Monday Poster Session
Category: Esophagus
P2898 - A Swallowing Crisis: Dysphagia as a Reversible Manifestation of Paroxysmal Nocturnal Hemoglobinuria Flares
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Alsiddig Elmahdi, MD
Virginia Commonwealth University Health System
Leesburg, VA
Presenting Author(s)
Alsiddig Elmahdi, MD1, Vinay Jahagirdar, MD2, Anas Aljabi, MD1, Brian Davis, MD3
1Virginia Commonwealth University Health System, Richmond, VA; 2Virginia Commonwealth University Medical Center, Richmond, VA; 3Medical Director of Liver Transplantation, Hunter Holmes McGuire VA Medical Center, Richmond, VA
Introduction: Paroxysmal Nocturnal Hemoglobinuria (PNH) is a rare hematologic disorder characterized by complement-mediated hemolysis and thrombosis. It can also be associated with gastrointestinal symptoms such as dysphagia. This occurs due to hemolysis release of free hemoglobin into the plasma from hemolysis, causing local and systemic nitric oxide depletion. The resulting unopposed smooth muscle contraction causes esophageal spasms and decreased relaxation of the lower esophageal sphincter.
Up to 23% of patients with PNH may have dysphagia. Despite this, there have been few documented cases of dysphagia in this population, and many clinicians fail to recognize it as a common symptom. Here, we demonstrate a classic case of dysphagia in a PNH patient.
Case Description/
Methods: A 77-year-old male with a history of PNH (hemolytic-classic type) presented with a week of dark urine with associated epigastric pain. Admission labs include: Bilirubin 3.4 mg/dL, Creatinine 1.3 mg/dL, Hgb 8.1 g/dL, platelets of 151 g/dL, LDH of 1,073 U/L and a haptoglobin of less than 8 mg/dL. Patient reported worsening solid-food dysphagia and noted that his PNH flares were associated with dysphagia. He was unable to tolerate any PO intake in days prior to presentation. Barium esophagram was performed which demonstrated mild narrowing of the distal esophagus, but the barium tablet was able to easily traverse the GEJ, ruling out a mechanical cause for the dysphagia. A recent EGD, done 1- year prior, was unremarkable.
Hematology and nephrology were consulted, as the patient went on to develop worsening hemolysis and acute renal failure from his PNH. The patient was urgently started on weekly IV eculizumab. Four days after receiving the first dose, the patient started to show clinical and laboratory improvement (LDH down to 771, haptoglobin up to 60). Patient also noted resolution of dysphagia symptoms, and was able to tolerate a regular diet.
Discussion: This case highlights dysphagia as an under-recognized but reversible complication of PNH. Prompt recognition and initiation of complement inhibition with eculizumab not only improves hematologic parameters but can also resolve associated gastrointestinal symptoms, supporting the mechanistic link between hemolysis, nitric oxide depletion, and smooth muscle dystonia in PNH.
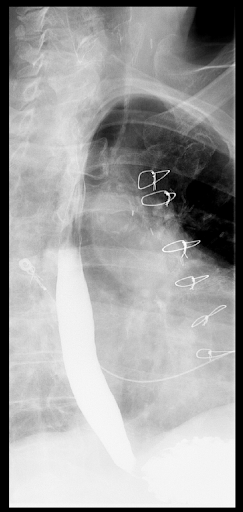
Figure: Barium Esophagram without any gross abnormalities, with free passage of contrast via gastroesophageal junction

Figure: Pertinent laboratory values at day zero (prior to initiating Eculizumab) and day five (four days after initiation)
Disclosures:
Alsiddig Elmahdi indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Anas Aljabi indicated no relevant financial relationships.
Brian Davis indicated no relevant financial relationships.
Alsiddig Elmahdi, MD1, Vinay Jahagirdar, MD2, Anas Aljabi, MD1, Brian Davis, MD3. P2898 - A Swallowing Crisis: Dysphagia as a Reversible Manifestation of Paroxysmal Nocturnal Hemoglobinuria Flares, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Virginia Commonwealth University Health System, Richmond, VA; 2Virginia Commonwealth University Medical Center, Richmond, VA; 3Medical Director of Liver Transplantation, Hunter Holmes McGuire VA Medical Center, Richmond, VA
Introduction: Paroxysmal Nocturnal Hemoglobinuria (PNH) is a rare hematologic disorder characterized by complement-mediated hemolysis and thrombosis. It can also be associated with gastrointestinal symptoms such as dysphagia. This occurs due to hemolysis release of free hemoglobin into the plasma from hemolysis, causing local and systemic nitric oxide depletion. The resulting unopposed smooth muscle contraction causes esophageal spasms and decreased relaxation of the lower esophageal sphincter.
Up to 23% of patients with PNH may have dysphagia. Despite this, there have been few documented cases of dysphagia in this population, and many clinicians fail to recognize it as a common symptom. Here, we demonstrate a classic case of dysphagia in a PNH patient.
Case Description/
Methods: A 77-year-old male with a history of PNH (hemolytic-classic type) presented with a week of dark urine with associated epigastric pain. Admission labs include: Bilirubin 3.4 mg/dL, Creatinine 1.3 mg/dL, Hgb 8.1 g/dL, platelets of 151 g/dL, LDH of 1,073 U/L and a haptoglobin of less than 8 mg/dL. Patient reported worsening solid-food dysphagia and noted that his PNH flares were associated with dysphagia. He was unable to tolerate any PO intake in days prior to presentation. Barium esophagram was performed which demonstrated mild narrowing of the distal esophagus, but the barium tablet was able to easily traverse the GEJ, ruling out a mechanical cause for the dysphagia. A recent EGD, done 1- year prior, was unremarkable.
Hematology and nephrology were consulted, as the patient went on to develop worsening hemolysis and acute renal failure from his PNH. The patient was urgently started on weekly IV eculizumab. Four days after receiving the first dose, the patient started to show clinical and laboratory improvement (LDH down to 771, haptoglobin up to 60). Patient also noted resolution of dysphagia symptoms, and was able to tolerate a regular diet.
Discussion: This case highlights dysphagia as an under-recognized but reversible complication of PNH. Prompt recognition and initiation of complement inhibition with eculizumab not only improves hematologic parameters but can also resolve associated gastrointestinal symptoms, supporting the mechanistic link between hemolysis, nitric oxide depletion, and smooth muscle dystonia in PNH.
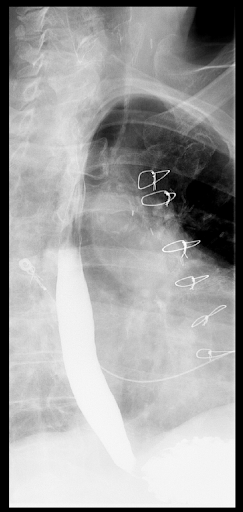
Figure: Barium Esophagram without any gross abnormalities, with free passage of contrast via gastroesophageal junction

Figure: Pertinent laboratory values at day zero (prior to initiating Eculizumab) and day five (four days after initiation)
Disclosures:
Alsiddig Elmahdi indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Anas Aljabi indicated no relevant financial relationships.
Brian Davis indicated no relevant financial relationships.
Alsiddig Elmahdi, MD1, Vinay Jahagirdar, MD2, Anas Aljabi, MD1, Brian Davis, MD3. P2898 - A Swallowing Crisis: Dysphagia as a Reversible Manifestation of Paroxysmal Nocturnal Hemoglobinuria Flares, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
