Monday Poster Session
Category: General Endoscopy
P2974 - Impact of IV Fluid Shortage on Outcomes of Endoscopic Procedures: A Nationwide Propensity-Matched Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Shivam Kalra, MBBS, MHA2, Angad Mann, MD3, Saranya Arumugam, MD1, Manan Trivedi, MD4, Banreet Dhindsa, MD5, Amaninder Dhaliwal, MD6
1University of California Riverside School of Medicine, Riverside, CA; 2Trident Medical Center, North Charleston, SC; 3University of California Riverside School of Medicine, Rancho Cucamonga, CA; 4University of California Riverside School of Medicine, Redlands, CA; 5Brown University / Rhode Island Hospital, East Providence, RI; 6University of South Carolina School of Medicine, Florence, SC
Introduction: Intravenous (IV) fluids are thought to be essential during endoscopic procedures for maintaining hemodynamic stability and managing complications. However, in late 2024, the U.S. experienced a shortage of IV fluids, raising concerns regarding procedural safety and patient outcomes. This study aims to account for the impact of this IV fluid shortage on peri-procedural outcomes in patients undergoing endoscopic procedures.
Methods: We conducted a retrospective cohort study using the TriNetX US Collaborative Network, encompassing 66 healthcare organizations. Patients aged 18–80 undergoing EGD or colonoscopy between Feb 1–Sep 30, 2024 (pre-shortage), were compared to those between Oct 1, 2024- May 31, 2025 (post-shortage). Propensity score matching (1:1) was performed on demographics and comorbidities, yielding 435,536 patients in each group. Outcomes included IV fluid administration, hypotension, shock, and postprocedural bleeding.
