Monday Poster Session
Category: Esophagus
P2892 - Acute Esophageal Necrosis: A Rare and Life-Threatening Cause of Acute Gastrointestinal Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Avneet Kaur, MBBS (she/her/hers)
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Avneet Kaur, MBBS, Sharifeh Almasaid, MD, MPH, Abdelkader Chaar, MD, Idan Goren, MD
SUNY Upstate Medical University, Syracuse, NY
Introduction: Acute esophageal necrosis (AEN), or “black esophagus,” is a rare, life-threatening cause of upper gastrointestinal bleeding, characterized by circumferential black mucosa typically involving the distal esophagus. It is frequently associated with systemic shock, severe acid reflux, and mucosal ischemia, which compromise esophageal perfusion. The two-hit hypothesis explains the pathogenesis, in which chronic comorbidities such as diabetes and alcohol use predispose to esophageal hypoperfusion and mucosal barrier loss, followed by an acute insult like shock that leads to severe ischemic and acid-mediated injury.
Case Description/
Methods: A 51-year-old male with diabetes mellitus and alcohol use disorder, recently consuming ~1 liter of vodka daily, presented with dyspnea and diaphoresis. He was found to be in shock requiring vasopressor support and intubation for encephalopathy. Post-intubation, moderate bloody output via his enteric tube prompted GI consultation. Labs revealed hemoglobin of 10.5 g/dL (baseline ~15), hyponatremia, hypokalemia, metabolic acidosis, elevated lipase, and lactic acidosis. CT imaging showed no