Monday Poster Session
Category: Esophagus
P2884 - Esophageal Adenocarcinoma Presenting With Pleural Effusion Due to Esophageal-Pleural Fistula Following Esophageal Stent Displacement: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmed Shukri, MD
Texas Tech University Health Sciences Center
Lubbock, TX
Presenting Author(s)
Ahmed Shukri, MD1, Tarek Shihab, MD1, Reham Majzoub, MD1, Mohamed Shoukrie, BS2, Anuyha Alapati, MD1
1Texas Tech University Health Sciences Center, Lubbock, TX; 2West Texas Digestive disease center, Lubbock, TX
Introduction: Esophageal adenocarcinoma is a life-threatening malignancy with high morbidity and mortality. Though rare, complications such as perforation and fistula formation can be catastrophic, particularly during treatment for advanced disease. Esophageal stenting is frequently used to manage malignant dysphagia but may lead to complications including migration, perforation, and fistula formation. Esophageal-pleural fistulas (EPFs) are particularly severe, as they can cause pleural effusion, empyema, and respiratory failure. We present a case of esophageal adenocarcinoma complicated by an EPF following stent migration, highlighting management challenges.
Case Description/
Methods: An 89-year-old man with esophageal adenocarcinoma and metastatic prostate cancer presented with acute shortness of breath, hypotension, and fever. He had undergone esophageal stenting two months prior for malignant dysphagia. On exam, he had respiratory distress and decreased right-sided breath sounds.
Chest imaging revealed a large right pleural effusion. A chest tube was placed, and fluid analysis confirmed empyema. Notably, pleural fluid amylase was markedly elevated (13,887 U/L). A Gastrografin study (Figure 1) demonstrated stent migration with contrast extravasation into the right hemithorax, confirming an EPF. Due to his frailty and comorbidities, surgery was deemed too high-risk. The stent was repositioned, and he was managed with jejunal feeding and prolonged antibiotics.
Discussion: Esophageal stenting is a palliative measure for malignant dysphagia but carries risks, including stent migration and fistula formation. In this case, stent displacement led to an EPF, empyema, and respiratory compromise. Surgical repair, often needed for such complications, was avoided due to the patient’s poor surgical candidacy. Conservative management with enteral nutrition and antibiotics was pursued.
This case illustrates the need for individualized, multidisciplinary care. Despite his advanced age, shared decision-making guided aggressive medical management. Vigilance for stent-related complications is essential, especially in patients with advanced disease. Early recognition and conservative strategies can improve outcomes in non-surgical candidates.
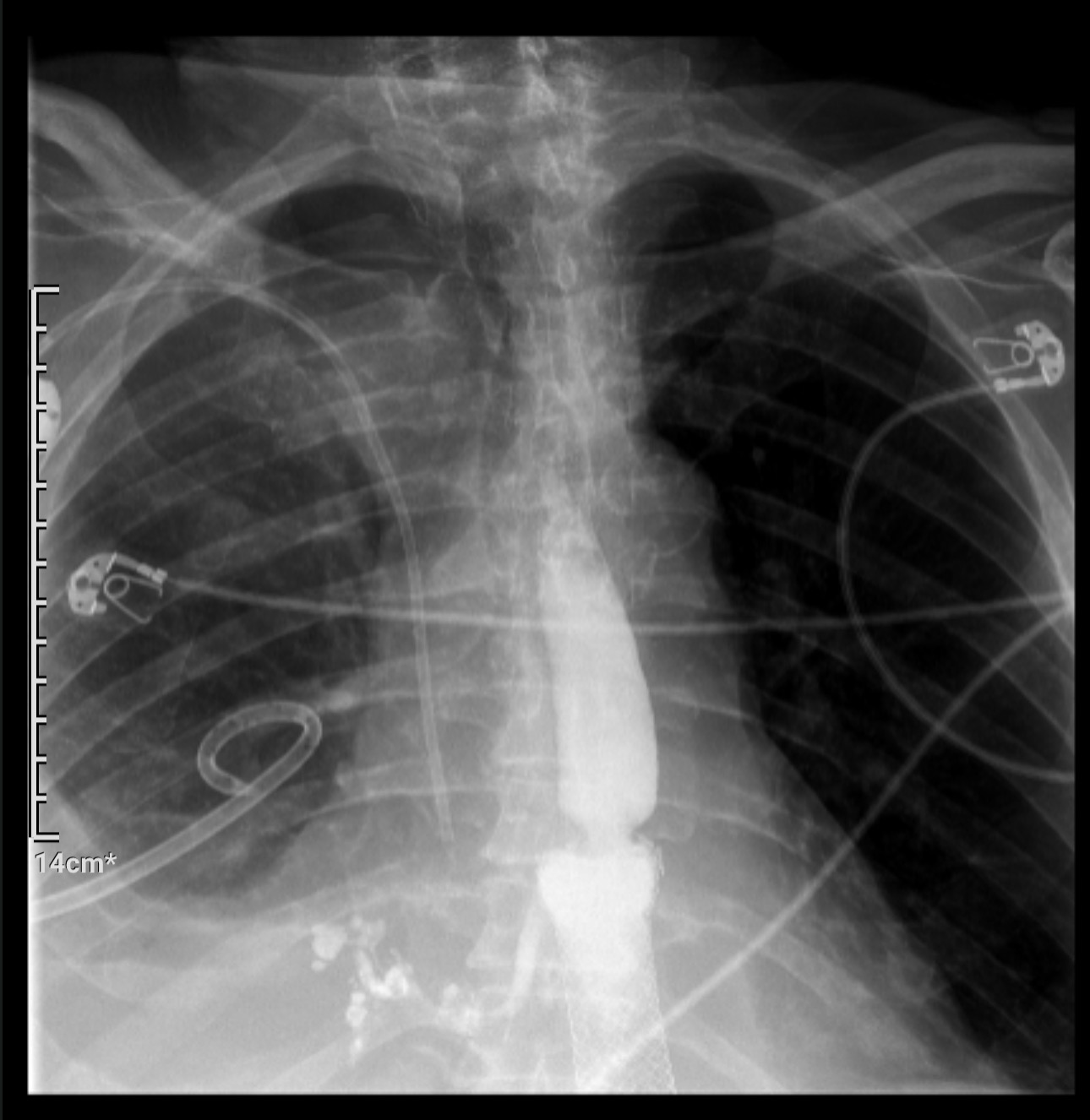
Figure: Figure 1: Gastrografin study demonstrating the esophageal-pleural fistula and associated right-sided pleural effusion.
