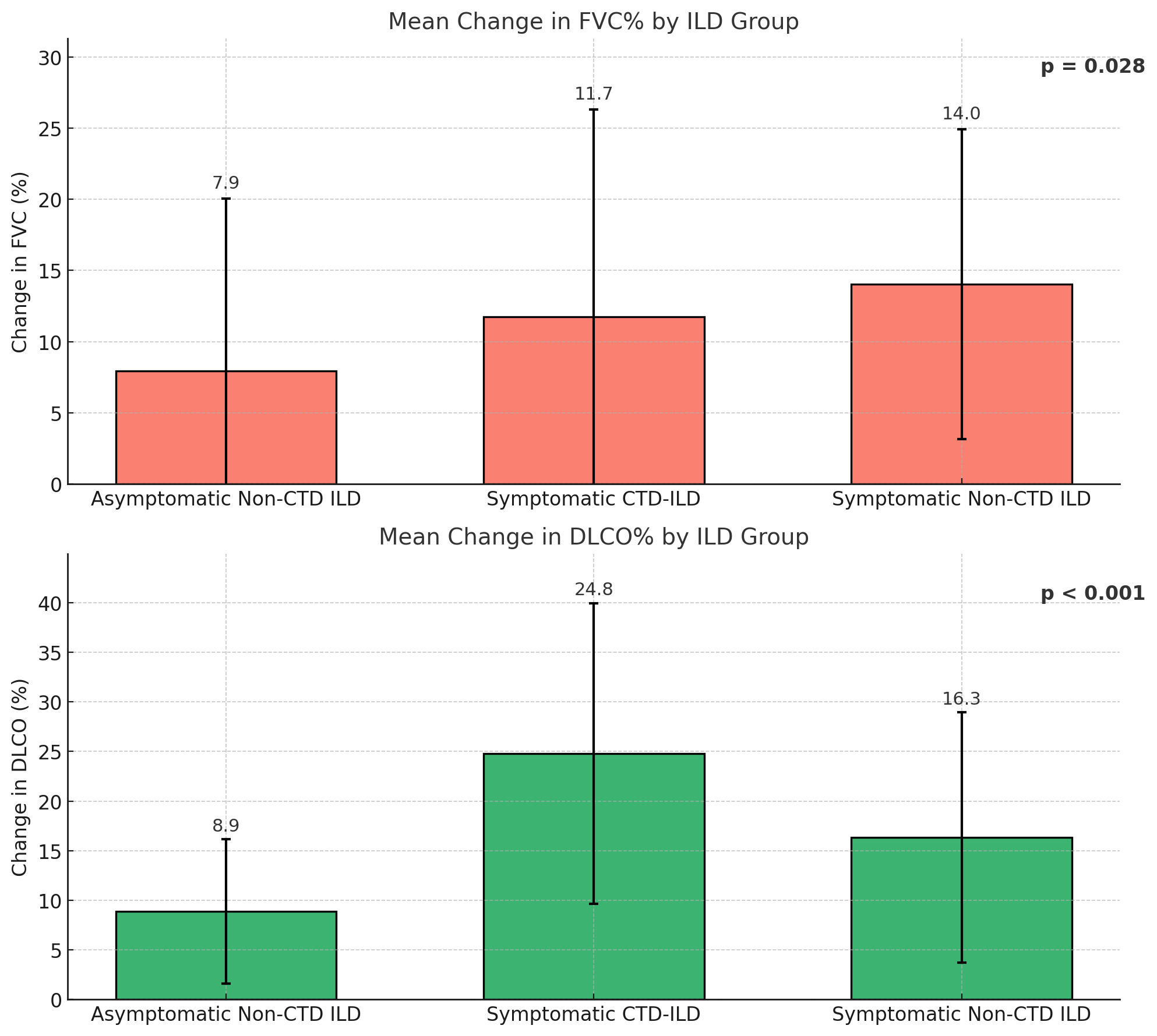
Figure: Figure: Mean Change in FVC% and DLCO%
Bars represent mean total change % ± standard deviation in FVC and DLCO among patients with asymptomatic non-CTD ILD, symptomatic CTD-ILD, and symptomatic non-CTD ILD. P-values reflect overall group differences.
Disclosures:
Tarek Jaber indicated no relevant financial relationships.
Thomas Kolman indicated no relevant financial relationships.
Mark Barash indicated no relevant financial relationships.
Francis Edeani indicated no relevant financial relationships.
Mei Ling indicated no relevant financial relationships.
Patrick Sanvanson indicated no relevant financial relationships.
Mark Kern indicated no relevant financial relationships.
Reza Shaker indicated no relevant financial relationships.
Gokulakrishnan Balasubramanian indicated no relevant financial relationships.
Tarek Jaber, DO1, Thomas Kolman, MS2, Mark Barash, MD2, Francis Edeani, MD2, Mei Ling, MD2, Patrick Sanvanson, MD2, Mark Kern, MD2, Reza Shaker, MD2, Gokulakrishnan Balasubramanian, MD2. P2794 - Impact of Esophageal Dysmotility on Pulmonary Function Decline in Interstitial Lung Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