Results: IV fluid use was significantly reduced post-shortage (24.5% vs. 17.7%, p< 0.001). Despite reduced fluid administration, the risk of shock (0.8% vs. 0.6%), hypotension (2.0% vs. 1.4%), and postprocedural bleeding (7.8% vs. 7.1%) were all significantly lower post-shortage (p< 0.001 for all). Hazard ratios for these outcomes similarly indicated reduced risk post-shortage. Median survival was not reached for any outcome, indicating low event rates.
Discussion: The nationwide IV fluid shortage was associated with reduced IV fluid use during endoscopic procedures but paradoxically correlated with lower rates of hypotension, shock, and bleeding. These findings may reflect more judicious fluid use, altered perioperative practices, or other system-level adaptations during the shortage period and, by extension, underscore the unnecessary periprocedural overuse of IV fluid in a non-shortage period. Further studies are warranted to guide the peri-endoscopic use of IV fluids and avoid overuse without impacting patient care.
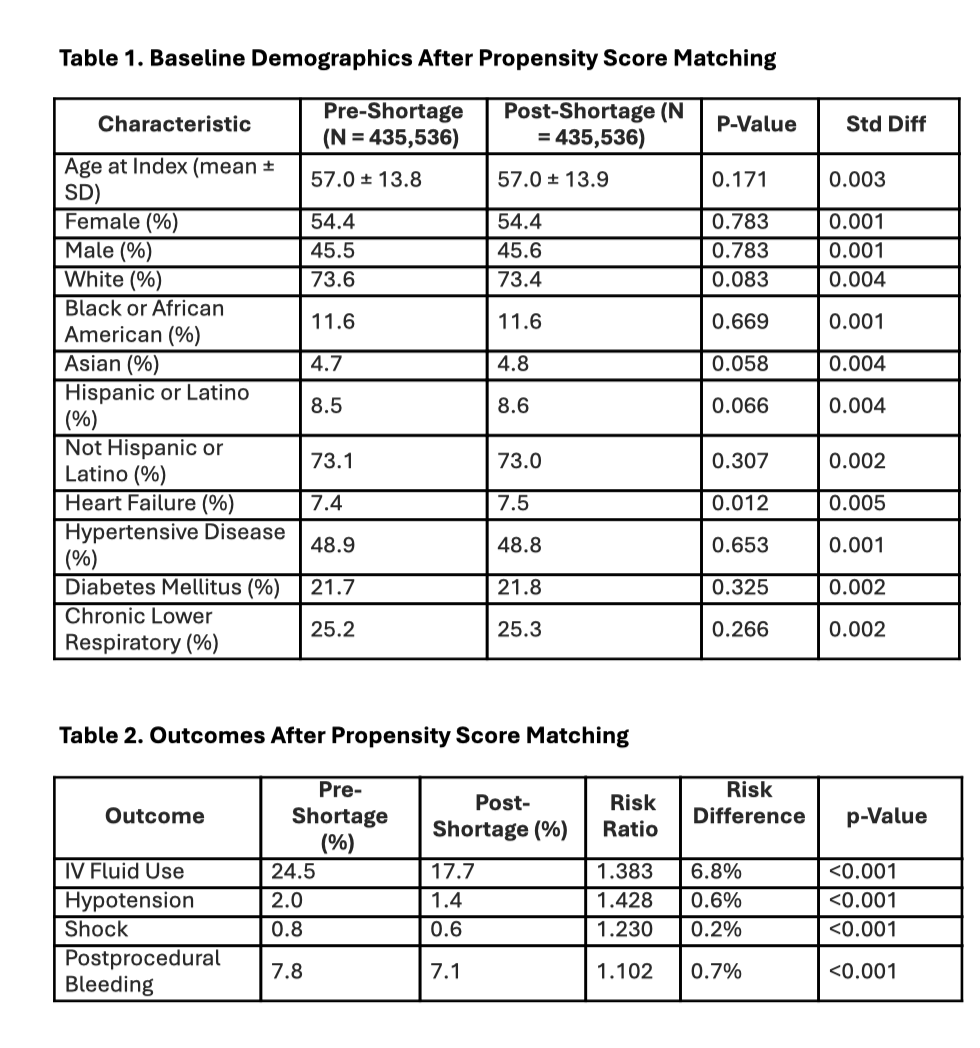
Figure: Figure depicting the comparative outcomes between pre- and post IV fluid shortage groups
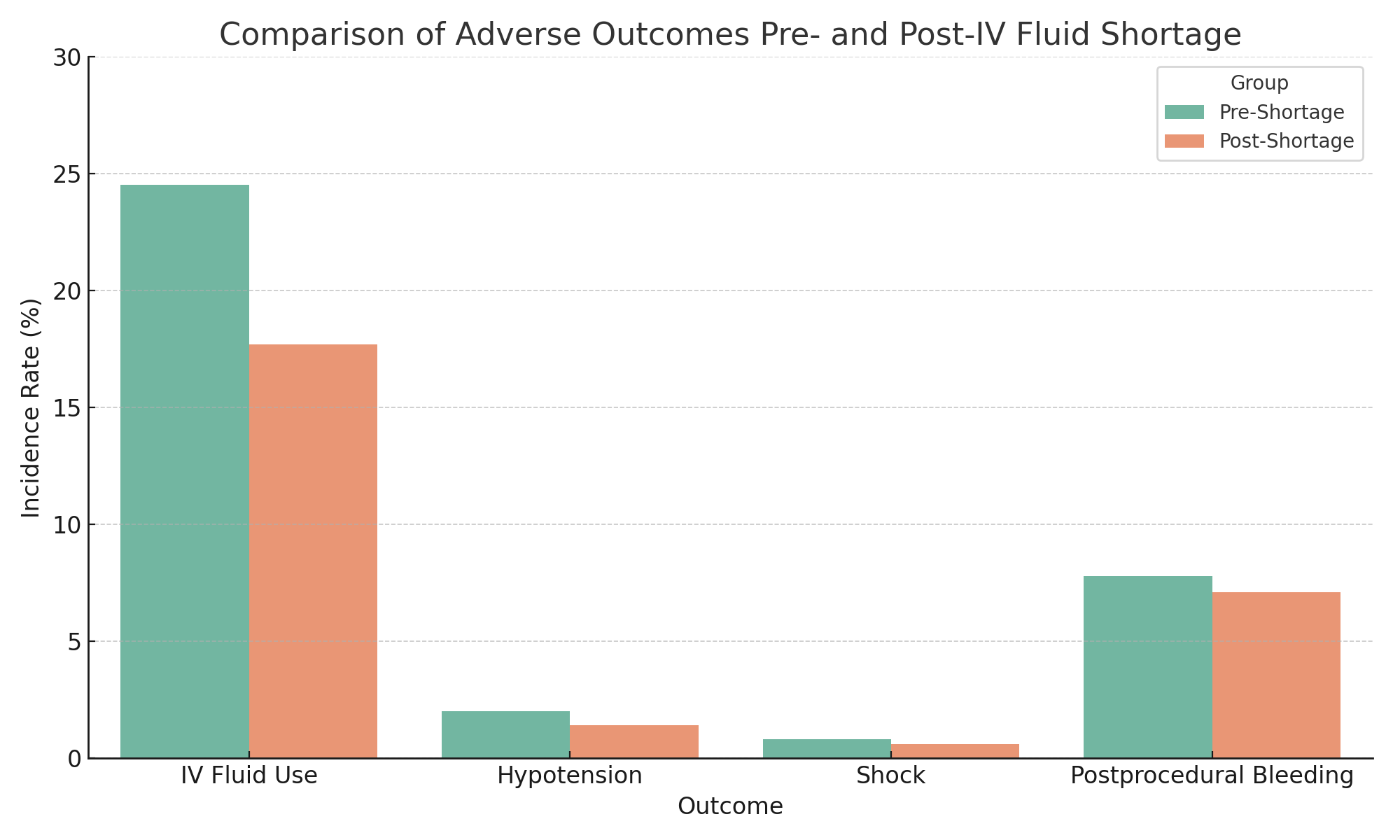
Figure: Table 1: Baseline demographics after propensity score matching
Table 2: Outcomes after propensity score matching
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Shivam Kalra indicated no relevant financial relationships.
Angad Mann indicated no relevant financial relationships.
Saranya Arumugam indicated no relevant financial relationships.
Manan Trivedi indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Amaninder Dhaliwal indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Shivam Kalra, MBBS, MHA2, Angad Mann, MD3, Saranya Arumugam, MD1, Manan Trivedi, MD4, Banreet Dhindsa, MD5, Amaninder Dhaliwal, MD6. P2974 - Impact of IV Fluid Shortage on Outcomes of Endoscopic Procedures: