Monday Poster Session
Category: Esophagus
P2902 - Down the Gastrointestinal Tract: A Rare Case of Metastatic Esophageal Cancer Spreading to the Colon
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tareq Alsaleh, MD
Department of Internal Medicine, AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Tareq Alsaleh, MD1, Prachi Mann, MD2, Nouman Shafique, MD1, Baha Fawwaz, MD3, Mohamad Khaled Almujarkesh, MD3, Mohammad Asfari, MD3
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Internal Medicine, Adventhealth Orlando, Orlando, FL; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Esophageal adenocarcinoma (EAC) incidence is rising in high-income countries. The most common sites of metastasis are the liver, lymph nodes, and lungs. Our case demonstrates an exceptionally rare instance of colonic metastasis of EAC.
Case Description/
Methods: A 64-year-old male with a past medical history of GERD and squamous cell laryngeal cancer in remission was referred for endoscopic evaluation following the detection of adenocarcinoma lesions in the liver on surveillance imaging. He denied any gastrointestinal symptoms. He did not smoke but consumed 10-20g of alcohol per month. The physical examination was unremarkable.
A recent surveillance computed tomography (CT) scan showed multiple low attenuated liver lesions and esophageal nodularity. A CT-guided biopsy of the liver lesions revealed poorly differentiated adenocarcinoma that stained positive for cytokeratin-7 (CK7), cytokeratin-20 (CK20), and CDX2, suggesting metastasis from an upper GI source.
Esophagogastroduodenoscopy (EGD) revealed multiple fungating masses in the mid and distal esophagus (Figure 1A). On colonoscopy, a fungating, infiltrative, and ulcerating large mass was found in the ascending colon (Figure 1B).
Biopsies from the esophageal and colon masses showed invasive adenocarcinoma (Figure 2). The masses stained positively for CK7, CK20, and CDX2. The colonic mass was also negative for p40 and CK5/6, suggesting that it is a secondary tumor metastasizing from the esophagus.
The patient was then started on oxaliplatin, 5-fluorouracil, trastuzumab and pembrolizumab.
Discussion: EAC has a high metastatic potential and poor prognosis, and it can be asymptomatic in early stages. Secondary neoplastic lesions in the liver are often found in patients with carcinoma of unknown primary (CUP). EGD and colonoscopy are reasonable options for the evaluation of CUP when the clinical picture or histopathology suggests the possibility of a GI source. There are no previously reported cases of EAC resulting in such a large fungating metastatic mass in the colon.
Imaging is a crucial part of evaluation of EAC, as it allows staging and identifies candidates for potential curative surgical therapy. It may still fail to detect colonic metastasis like in our patient. Colonoscopy is not routinely recommended in the evaluation of EAC, but our case underscores its utility as part of a multi-disciplinary approach when standard workup fails. The bulky gross morphology of this colonic mass stresses the serious metastatic potential of EAC.
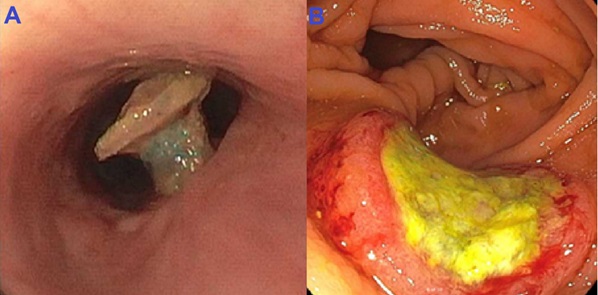
Figure: Figure 1A. Fungating esophageal mass. Figure 1B. Infiltrative and ulcerating large mass in the ascending colon
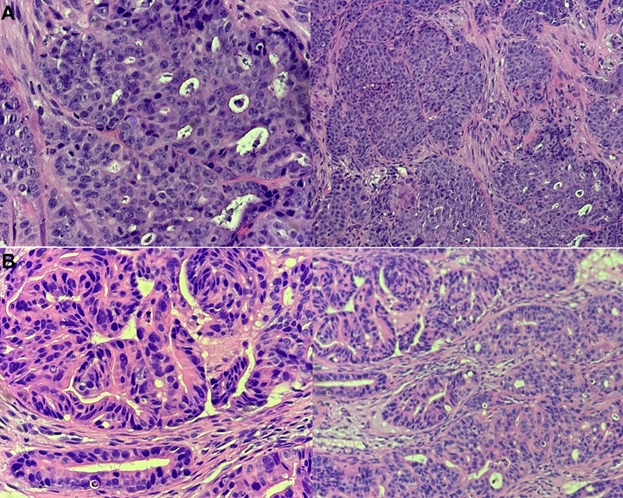
Figure: Figure 2A. Invasive, moderately differentiated adenocarcinoma in the esophagus. Figure 2B. Invasive, poorly differentiated adenocarcinoma in the colon
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Prachi Mann indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Baha Fawwaz indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Mohammad Asfari indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Prachi Mann, MD2, Nouman Shafique, MD1, Baha Fawwaz, MD3, Mohamad Khaled Almujarkesh, MD3, Mohammad Asfari, MD3. P2902 - Down the Gastrointestinal Tract: A Rare Case of Metastatic Esophageal Cancer Spreading to the Colon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Internal Medicine, Adventhealth Orlando, Orlando, FL; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Esophageal adenocarcinoma (EAC) incidence is rising in high-income countries. The most common sites of metastasis are the liver, lymph nodes, and lungs. Our case demonstrates an exceptionally rare instance of colonic metastasis of EAC.
