Monday Poster Session
Category: Esophagus
P2897 - Precision Over Protocol: Endoscopic Wireless pH Placement Tailored to Esophageal Diverticular Anatomy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Benjamin Gow-Lee, MD (he/him/his)
University of Utah School of Medicine
Salt Lake City, UT
Presenting Author(s)
Award: ACG Presidential Poster Award
Benjamin Gow-Lee, MD1, Mina Awadallah, MD, MSc2, John Fang, MD2, John Erikson Yap, MD, MBA, FACG3
1University of Utah School of Medicine, Salt Lake City, UT; 2University of Utah, Salt Lake City, UT; 3University of Utah Health, Salt Lake City, UT
Introduction: Wireless pH monitoring systems are a widely used diagnostic tool for assessing gastroesophageal reflux disease (GERD), typically deployed approximately 6 cm above the gastroesophageal junction (GEJ) without direct visualization. However, in patients with structural abnormalities such as esophageal diverticula, this standard approach may result in technical challenges, including dislodgment or improper placement. This case highlights the importance of individualized technique when conventional placement is not feasible due to altered anatomy.
Case Description/
Methods: A 67-year-old man with hypertension presented with progressive dysphagia. As part of his dysphagia workup and in consideration of a possible pre-POEM (peroral endoscopic myotomy) evaluation, a Bravo pH study was planned to assess for underlying reflux disease. A Bravo study was initially attempted, but the capsule was dislodged shortly after the procedure, likely due to a forceful cough and suboptimal positioning. Further review revealed a diverticulum in the distal esophagus located approximately 6 cm proximal to the GEJ—the standard location for Bravo pH capsule placement—raising concern that the altered wall anatomy contributed to the failed attachment.
A repeat upper endoscopy was performed, and given the anatomic challenge, a decision was made to deploy the Bravo capsule under direct endoscopic visualization. The diverticulum was clearly identified at the typical deployment site, and an alternate location was carefully selected on the opposite side of the diverticulum to avoid complications. The capsule was successfully affixed, and the patient experienced no further issues.
Discussion: Standard wireless pH monitoring relies on blind deployment using anatomic landmarks, but such techniques may be inadequate in patients with esophageal anomalies. In this case, a distal esophageal diverticulum overlapped the typical deployment zone, necessitating a modified approach. Direct visualization allowed precise identification of the diverticulum and safe wireless pH capsule placement on unaffected mucosa. This case demonstrates the value of tailoring procedural strategies based on individual anatomy and supports the use of endoscopic visualization when structural abnormalities increase the risk of failure or complications with traditional techniques.
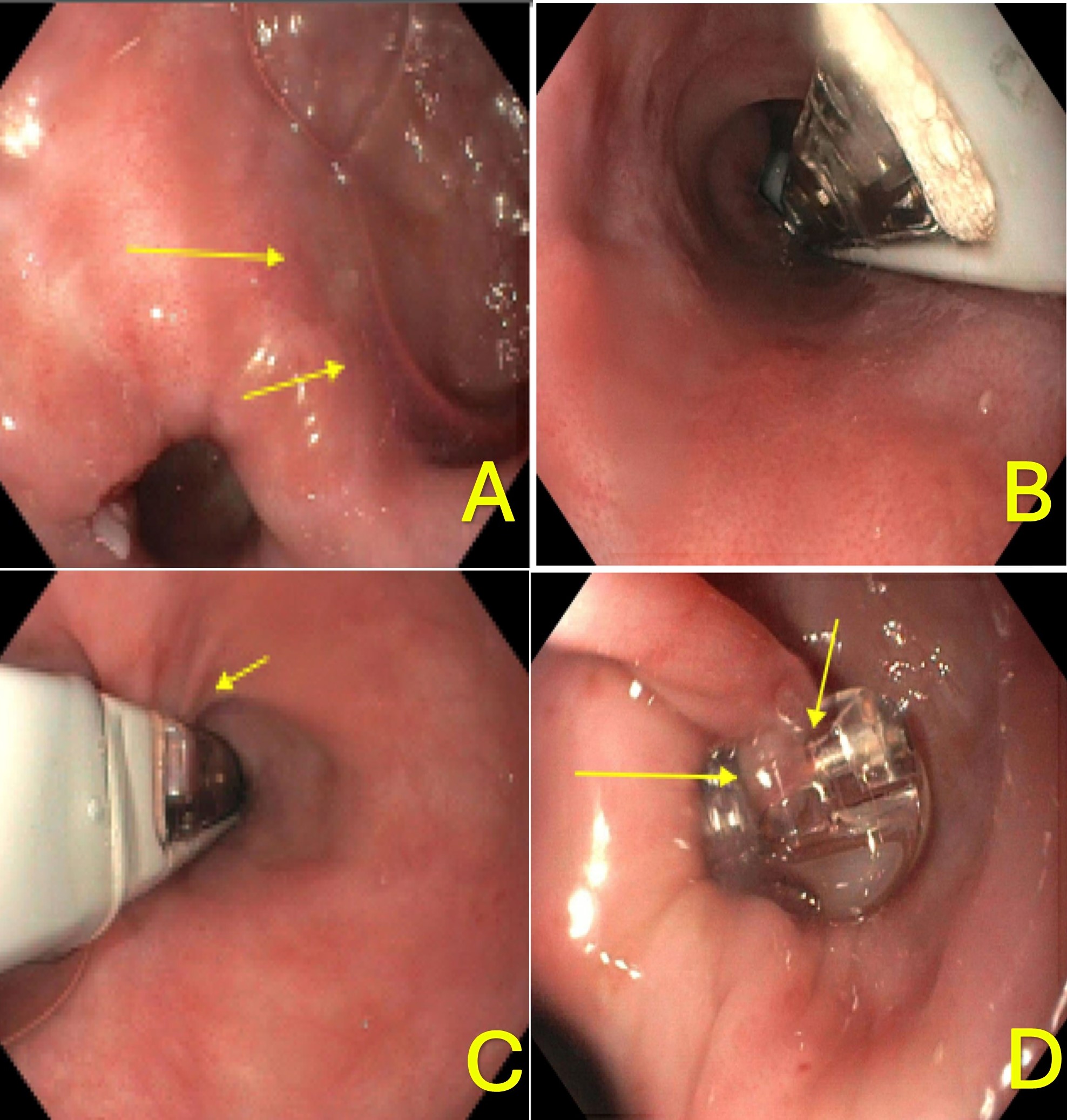
Figure: A. Esophageal diverticulum identified (yellow arrows). B. Endoscopic visualization confirming safe deployment site opposite the diverticulum. C. Suction initiated for wireless pH capsule placement. D. Successful deployment of the pH capsule opposite the diverticulum.