active bleeding or signs of advanced liver disease. Upper endoscopy demonstrated extensive circumferential black necrotic mucosa, characteristic of AEN, extending from 20 cm from the incisors to the gastroesophageal junction with a sharp transition to normal tissue (Figure 1). He was kept NPO and treated with IV pantoprazole. After extubation, sucralfate was added as diet resumed. Repeat endoscopy two weeks later showed resolving esophagitis with no active bleeding. He was discharged to a rehabilitation facility.
Discussion: This case illustrates a typical presentation of AEN in the setting of alcohol use, metabolic derangement, and shock. AEN should be suspected in critically ill patients with upper GI bleeding and relevant risk factors. Prompt endoscopic evaluation, aggressive supportive care, and a multidisciplinary approach are essential to optimize outcomes and minimize complications such as stricture formation.
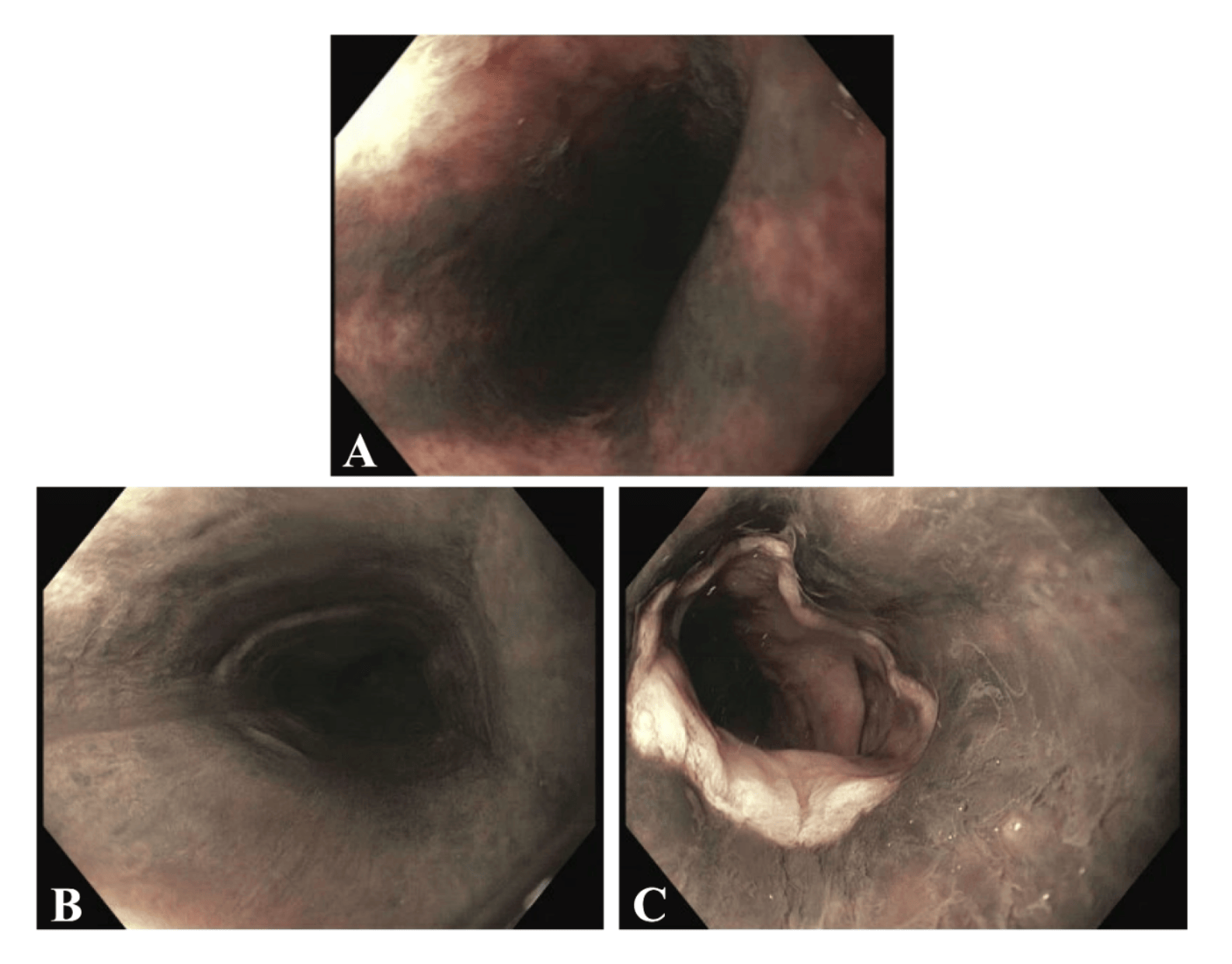
Figure: Figure 1: Initial upper endoscopy showing acute necrotizing esophagitis. A- Upper esophagus. B- Middle esophagus. C- Lower esophagus with sharp transition at the GE junction to normal appearing mucosa distally.
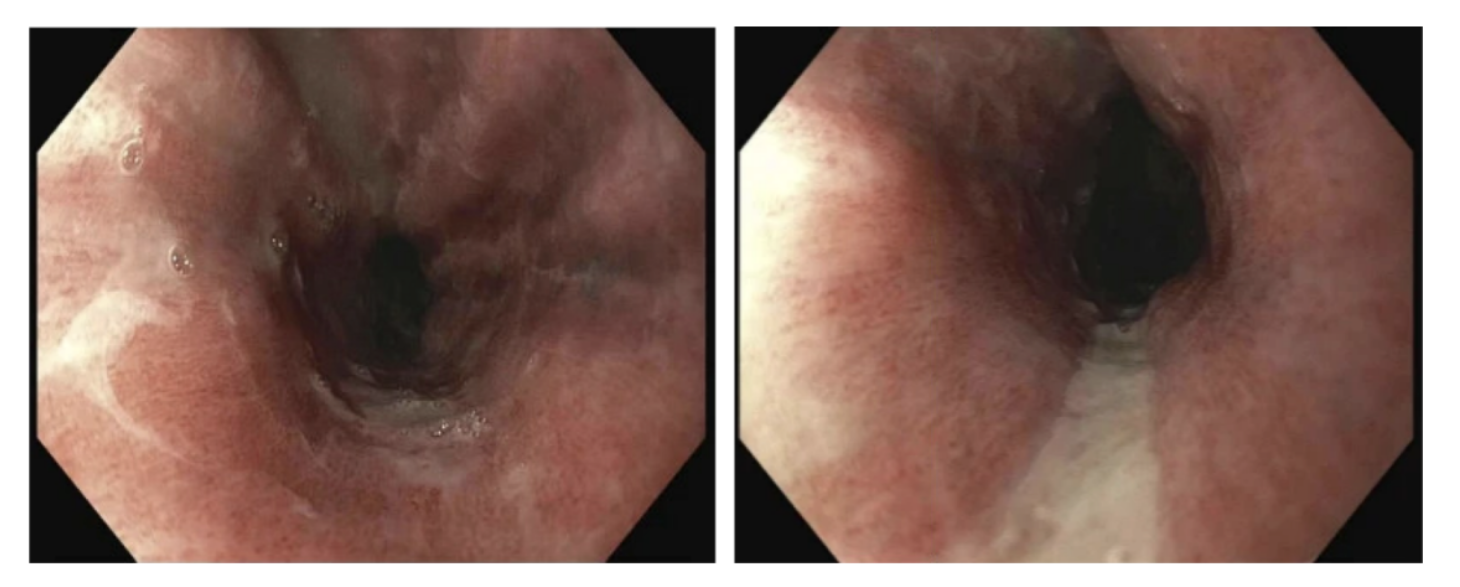
Figure: Figure 2: Follow up upper endoscopy after 2 weeks showing improved mucosa
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Sharifeh Almasaid indicated no relevant financial relationships.
Abdelkader Chaar indicated no relevant financial relationships.
Idan Goren indicated no relevant financial relationships.