Case Description/
Methods: A 64-year-old male with a past medical history of GERD and squamous cell laryngeal cancer in remission was referred for endoscopic evaluation following the detection of adenocarcinoma lesions in the liver on surveillance imaging. He denied any gastrointestinal symptoms. He did not smoke but consumed 10-20g of alcohol per month. The physical examination was unremarkable.
A recent surveillance computed tomography (CT) scan showed multiple low attenuated liver lesions and esophageal nodularity. A CT-guided biopsy of the liver lesions revealed poorly differentiated adenocarcinoma that stained positive for cytokeratin-7 (CK7), cytokeratin-20 (CK20), and CDX2, suggesting metastasis from an upper GI source.
Esophagogastroduodenoscopy (EGD) revealed multiple fungating masses in the mid and distal esophagus (Figure 1A). On colonoscopy, a fungating, infiltrative, and ulcerating large mass was found in the ascending colon (Figure 1B).
Biopsies from the esophageal and colon masses showed invasive adenocarcinoma (Figure 2). The masses stained positively for CK7, CK20, and CDX2. The colonic mass was also negative for p40 and CK5/6, suggesting that it is a secondary tumor metastasizing from the esophagus.
The patient was then started on oxaliplatin, 5-fluorouracil, trastuzumab and pembrolizumab.
Discussion: EAC has a high metastatic potential and poor prognosis, and it can be asymptomatic in early stages. Secondary neoplastic lesions in the liver are often found in patients with carcinoma of unknown primary (CUP). EGD and colonoscopy are reasonable options for the evaluation of CUP when the clinical picture or histopathology suggests the possibility of a GI source. There are no previously reported cases of EAC resulting in such a large fungating metastatic mass in the colon.
Imaging is a crucial part of evaluation of EAC, as it allows staging and identifies candidates for potential curative surgical therapy. It may still fail to detect colonic metastasis like in our patient. Colonoscopy is not routinely recommended in the evaluation of EAC, but our case underscores its utility as part of a multi-disciplinary approach when standard workup fails. The bulky gross morphology of this colonic mass stresses the serious metastatic potential of EAC.
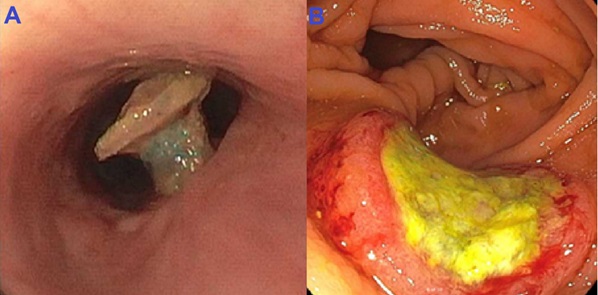
Figure: Figure 1A. Fungating esophageal mass. Figure 1B. Infiltrative and ulcerating large mass in the ascending colon
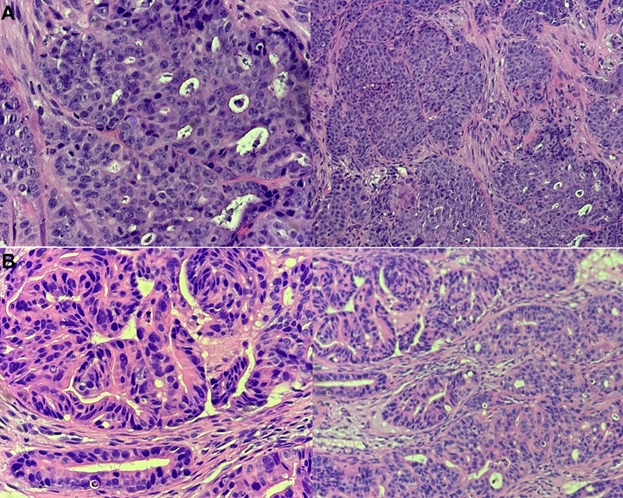
Figure: Figure 2A. Invasive, moderately differentiated adenocarcinoma in the esophagus. Figure 2B. Invasive, poorly differentiated adenocarcinoma in the colon
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Prachi Mann indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Baha Fawwaz indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Mohammad Asfari indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Prachi Mann, MD2, Nouman Shafique, MD1, Baha Fawwaz, MD3, Mohamad Khaled Almujarkesh, MD3, Mohammad Asfari, MD3. P2902 - Down the Gastrointestinal Tract: A Rare Case of Metastatic Esophageal Cancer Spreading to the Colon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