Disclosures:
Benjamin Gow-Lee indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
John Fang: Aspero Medical – Consultant. Circa Scientific – Consultant. Merit – Consultant.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Benjamin Gow-Lee, MD1, Mina Awadallah, MD, MSc2, John Fang, MD2, John Erikson Yap, MD, MBA, FACG3. P2897 - Precision Over Protocol: Endoscopic Wireless pH Placement Tailored to Esophageal Diverticular Anatomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Benjamin Gow-Lee, MD1, Mina Awadallah, MD, MSc2, John Fang, MD2, John Erikson Yap, MD, MBA, FACG3
1University of Utah School of Medicine, Salt Lake City, UT; 2University of Utah, Salt Lake City, UT; 3University of Utah Health, Salt Lake City, UT
Introduction: Wireless pH monitoring systems are a widely used diagnostic tool for assessing gastroesophageal reflux disease (GERD), typically deployed approximately 6 cm above the gastroesophageal junction (GEJ) without direct visualization. However, in patients with structural abnormalities such as esophageal diverticula, this standard approach may result in technical challenges, including dislodgment or improper placement. This case highlights the importance of individualized technique when conventional placement is not feasible due to altered anatomy.
Case Description/
Methods: A 67-year-old man with hypertension presented with progressive dysphagia. As part of his dysphagia workup and in consideration of a possible pre-POEM (peroral endoscopic myotomy) evaluation, a Bravo pH study was planned to assess for underlying reflux disease. A Bravo study was initially attempted, but the capsule was dislodged shortly after the procedure, likely due to a forceful cough and suboptimal positioning. Further review revealed a diverticulum in the distal esophagus located approximately 6 cm proximal to the GEJ—the standard location for Bravo pH capsule placement—raising concern that the altered wall anatomy contributed to the failed attachment.
A repeat upper endoscopy was performed, and given the anatomic challenge, a decision was made to deploy the Bravo capsule under direct endoscopic visualization. The diverticulum was clearly identified at the typical deployment site, and an alternate location was carefully selected on the opposite side of the diverticulum to avoid complications. The capsule was successfully affixed, and the patient experienced no further issues.
Discussion: Standard wireless pH monitoring relies on blind deployment using anatomic landmarks, but such techniques may be inadequate in patients with esophageal anomalies. In this case, a distal esophageal diverticulum overlapped the typical deployment zone, necessitating a modified approach. Direct visualization allowed precise identification of the diverticulum and safe wireless pH capsule placement on unaffected mucosa. This case demonstrates the value of tailoring procedural strategies based on individual anatomy and supports the use of endoscopic visualization when structural abnormalities increase the risk of failure or complications with traditional techniques.