A Nationwide Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Trident Medical Center, North Charleston, SC; 3University of California Riverside School of Medicine, Rancho Cucamonga, CA; 4University of California Riverside School of Medicine, Redlands, CA; 5Brown University / Rhode Island Hospital, East Providence, RI; 6University of South Carolina School of Medicine, Florence, SC
Introduction: Intravenous (IV) fluids are thought to be essential during endoscopic procedures for maintaining hemodynamic stability and managing complications. However, in late 2024, the U.S. experienced a shortage of IV fluids, raising concerns regarding procedural safety and patient outcomes. This study aims to account for the impact of this IV fluid shortage on peri-procedural outcomes in patients undergoing endoscopic procedures.
Methods: We conducted a retrospective cohort study using the TriNetX US Collaborative Network, encompassing 66 healthcare organizations. Patients aged 18–80 undergoing EGD or colonoscopy between Feb 1–Sep 30, 2024 (pre-shortage), were compared to those between Oct 1, 2024- May 31, 2025 (post-shortage). Propensity score matching (1:1) was performed on demographics and comorbidities, yielding 435,536 patients in each group. Outcomes included IV fluid administration, hypotension, shock, and postprocedural bleeding.
Results: IV fluid use was significantly reduced post-shortage (24.5% vs. 17.7%, p< 0.001). Despite reduced fluid administration, the risk of shock (0.8% vs. 0.6%), hypotension (2.0% vs. 1.4%), and postprocedural bleeding (7.8% vs. 7.1%) were all significantly lower post-shortage (p< 0.001 for all). Hazard ratios for these outcomes similarly indicated reduced risk post-shortage. Median survival was not reached for any outcome, indicating low event rates.