Disclosures:
Ahmed Shukri indicated no relevant financial relationships.
Tarek Shihab indicated no relevant financial relationships.
Reham Majzoub indicated no relevant financial relationships.
Mohamed Shoukrie indicated no relevant financial relationships.
Anuyha Alapati indicated no relevant financial relationships.
Ahmed Shukri, MD1, Tarek Shihab, MD1, Reham Majzoub, MD1, Mohamed Shoukrie, BS2, Anuyha Alapati, MD1. P2884 - Esophageal Adenocarcinoma Presenting With Pleural Effusion Due to Esophageal-Pleural Fistula Following Esophageal Stent Displacement: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, Lubbock, TX; 2West Texas Digestive disease center, Lubbock, TX
Introduction: Esophageal adenocarcinoma is a life-threatening malignancy with high morbidity and mortality. Though rare, complications such as perforation and fistula formation can be catastrophic, particularly during treatment for advanced disease. Esophageal stenting is frequently used to manage malignant dysphagia but may lead to complications including migration, perforation, and fistula formation. Esophageal-pleural fistulas (EPFs) are particularly severe, as they can cause pleural effusion, empyema, and respiratory failure. We present a case of esophageal adenocarcinoma complicated by an EPF following stent migration, highlighting management challenges.
Case Description/
Methods: An 89-year-old man with esophageal adenocarcinoma and metastatic prostate cancer presented with acute shortness of breath, hypotension, and fever. He had undergone esophageal stenting two months prior for malignant dysphagia. On exam, he had respiratory distress and decreased right-sided breath sounds.
Chest imaging revealed a large right pleural effusion. A chest tube was placed, and fluid analysis confirmed empyema. Notably, pleural fluid amylase was markedly elevated (13,887 U/L). A Gastrografin study (Figure 1) demonstrated stent migration with contrast extravasation into the right hemithorax, confirming an EPF. Due to his frailty and comorbidities, surgery was deemed too high-risk. The stent was repositioned, and he was managed with jejunal feeding and prolonged antibiotics.
Discussion: Esophageal stenting is a palliative measure for malignant dysphagia but carries risks, including stent migration and fistula formation. In this case, stent displacement led to an EPF, empyema, and respiratory compromise. Surgical repair, often needed for such complications, was avoided due to the patient’s poor surgical candidacy. Conservative management with enteral nutrition and antibiotics was pursued.
This case illustrates the need for individualized, multidisciplinary care. Despite his advanced age, shared decision-making guided aggressive medical management. Vigilance for stent-related complications is essential, especially in patients with advanced disease. Early recognition and conservative strategies can improve outcomes in non-surgical candidates.