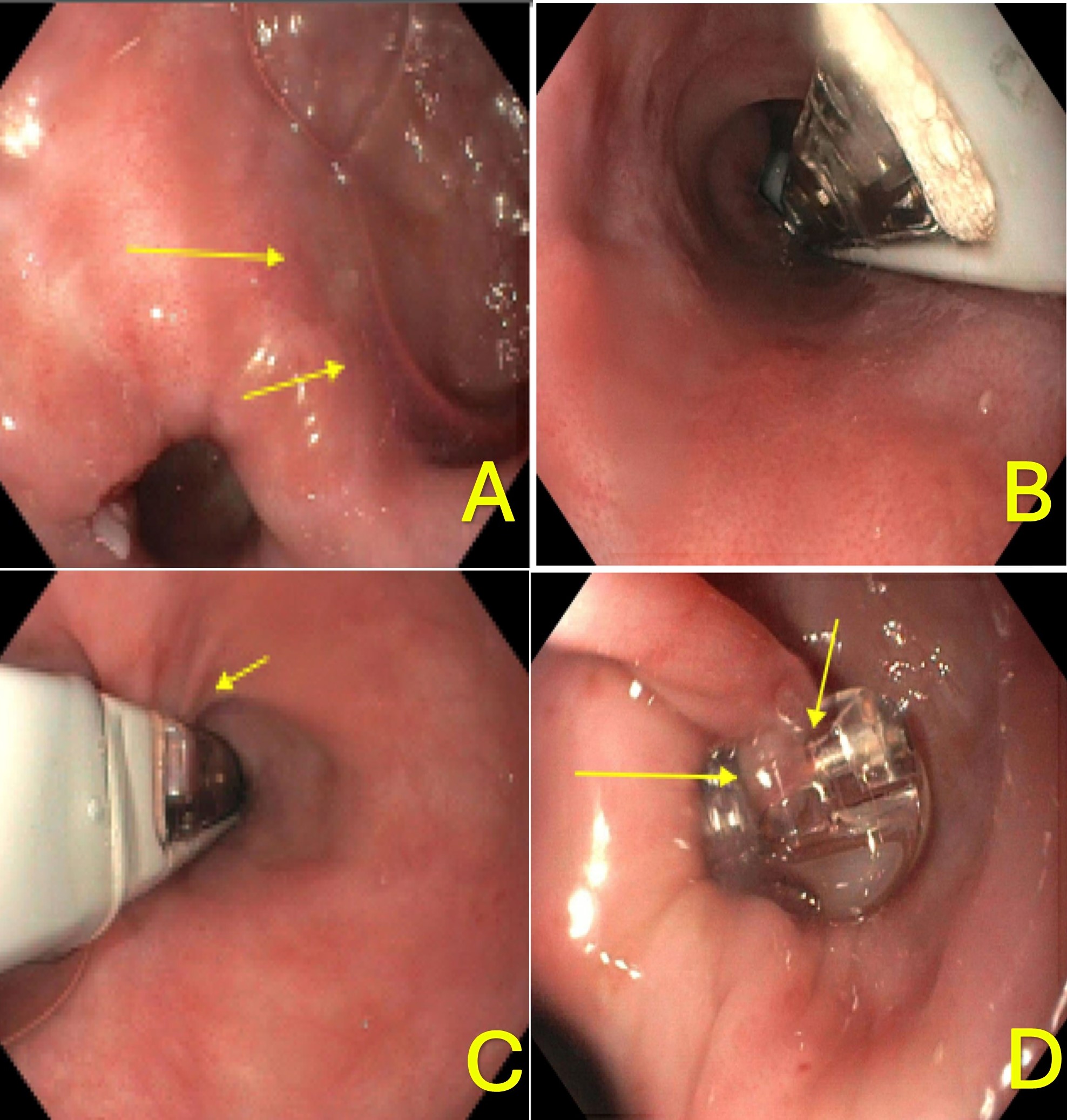
Figure: A. Esophageal diverticulum identified (yellow arrows). B. Endoscopic visualization confirming safe deployment site opposite the diverticulum. C. Suction initiated for wireless pH capsule placement. D. Successful deployment of the pH capsule opposite the diverticulum.
Disclosures:
Benjamin Gow-Lee indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
John Fang: Aspero Medical – Consultant. Circa Scientific – Consultant. Merit – Consultant.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Benjamin Gow-Lee, MD1, Mina Awadallah, MD, MSc2, John Fang, MD2, John Erikson Yap, MD, MBA, FACG3. P2897 - Precision Over Protocol: Endoscopic Wireless pH Placement Tailored to Esophageal Diverticular Anatomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

