Monday Poster Session
Category: Esophagus
P2886 - Boneless but Not Harmless: Endoscopic Closure of Steak-Induced Upper Esophageal Perforation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Woo Suk Kim, DO (he/him/his)
Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai
Queens, NY
Presenting Author(s)
Woo Suk Kim, DO, Bibhuti Adhikari, MD, Genanew Bedanie, MD, Sindhura Kolli, MD, Tasur Seen, MD, Nirali Sheth, DO, Krishna Gurram, MD
Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, Queens, NY
Introduction: Esophageal perforation (EP) is a life-threatening crisis with mortality rates reaching up to 50%. Most cases are iatrogenic, while other etiologies include spontaneous rupture and caustic ingestion. Among foreign body-related injuries, fish bones are most common, accounting for around 12% of cases. Perforations due to boneless food is exceedingly uncommon. Upper EPs pose a distinct challenge for endoscopic stent placement due to the close proximity to the upper esophageal sphincter, increased risk of stent migration, and patient intolerance. Therefore, alternative minimally invasive strategies are crucial - particularly for stable patients with contained perforations where conventional stenting is not viable.
Case Description/
Methods: A 43-year-old male with type 2 diabetes and no smoking history presented with dysphagia and burning chest pain after eating steak, which briefly felt stuck in his throat before passing. He initially tolerated solids but his symptoms worsened over three days, progressing to liquid-only diet. Computed Tomography imaging of neck revealed a 5.8 cm retropharyngeal collection just distal to the upper esophageal sphincter, showing mixed fluid and soft tissue components with local esophageal deviation. Esophagogastroduodenoscopy demonstrated a 3 cm non-bleeding, contained upper EP located 19-22 cm from incisors, with yellow debris but no pus. A pediatric gastroscope was utilized to evaluate and irrigate the cavity with a gentamicin-water solution. PuraStat was then applied to promote mucosal healing. To approximate the edges of the defect, eight hemostatic clips were deployed. A post-procedure Gastrografin esophagram showed no evidence of leakage, and the patient’s diet was gradually advanced.
Discussion: Upper EP presents significant technical limitations for conventional stent placement due to anatomical constraints. This case illustrates that even boneless foods, if swallowed with sufficient force, can cause perforation. It also highlights the viability of a minimally invasive endoscopic approach utilizing PuraStat and hemostatic clips. PuraStat, a self-assembling peptide gel traditionally used for hemostasis, shows promise in promoting mucosal healing and tissue granulation. Furthermore, a pediatric gastroscope was used to distinguish between a mediastinal leak and a contained perforation. This successful case reinforces the evolving role of minimally invasive endoscopic techniques in managing upper EPs, offering an effective alternative to surgery in select patients.
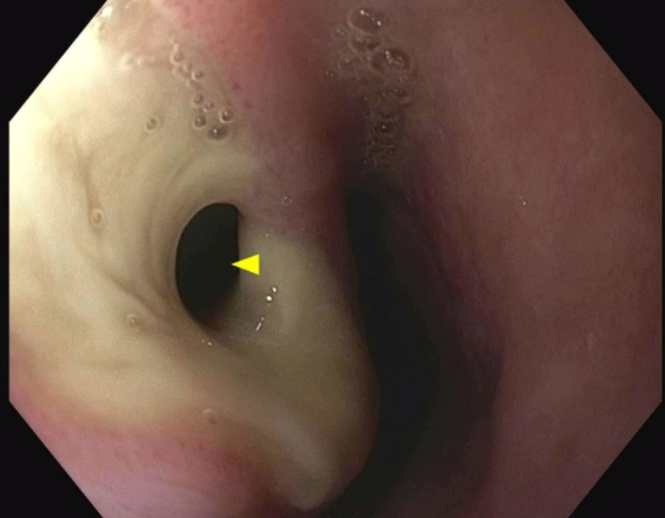
Figure: CT image showing a retropharyngeal collection just distal to the upper esophageal sphincter with local esophageal deviation
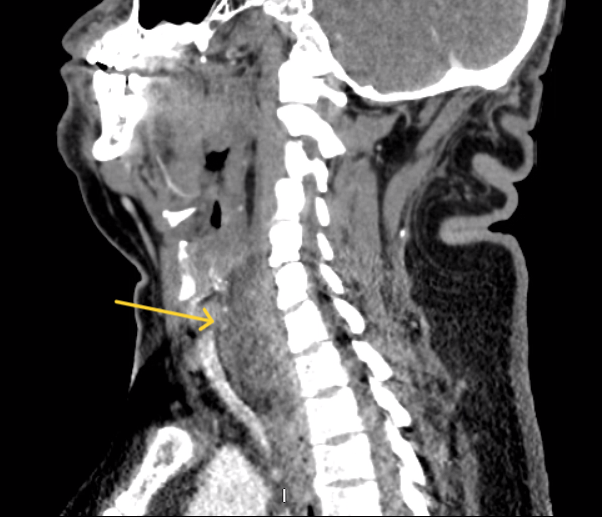
Figure: Endoscopic image of a 3 cm non-bleeding, contained upper esophageal perforation located 19-22 cm from incisors
Disclosures:
Woo Suk Kim indicated no relevant financial relationships.
Bibhuti Adhikari indicated no relevant financial relationships.
Genanew Bedanie indicated no relevant financial relationships.
Sindhura Kolli indicated no relevant financial relationships.
Tasur Seen indicated no relevant financial relationships.
Nirali Sheth indicated no relevant financial relationships.
Krishna Gurram indicated no relevant financial relationships.