Avneet Kaur, MBBS, Sharifeh Almasaid, MD, MPH, Abdelkader Chaar, MD, Idan Goren, MD. P2892 - Acute Esophageal Necrosis: A Rare and Life-Threatening Cause of Acute Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
SUNY Upstate Medical University, Syracuse, NY
Introduction: Acute esophageal necrosis (AEN), or “black esophagus,” is a rare, life-threatening cause of upper gastrointestinal bleeding, characterized by circumferential black mucosa typically involving the distal esophagus. It is frequently associated with systemic shock, severe acid reflux, and mucosal ischemia, which compromise esophageal perfusion. The two-hit hypothesis explains the pathogenesis, in which chronic comorbidities such as diabetes and alcohol use predispose to esophageal hypoperfusion and mucosal barrier loss, followed by an acute insult like shock that leads to severe ischemic and acid-mediated injury.
Case Description/
Methods: A 51-year-old male with diabetes mellitus and alcohol use disorder, recently consuming ~1 liter of vodka daily, presented with dyspnea and diaphoresis. He was found to be in shock requiring vasopressor support and intubation for encephalopathy. Post-intubation, moderate bloody output via his enteric tube prompted GI consultation. Labs revealed hemoglobin of 10.5 g/dL (baseline ~15), hyponatremia, hypokalemia, metabolic acidosis, elevated lipase, and lactic acidosis. CT imaging showed no active bleeding or signs of advanced liver disease. Upper endoscopy demonstrated extensive circumferential black necrotic mucosa, characteristic of AEN, extending from 20 cm from