Discussion: The nationwide IV fluid shortage was associated with reduced IV fluid use during endoscopic procedures but paradoxically correlated with lower rates of hypotension, shock, and bleeding. These findings may reflect more judicious fluid use, altered perioperative practices, or other system-level adaptations during the shortage period and, by extension, underscore the unnecessary periprocedural overuse of IV fluid in a non-shortage period. Further studies are warranted to guide the peri-endoscopic use of IV fluids and avoid overuse without impacting patient care.
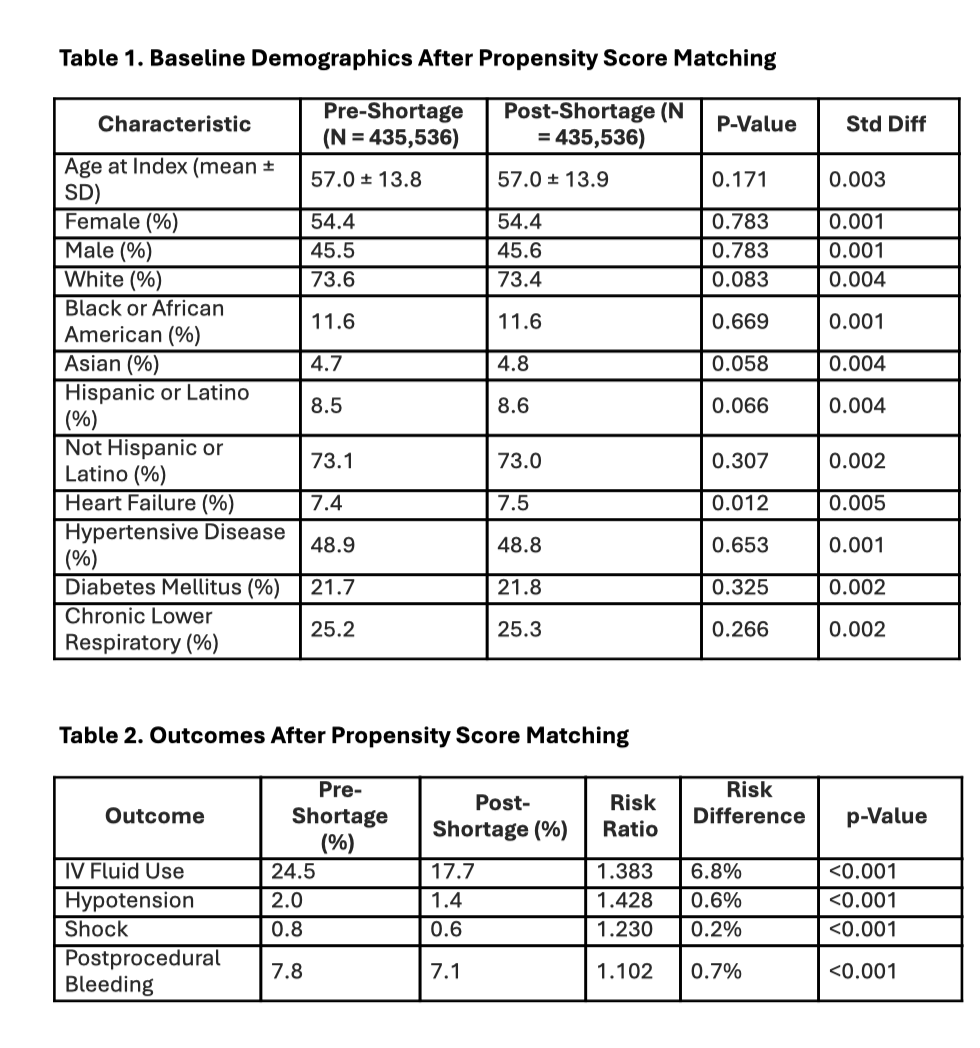
Figure: Figure depicting the comparative outcomes between pre- and post IV fluid shortage groups
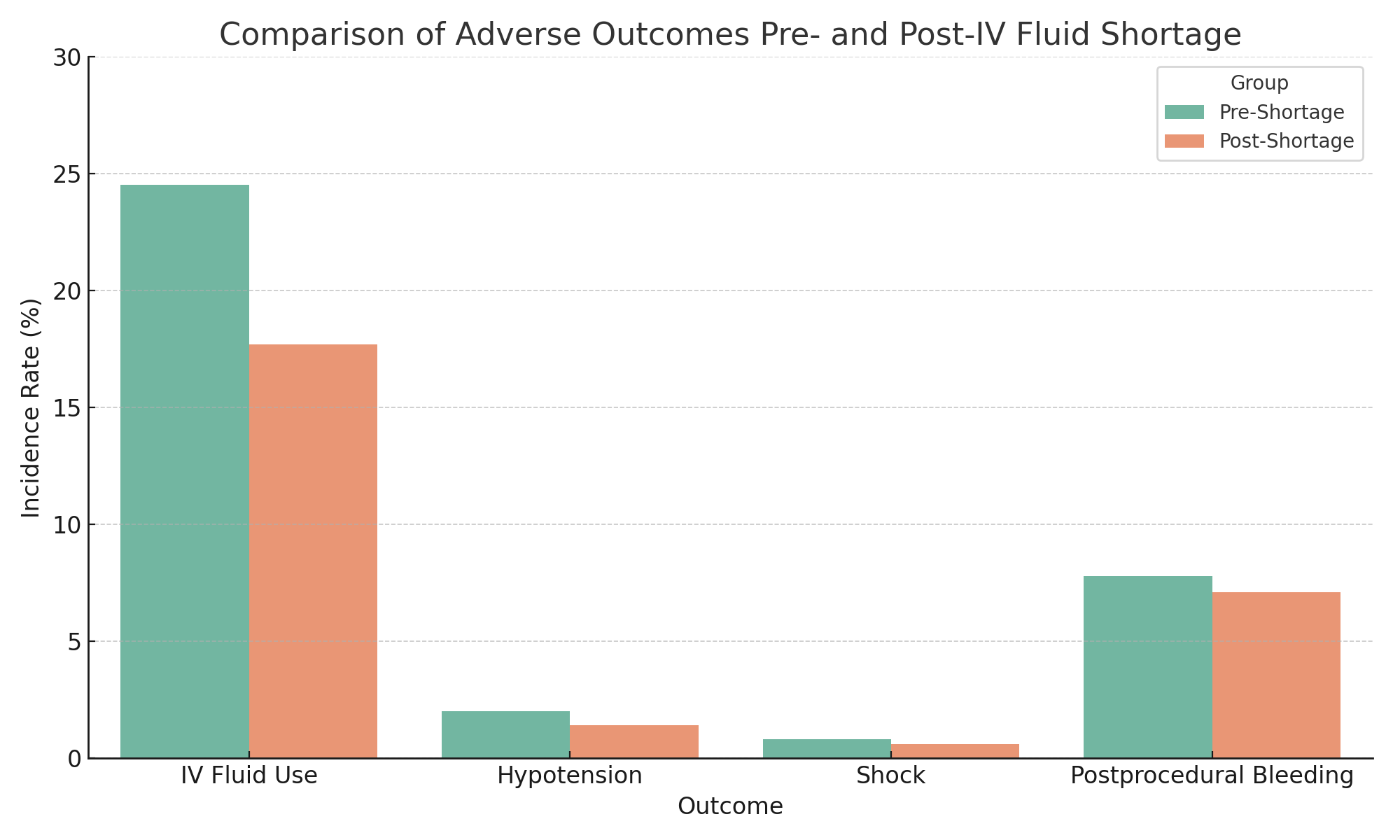
Figure: Table 1: Baseline demographics after propensity score matching
Table 2: Outcomes after propensity score matching
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Shivam Kalra indicated no relevant financial relationships.
Angad Mann indicated no relevant financial relationships.
Saranya Arumugam indicated no relevant financial relationships.
Manan Trivedi indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Amaninder Dhaliwal indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Shivam Kalra, MBBS, MHA2, Angad Mann, MD3, Saranya Arumugam, MD1, Manan Trivedi, MD4, Banreet Dhindsa, MD5, Amaninder Dhaliwal, MD6. P2974 - Impact of IV Fluid Shortage on Outcomes of Endoscopic Procedures: A Nationwide Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