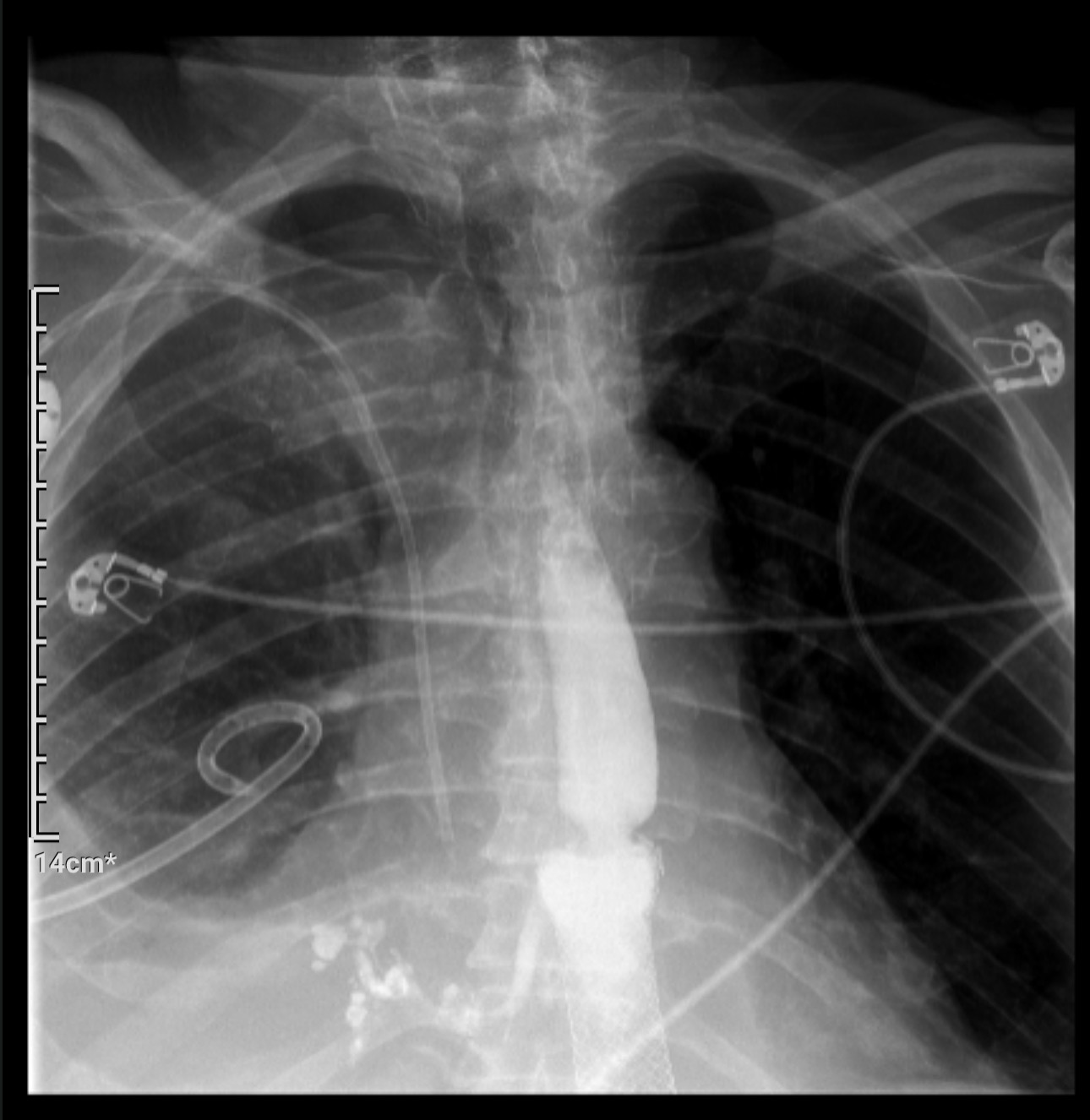
Figure: Figure 1: Gastrografin study demonstrating the esophageal-pleural fistula and associated right-sided pleural effusion.
Disclosures:
Ahmed Shukri indicated no relevant financial relationships.
Tarek Shihab indicated no relevant financial relationships.
Reham Majzoub indicated no relevant financial relationships.
Mohamed Shoukrie indicated no relevant financial relationships.
Anuyha Alapati indicated no relevant financial relationships.
Ahmed Shukri, MD1, Tarek Shihab, MD1, Reham Majzoub, MD1, Mohamed Shoukrie, BS2, Anuyha Alapati, MD1. P2884 - Esophageal Adenocarcinoma Presenting With Pleural Effusion Due to Esophageal-Pleural Fistula Following Esophageal Stent Displacement: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