the incisors to the gastroesophageal junction with a sharp transition to normal tissue (Figure 1). He was kept NPO and treated with IV pantoprazole. After extubation, sucralfate was added as diet resumed. Repeat endoscopy two weeks later showed resolving esophagitis with no active bleeding. He was discharged to a rehabilitation facility.
Discussion: This case illustrates a typical presentation of AEN in the setting of alcohol use, metabolic derangement, and shock. AEN should be suspected in critically ill patients with upper GI bleeding and relevant risk factors. Prompt endoscopic evaluation, aggressive supportive care, and a multidisciplinary approach are essential to optimize outcomes and minimize complications such as stricture formation.
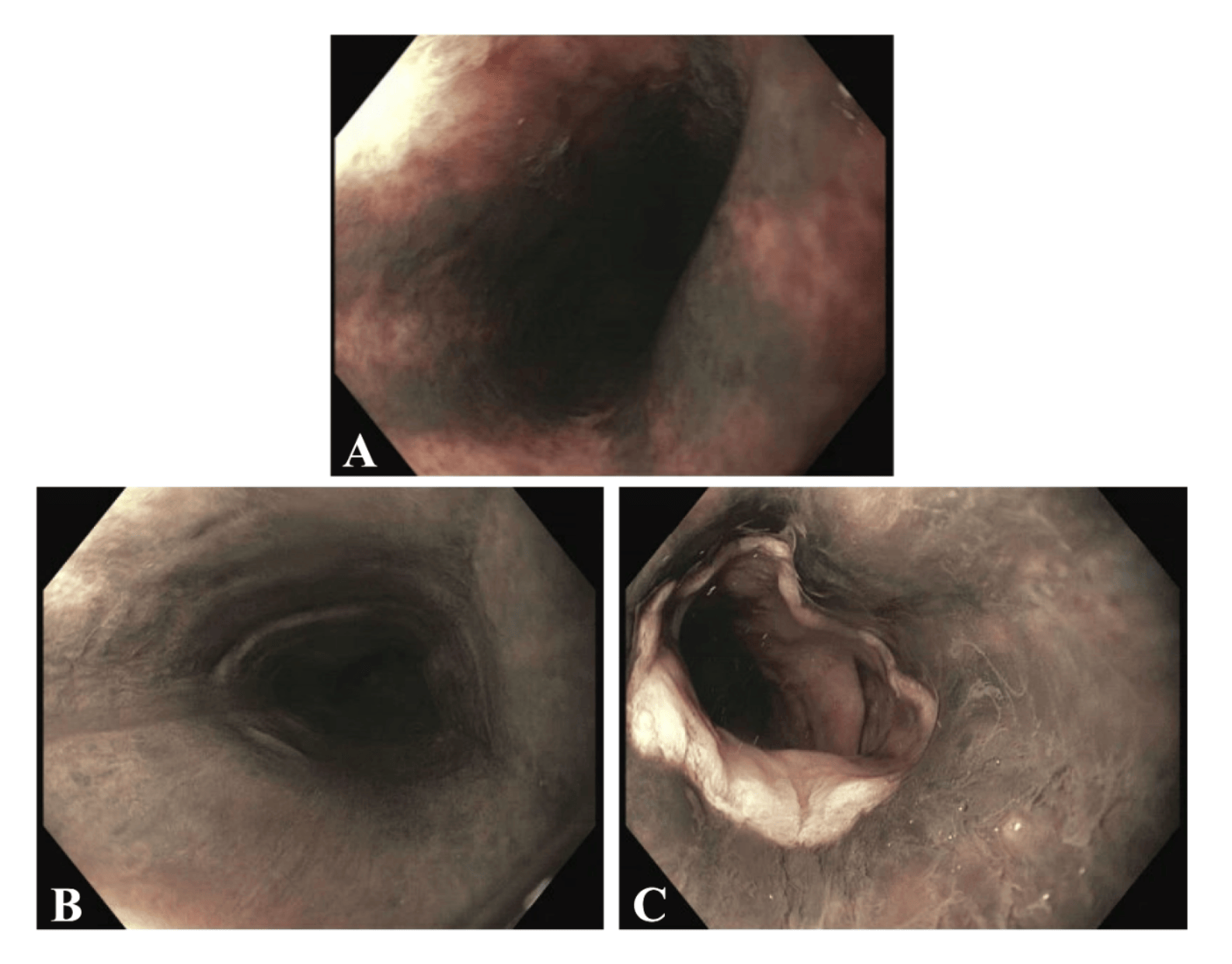
Figure: Figure 1: Initial upper endoscopy showing acute necrotizing esophagitis. A- Upper esophagus. B- Middle esophagus. C- Lower esophagus with sharp transition at the GE junction to normal appearing mucosa distally.
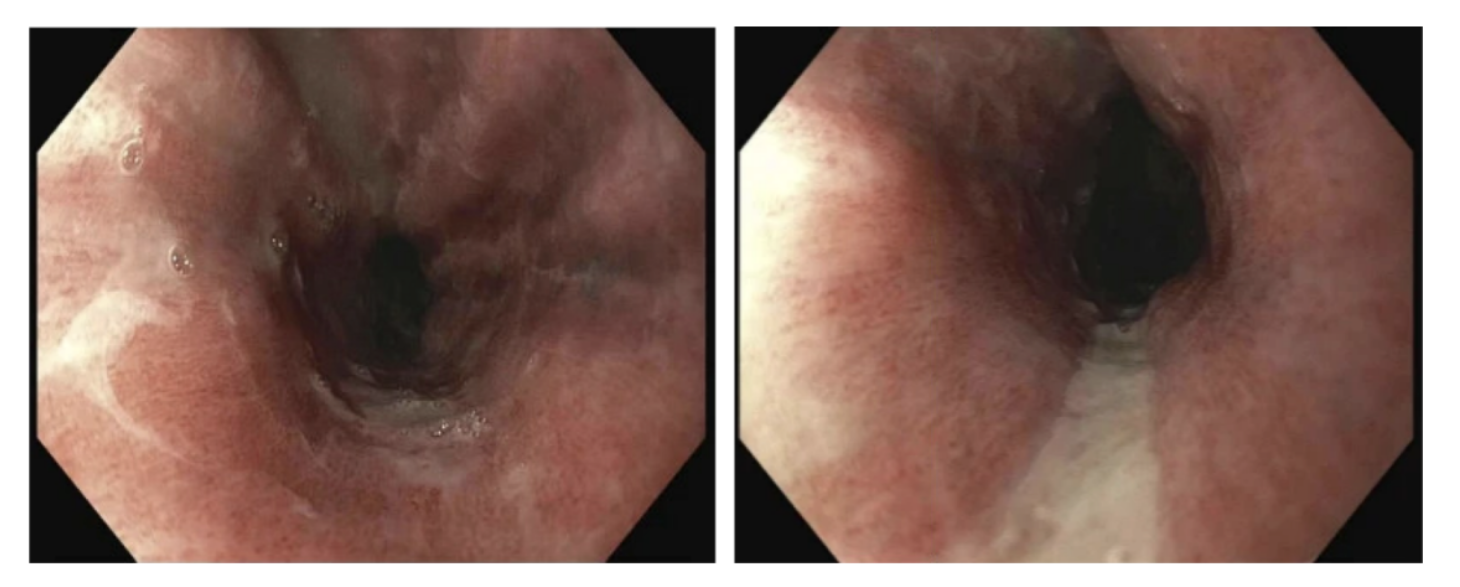
Figure: Figure 2: Follow up upper endoscopy after 2 weeks showing improved mucosa
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Sharifeh Almasaid indicated no relevant financial relationships.
Abdelkader Chaar indicated no relevant financial relationships.
Idan Goren indicated no relevant financial relationships.
Avneet Kaur, MBBS, Sharifeh Almasaid, MD, MPH, Abdelkader Chaar, MD, Idan Goren, MD. P2892 - Acute Esophageal Necrosis: A Rare and Life-Threatening Cause of Acute Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