Woo Suk Kim, DO, Bibhuti Adhikari, MD, Genanew Bedanie, MD, Sindhura Kolli, MD, Tasur Seen, MD, Nirali Sheth, DO, Krishna Gurram, MD. P2886 - Boneless but Not Harmless: Endoscopic Closure of Steak-Induced Upper Esophageal Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, Queens, NY
Introduction: Esophageal perforation (EP) is a life-threatening crisis with mortality rates reaching up to 50%. Most cases are iatrogenic, while other etiologies include spontaneous rupture and caustic ingestion. Among foreign body-related injuries, fish bones are most common, accounting for around 12% of cases. Perforations due to boneless food is exceedingly uncommon. Upper EPs pose a distinct challenge for endoscopic stent placement due to the close proximity to the upper esophageal sphincter, increased risk of stent migration, and patient intolerance. Therefore, alternative minimally invasive strategies are crucial - particularly for stable patients with contained perforations where conventional stenting is not viable.
Case Description/
Methods: A 43-year-old male with type 2 diabetes and no smoking history presented with dysphagia and burning chest pain after eating steak, which briefly felt stuck in his throat before passing. He initially tolerated solids but his symptoms worsened over three days, progressing to liquid-only diet. Computed Tomography imaging of neck revealed a 5.8 cm retropharyngeal collection just distal to the upper esophageal sphincter, showing mixed fluid and soft tissue components with local esophageal deviation. Esophagogastroduodenoscopy demonstrated a 3 cm non-bleeding, contained upper EP located 19-22 cm from incisors, with yellow debris but no pus. A pediatric gastroscope was utilized to evaluate and irrigate the cavity with a gentamicin-water solution. PuraStat was then applied to promote mucosal healing. To approximate the edges of the defect, eight hemostatic clips were deployed. A post-procedure Gastrografin esophagram showed no evidence of leakage, and the patient’s diet was gradually advanced.
Discussion: Upper EP presents significant technical limitations for conventional stent placement due to anatomical constraints. This case illustrates that even boneless foods, if swallowed with sufficient force, can cause perforation. It also highlights the viability of a minimally invasive endoscopic approach utilizing PuraStat and hemostatic clips. PuraStat, a self-assembling peptide gel traditionally used for hemostasis, shows promise in promoting mucosal healing and tissue granulation. Furthermore, a pediatric gastroscope was used to distinguish between a mediastinal leak and a contained perforation. This successful case reinforces the evolving role of minimally invasive endoscopic techniques in managing upper EPs, offering an effective alternative to surgery in select patients.
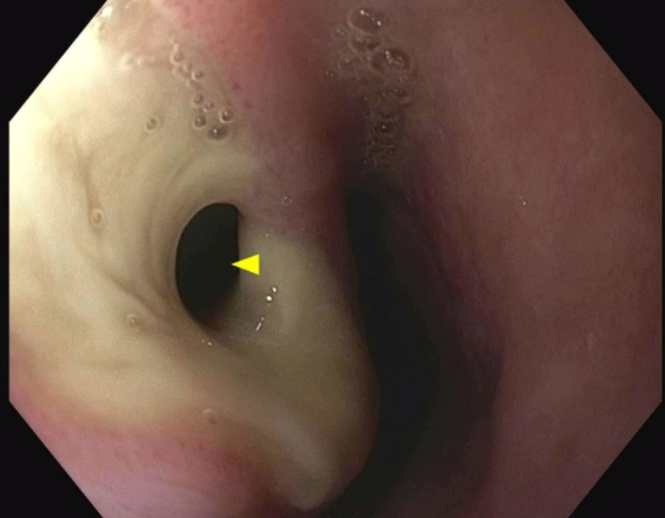
Figure: CT image showing a retropharyngeal collection just distal to the upper esophageal sphincter with local esophageal deviation
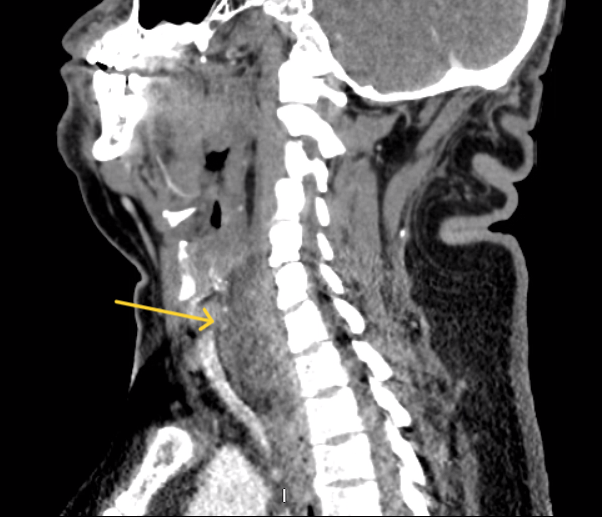
Figure: Endoscopic image of a 3 cm non-bleeding, contained upper esophageal perforation located 19-22 cm from incisors
Disclosures:
Woo Suk Kim indicated no relevant financial relationships.
Bibhuti Adhikari indicated no relevant financial relationships.
Genanew Bedanie indicated no relevant financial relationships.
Sindhura Kolli indicated no relevant financial relationships.
Tasur Seen indicated no relevant financial relationships.
Nirali Sheth indicated no relevant financial relationships.
Krishna Gurram indicated no relevant financial relationships.
Woo Suk Kim, DO, Bibhuti Adhikari, MD, Genanew Bedanie, MD, Sindhura Kolli, MD, Tasur Seen, MD, Nirali Sheth, DO, Krishna Gurram, MD. P2886 - Boneless but Not Harmless: Endoscopic Closure of Steak-Induced Upper Esophageal Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

